Abstract
Purpose
To determine if central sympathetic blockade by dexmedetomidine, a selective alpha2 adrenergic receptor agonist, prevents cardiac dysfunction associated with intracranial hypertension (ICH) in a rat model.
Methods
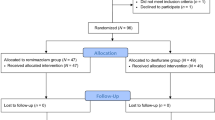
Following intracisternal administration of dexmedetomidine (1 μg · μl−1, 10 μL volume) or the stereoisomer levomedetomidine (1 μg· μL−1, 10 μL volume) in halothane-anesthetized rats, a subdural balloon catheter was inflated for 60 sec to produce ICH. Intracranial pressure, hemodynamic, left ventricular (LV) pressures and electrocardiographic (ECG) changes were recorded. Plasma and myocardial catecholamines and malondialdehyde (MDA) levels were measured.
Results
After levomedetomidine administration, subdural balloon inflation precipitated an increase in mean arterial pressure (149 ± 33% of baseline), heart rate (122 ± 19% of baseline), LV systolic pressure (LVP), LV end-diastolic pressure (LVEDP), LV developed pressure (LVDP), LV dP/dtmax and rate pressure product (RPP) (132 ± 19%, 260 ± 142%, 119 ± 15%, 126 ± 24% and 146 ± 33% of baseline value, respectively). ICH decelerated LVP fall (τ), as t increased from 7.75 ± 1. 1 to 14.37 ± 4.5 msec. Moreover, plasma norepinephrine levels were elevated ( 169 ± 50% of baseline) and there was the appearance of cardiac dysrhythmias and other ECG abnormalities. This response was transient and cardiac function deteriorated in a temporal manner. Intracisternal dexmedetomidine prevented the rise in plasma norepinephrine, blocked the ECG abnormalities, and preserved cardiac function. Moreover, dexmedetomidine attenuated the rise in MDA levels.
Conclusions
The results demonstrate that dexmedetomidine attenuates cardiac dysfunction associated with ICH. Our results provide evidence for the role of central sympathetic hyperactivity in the development of cardiac dysfunction associated with ICH.
Résumé
Objectif
Déterminer si !e biocage sympathique central par ia dexmédétomidine, un agoniste sélectif des récepteurs alpha2 adrénergiques, prévient ia dysfonction cardiaque associée à l’hypertension intracrânienne (HIC) chez un modèle rat.
Méthode
Après l’administration intradstemale de dexmédétomidine (1 μg · μL−1, volume de 10μL) ou du stéréoisomère lévomédétomidine (1 μg · μL−1, volume de 10 μL) chez des rats anesthésiés à l’halothane, un cathéter sous-dural à ballonnet a été gonflé pendant 60 s pour produire une HIC. La pression intracrânienne, l’hémodynamique, les pressions ventriculaires gauches (VG) et les changements électrocardiographiques (ECG) ont été enregistrés. Les niveaux plasmatiques et myocardiques de catécholamines et de malondialdéhyde (MDA) ont été mesurés.
Résultats
Après l’administration de lévomédétomidine, le gonflement du ballonnet sous-dural a précipité une hausse de la tension artérielle moyenne (149 ± 33 % des mesures de base), de la fréquence cardiaque (122 ± 19 % de la base), la tension systolique VG (TVG), la tension télédiastolique VG (TTDVG), la tension développée du VG (TDVG), dP/dtmax VG et le produit tension-fréquence cardiaque PJF (132 ± 19%, 260 ± 142 %, 119 ± 15 %, 126 ± 24% et 146 ± 33% des valeurs de base, respectivement). L’HIC a décéléré la chute de la TVG (τ), à mesure que t augmentait de 7,75 ± 1,1 à 14,37 ± 4,5 msec. De plus, les niveaux plasmatiques de norépinéphrine étaient élevés (169 ± 50 % de la base) et des dysrythmies cardiaques sont apparues avec d’autres anomalies ECG. La réaction a été une détérioration transitoire de la fonction cardiaque d’une manière temporelle. La dexmédétomidine intracisternale a empêché l’élévation de norépinéphrine plasmatique, bloqué les anomalies ECG et préservé la fonction cardiaque. La dexmédétomidine a diminué la hausse des niveaux de MDA.
