Abstract
Purpose
The aim was to evaluate stereotactic body radiation therapy (SBRT) treatment planning variability for early stage nonsmall cell lung cancer (NSCLC) with respect to the published guidelines of the Stereotactic Radiotherapy Working Group of the German Society for Radiation Oncology (DEGRO).
Materials and methods
Planning computed tomography (CT) scan and the structure sets (planning target volume, PTV; organs at risk, OARs) of 3 patients with early stage NSCLC were sent to 22 radiotherapy departments with SBRT experience: each department was asked to prepare a treatment plan according to the DEGRO guidelines. The prescription dose was 3 fractions of 15 Gy to the 65% isodose.
Results
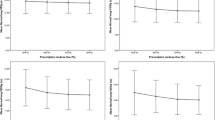
In all, 87 plans were generated: 36 used intensity-modulated arc therapy (IMAT), 21 used three-dimensional conformal radiation therapy (3DCRT), 6 used static field intensity-modulated radiation therapy (SF-IMRT), 9 used helical radiotherapy and 15 used robotic radiosurgery. PTV dose coverage and simultaneously kept OARs doses were within the clinical limits published in the DEGRO guidelines. However, mean PTV dose (mean 58.0 Gy, range 52.8–66.4 Gy) and dose conformity indices (mean 0.75, range 0.60–1.00) varied between institutions and techniques (p ≤ 0.02). OARs doses varied substantially between institutions, but appeared to be technique independent (p = 0.21).
Conclusion
All studied treatment techniques are well suited for SBRT of early stage NSCLC according to the DEGRO guidelines. Homogenization of SBRT practice in Germany is possible through the guidelines; however, detailed treatment plan characteristics varied between techniques and institutions and further homogenization is warranted in future studies and recommendations. Optimized treatment planning should always follow the ALARA (as low as reasonably achievable) principle.
Zusammenfassung
Hintergrund
Ziel war die Untersuchung der Variabilität der Bestrahlungsplanung der stereotaktischen Strahlentherapie (SBRT) für das nicht-kleinzellige Bronchialkarzinom (NSCLC) im Frühstadium in Bezug auf die veröffentlichten Empfehlungen der Arbeitsgemeinschaft Stereotaxie der Deutschen Gesellschaft für Radioonkologie (DEGRO).
Material und Methoden
Planungscomputertomographie und Strukturdatensätze (Planungszielvolumen, PTV; Risikoorgane, OARs) von 3 NSCLC-Patienten im Frühstadium wurden an 22 Strahlentherapieabteilungen mit SBRT-Erfahrung gesendet: Jede Abteilung sollte einen Behandlungsplan nach DEGRO-Richtlinie generieren. Die Verschreibungsdosis betrug 3 Fraktionen mit je 15 Gy auf die 65%-Isodose.
Ergebnisse
Es wurden 87 Pläne erzeugt: 36 mit intensitätsmodulierter Arc-Therapie (IMAT), 21 mit dreidimensionaler konformaler Strahlentherapie (3D-CRT), 6 mit intensitätsmodulierte Radiotherapie mit statischen Feldern (SF-IMRT), 9 mit helikaler Strahlentherapie und 15 mit robotergestützter Radiochirurgie. PTV-Dosisabdeckung und alle gleichzeitig erfassten OAR-Dosen hielten sich an die klinischen Grenzwerte der DEGRO-Richtlinie. Dennoch variierten durchschnittliche PTV-Dosen (Mittelwert 58,0 Gy; Spanne 52,8–66,4 Gy) und Dosiskonformitätsindizes (Mittelwert 0,75; Spanne 0,60–1,00) zwischen Institutionen und Techniken (p ≤ 0,02). OAR-Dosen variierten erheblich zwischen den Institutionen, aber unabhängig von der Technik (p = 0,21).
Schlussfolgerung
Alle untersuchten Behandlungstechniken eignen sich gemäß den DEGRO-Empfehlungen für die SBRT von NSCLC im Frühstadium. Die Homogenisierung der SBRT-Anwendung in Deutschland ist durch die Richtlinien möglich; jedoch waren einige Charakteristika der Behandlungspläne stark technik- und benutzerabhängig und eine weitere Homogenisierung ist für künftige Studien und Empfehlungen nötig. Eine optimierte Bestrahlungsplanung sollte immer dem ALARA-Prinzip (so niedrig wie vernünftig erreichbar) folgen.