Conclusion
Les résultats démontrent que la dexmédétomidine atténue la dysfonction cardiaque associée à HIC. Ils mettent en évidence le rôle de l’hyperactivité sympathique centrale dans le développement de dysfonction cardiaque associée à l’HIC.
Similar content being viewed by others
References
DujarMn KS, McCully RB, Wijdicks EF, et al. Myocardial dysfunction associated with brain death: clinical, echocardiographic, and pathologic features. J Heart Lung Transplant 2001; 20: 350–7.
Huttemann E, Schelenz C, Chatzinikolaou K, Reinhart K. Left ventricular dysfunction in lethal severe brain injury: impact of transesophageal echocardiography on patient management. Intensive Care Med 2002; 28: 1084–8.
Bratton SL, Davis RL. Acute lung injury in isolated traumatic brain injury. Neurosurgery 1997; 40: 707–12.
Gilbert EM, Krueger SK, Murray JL, et al. Echocardiographic evaluation of potential cardiac transplant donors. J Thorac Cardiovasc Surg 1988; 95: 1003–7.
Busson M, N’Doye P, Benoit G, et al. Donor factors influencing organ transplant prognosis. Transplant Proc 1995; 27: 1662–4.
Nygaard CE, Townsend RN, Diamond DL. Organ donor management and organ outcome: a 6-year review from a level I trauma center. J Trauma 1990; 30: 728–32.
Tsai FC, Marelli D, Bresson J, et al. Use of hearts transplanted from donors with atraumatic intracranial bleeds. J Heart Lung Transplant 2002; 21: 623–8.
Novitzky D, Wicomb WN, Cooper DK, Rose AG, Fraser RC, Barnard CN. Electrocardiographic, hemodynamic and endocrine changes occuring during experimental brain death in the Chacma baboon. Heart Transplant 1984; 4: 63–9.
Shanlin RJ, Sole MJ, Rahimifar M, Tator CH, Factor SM. Increased intracranial pressure elicits hypertension, increased sympathetic activity, electrocardiographic abnormalities and myocardial damage in rats. J Am Coll Cardiol 1988; 12: 727–36.
Graf CJ, Rossi NP. Catecholamine response to intracranial hypertension. J Neurosurg 1978; 49: 862–8.
Novitzky D, Rhodin J, Cooper DK, Te T, Min KW, DeBault L. Ultrastructure changes associated with brain death in the human donor heart. Transpl Int 1997; 10: 24–32.
Novitzky D, Wicomb WN, Cooper DK, Rose AG, Reichart B. Prevention of myocardial injury during brain death by total cardiac sympathectomy in the Chacma baboon. Ann Thorac Surg 1986; 41: 520–4.
Shivalkar B, Van Loon J, Wieland W, et al. Variable effects of explosive or gradual increase of intracranial pressure on myocardial structure and function. Circulation 1993; 87: 230–9.
White M, Wiechmann RJ, Roden RL, et al. Cardiac ß- adrenergic neuroeffector systems in acute myocardial dysfunction related to brain injury. Evidence for catecholamine-mediated myocardial damage. Circulation 1995; 92: 2183–9.
Rona G. Catecholamine cardiotoxicity (Editorial). J Mol Cell Cardiol 1985; 17: 291–306.
Dampney RA, Kumada M, Reis DJ. Central neural mechanisms of the cerebral ischemic response. Characterization, effect of brainstem and cranial nerve transections, and simulation by electrical stimulation of restricted regions of medulla oblongata in rabbit. Circ Res 1979; 44: 48–62.
Dampney RA, Moon FA. Role of ventrolateral medulla in vasomotor response to cerebral ischemia. Am J Physiol 1980; 239: H349–58.
Hong M, Milne B, Loomis C, Jhamandas K. Stereoselective effects of central α2-adrenergic agonist medetomidine on in vivo catechol activity in the rat rostral ventrolateral medulla (RVLM). Brain Res 1992; 592: 163–9.
Punnen S, Urbanski R, Krieger AJ, Sapru HN. Ventrolateral medullary pressor area: site of hypotensive action of clonidine. Brain Res 1987; 422: 336–46.
Cruickshank JM, Neil-Dwyer G, Degaute JP, et al. Reduction of stress/catecholamine-induced cardiac necrosis by beta1 — selective blockade. Lancet 1987; 2: 585–9.
Hunt D, Gore I. Myocardial lesions following experimental intracranial hemorrhage: prevention with propranolol. Am Heart J 1972; 83: 232–6.
Hall SR, Wang L, Milne B, Ford S, Hong M. Intrathecal lidocaine prevents cardiovascular collapse and neurogenic pulmonary edema in a rat model of acute intracranial hypertension. Anesth Analg 2002; 94: 948–53.
Farber NE, Samso E, Staunton M, Schwabe D, Schmeling WT. Dexmedetomidine modulates cardiovascular responses to stimulation of central nervous system pressor sites. Anesth Analg 1999; 88: 617–24.
Adler D, Nikolic SD, Sonnenblick EH, Tellin EL. Time to dP/dtmax, a preload-independent index of contractility: open-chest dog study. Basic Res Cardiol 1996; 91: 94–100.
Weiss JL, Frederiksen JW, Weisfeldt ML. Hemodynamic determinants of the time-course of fall in canine left ventricular pressure. J Clin Invest 1976; 58: 751–60.
Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol 1978; 52: 302–10.
Clifton GL, Robertson CS, Kyper K, Taylor AA, Dhekne RD, Grossman RG. Cardiovascular response to severe head injury. J Neurosurg 1983; 59: 447–54.
Powner DJ, Hendrich A, Nyhuis A, Strate R. Changes in serum catecholamine levels in patients who are brain dead. J Heart Lung Transplant 1992; 11: 1046–53.
Herijgers P, Leunens V, Tjandra-Maga TB, Mubagwa K, Flameng W. Changes in organ perfusion after brain death in the rat and its relation to circulating catecholamines. Transplantation 1996; 62: 330–5.
Di Pasquale G, Pinelli G, Andreoli A, Manini G, Grazi P, Tognetti F. Holter detection of cardiac arrhythmias in intracranial subarachnoid hemorrhage. Am J Cardiol 1987; 59: 596–600.
Yamour BJ, Sridharan MR, Rice JF, Flowers NC. Electrocardiographic changes in cerebrovascular hemorrhage. Am Heart J 1980; 99: 294–300.
Gutteridge JM, Halliwell B. The measurement and mechanism of lipid peroxidation in biological systems. Trends Biochem Sci 1990; 15: 129–35.
Folden DV, Gupta A, Sharma AC, Li SY, Saari JT, Ren J. Malondialdehyde inhibits cardiac contractile function in ventricular myocytes via a p38 mitogen-activated protein kinase-dependent mechanism. Br J Pharmacol 2003; 139: 1310–6.
Dhalla NS, Temsah RM, Netticadan T. Role of oxidative stress in cardiovascular diseases. J Hypertens 2000; 18: 655–73.
Rupp H, Dhalla KS, Dhalla NS. Mechanisms of cardiac cell damage due to catecholamines: significance of drugs regulating central sympathetic outflow. J Cardiovasc Pharmacol 1994; 24(Suppl 1): S16–24.
Hori M, Gotoh K, Kitakaze M, et al. Role of oxygenderived free radicals in myocardial edema and ischemia in coronary microvascular embolization. Circulation 1991; 84: 828–40.
Kaneko M, Beamish RE, Dhalla NS. Depression of heart sarcolemmal Ca2+-pump activity by oxygen free radicals. Am J Physiol 1989; 256: H368–74.
Kaneko M, Elimban V, Dhalla NS. Mechanism for depression of heart sarcolemmal Ca2+ pump by oxygen free radicals. Am J Physiol 1989; 257: H804–11.
Tappia PS, Hata T, Hozaima L, Sandhu MS, Panagia V, Dhalla NS. Role of oxidative stress in catecholamine-induced changes in cardiac sarcolemmal Ca2+ transport. Arch Biochem Biophys 2001; 387: 85–92.
Author information
Authors and Affiliations
Corresponding author
Additional information
Preliminary results of this study were previously presented at the 49th Annual Canadian Anesthesiologists’ Society (CAS) Meeting, June 1, 2002, Victoria, British Columbia, Canada.
Rights and permissions
About this article
Cite this article
Hall, S.R.R., Wang, L., Milne, B. et al. Central dexmedetomidine attenuates cardiac dysfunction in a rodent model of intracranial hypertension. Can J Anesth 51, 1025–1033 (2004). https://doi.org/10.1007/BF03018493
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03018493