Similar content being viewed by others
References
Rocco G, Morabito A, Leone A et al (2016) Management of non-small cell lung cancer in the era of personalized medicine. Int J Biochem Cell Biol 78:173–179
Guckenberger M, Allgauer M, Appold S et al (2013) Safety and efficacy of stereotactic body radiotherapy for stage I non-small-cell lung cancer in routine clinical practice. Patterns-of-care and outcome analysis. J Thorac Oncol 8(8):1050–1058
Cascales A, Martinetti F, Belemsagha D et al (2014) Challenges in the treatment of early non-small cell lung cancer: what is the standard, what are the challenges and what is the future for radiotherapy? Transl Lung Cancer Res 3(4):195–204
Maquilan G, Timmerman R (2016) Stereotactic body radiation therapy for early-stage lung cancer. Cancer J 22(4):274–279
Chang JY, Senan S, Paul MA et al (2015) Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol 16(6):630–637
Guckenberger M, Klement RJ, Allgäuer M et al (2016) Local tumor control probability modeling of primary and secondary lung tumors in stereotactic body radiotherapy. Radiother Oncol 118(3):485–491
Guckenberger M, Andratschke N, Alheit H et al (2014) Definition of stereotactic body radiotherapy: principles and practice for the treatment of stage I non-small cell lung cancer. Strahlenther Onkol 190(1):26–33
Büther F, Ernst I, Dawood M et al (2010) Detection of respiratory tumour motion using intrinsic list mode-driven gating in positron emission tomography. Eur J Nucl Med Mol Imaging 37(12):2315–2327
ICRU (1993) Prescribing, recording and reporting photon beam therapy. J ICRU os26(1):NP (ICRU Report 50)
ICRU (1999) Prescribing, recording and reporting photon beam therapy (Supplement to ICRU Report 50). J ICRU os32(1):NP (ICRU Report 62)
ICRU (2010) Prescribing, recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT). J ICRU 10(1):NP (ICRU Report 83)
van’t Riet A, Mak AC, Moerland MA et al (1997) A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate. Int J Radiat Oncol Biol Phys 37(3):731–736
Knöös T, Kristensen I, Nilsson P (1998) Volumetric and dosimetric evaluation of radiation treatment plans: radiation conformity index. Int J Radiat Oncol Biol Phys 42(5):1169–1176
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg 93(Suppl 3):219–222
Lomax NJ, Scheib SG (2003) Quantifying the degree of conformity in radiosurgery treatment planning. Int J Radiat Oncol Biol Phys 55(5):1409–1419
Wagner TH, Bova FJ, Friedman WA et al (2003) A simple and reliable index for scoring rival stereotactic radiosurgery plans. Int J Radiat Oncol Biol Phys 57(4):1141–1149
Wu VW, Kwong DL, Sham JS (2004) Target dose conformity in 3‑dimensional conformal radiotherapy and intensity modulated radiotherapy. Radiother Oncol 71(2):201–206
Van Gellekom MP, Moerland MA, Battermann JJ et al (2004) MRI-guided prostate brachytherapy with single needle method – a planning study. Radiother Oncol 71(3):327–332
Kataria T, Sharma K, Subramani V et al (2012) Homogeneity Index: An objective tool for assessment of conformal radiation treatments. J Med Phys 37(4):207–213
Haverkamp U, Norkus D, Kriz J et al (2014) Optimization by visualization of indices. Strahlenther Onkol 190(11):1053–1059
Blanck O, Wang L, Baus W et al (2016) Inverse treatment planning for spinal robotic radiosurgery: an international multi-institutional benchmark trial. J Appl Clin Med Phys 17(3):6151
Song DY, Kavanagh BD, Benedict SH et al (2004) Stereotactic body radiation therapy. Rationale, techniques, applications, and optimization. Oncology (Williston Park, NY) 18(11):1419–1430 (discussion 1430, 1432, 1435–6)
Giglioli FR, Strigari L, Ragona R et al (2016) Lung stereotactic ablative body radiotherapy: A large scale multi-institutional planning comparison for interpreting results of multi-institutional studies. Phys Med 32(4):600–606
Zhang GG, Ku L, Dilling TJ et al (2011) Volumetric modulated arc planning for lung stereotactic body radiotherapy using conventional and unflattened photon beams: a dosimetric comparison with 3D technique. Radiat Oncol 6:152
Holt A, van Vliet-Vroegindeweij C, Mans A et al (2011) Volumetric-modulated arc therapy for stereotactic body radiotherapy of lung tumors: a comparison with intensity-modulated radiotherapy techniques. Int J Radiat Oncol Biol Phys 81(5):1560–1567
Atalar B, Aydin G, Gungor G et al (2012) Dosimetric comparison of robotic and conventional linac-based stereotactic lung irradiation in early-stage lung cancer. Technol Cancer Res Treat 11(3):249–255
Weyh A, Konski A, Nalichowski A et al (2013) Lung SBRT: dosimetric and delivery comparison of RapidArc, TomoTherapy, and IMRT. J Appl Clin Med Phys 14(4):4065
Chan MK, Kwong DL, Law GM et al (2013) Dosimetric evaluation of four-dimensional dose distributions of CyberKnife and volumetric-modulated arc radiotherapy in stereotactic body lung radiotherapy. J Appl Clin Med Phys 14(4):4229
Andratschke N, Parys A, Stadtfeld S et al (2016) Clinical results of mean GTV dose optimized robotic guided SBRT for liver metastases. Radiat Oncol 11:74
Bibault JE, Mirabel X, Lacornerie T et al (2015) Adapted prescription dose for Monte Carlo algorithm in lung SBRT: clinical outcome on 205 patients. PLOS ONE 10(7):e0133617
Lacornerie T, Lisbona A, Mirabel X et al (2014) GTV-based prescription in SBRT for lung lesions using advanced dose calculation algorithms. Radiat Oncol 9:223
Grimm J, LaCouture T, Croce R et al (2011) Dose tolerance limits and dose volume histogram evaluation for stereotactic body radiotherapy. J Appl Clin Med Phys 12(2):3368
Ojala JJ, Kapanen MK, Hyödynmaa SJ et al (2014) Performance of dose calculation algorithms from three generations in lung SBRT: comparison with full Monte Carlo-based dose distributions. J Appl Clin Med Phys 15(2):4662
Zheng D, Zhu X, Zhang Q et al (2016) Target dose conversion modeling from pencil beam (PB) to Monte Carlo (MC) for lung SBRT. Radiat Oncol 11:83
Darby SC, Ewertz M, McGale P et al (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368(11):987–998
Wang K, Eblan MJ, Deal AM et al (2017) Cardiac toxicity after radiotherapy for stage III non-small-cell lung cancer: pooled analysis of dose-escalation trials delivering 70 to 90 Gy. J Clin Oncol:JCO2016700229. doi:10.1200/JCO.2016.70.0229
Keall PJ, Mageras GS, Balter JM et al (2016) The management of respiratory motion in radiation oncology report of AAPM Task Group 76. Med Phys 33(10):3874–3900
Benedict SH, Yenice KM, Followill D et al (2010) Stereotactic body radiation therapy: the report of AAPM Task Group 101. Med Phys 37(8):4078–4101
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Moustakis, O. Blanck, F. Ebrahimi, M. ka heng Chan, I. Ernst, T. Krieger, M.-N. Duma, M. Oechsner, U. Ganswindt, C. Heinz, H. Alheit, H. Blank, U. Nestle, R. Wiehle, C. Kornhuber, C. Ostheimer, C. Petersen, G. Pollul, W. Baus, G. Altenstein, E. Beckers, K. Jurianz, F. Sterzing, M. Kretschmer, H. Seegenschmiedt, T. Maass, S. Droege, U. Wolf, J. Schoeffler, U. Haverkamp, H. Eich and M. Guckenberger declare that they have no competing interests.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Moustakis, C., Blanck, O., Ebrahimi Tazehmahalleh, F. et al. Planning benchmark study for SBRT of early stage NSCLC. Strahlenther Onkol 193, 780–790 (2017). https://doi.org/10.1007/s00066-017-1151-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1151-8
Keywords
- Stereotactic radiation therapy
- Nonsmall cell lung cancer
- Organs at risk
- Planning benchmark study
- Quality assurance