Abstract
Purpose
Severe hepatic injury due to gunshot (GSW) compared to blunt mechanism may have significantly different presentation, management, complications, and outcomes. The aim of this study was to identify the differences.
Methods
Retrospective single-center analysis June 1, 2015–June 30, 2020, included all patients with Grade III–V liver injuries due to GSW or blunt mechanism. Clinical characteristics, severity of injury, liver-related complications (rebleeding, necrosis/abscess, bile leak/biloma, pseudoaneurysm, acute liver failure) and overall outcomes (mortality, hospital length of stay, intensive care unit length of stay, and ventilatory days) were compared.
Results
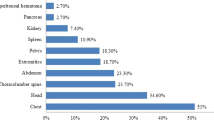
Of 879 patients admitted with hepatic trauma, 347 sustained high-grade injury and were included: 81 (23.3%) due to GSW and 266 (76.7%) due to blunt force. A significantly larger proportion of patients with GSW were managed operatively (82.7 vs. 36.1%, p < 0.001). GSW was associated with significantly more liver-related complications (40.7% vs. 27.4%, p = 0.023), specifically liver necrosis/abscess (18.5% vs. 7.1%, p = 0.003) and bile leak/biloma (12.3% vs. 5.3%, p = 0.028). On subgroup analysis, in patients with grade III injury, the incidence of liver necrosis/abscess and bile leak/biloma remained significantly higher after GSW (13.9% vs. 3.1%, p = 0.008 and 11.1% vs. 2.5%, p = 0.018, respectively). In sub analysis of 88 patients with leading severe liver injuries, GSW had a significantly longer hospital length of stay, ICU length of stay, and ventilator days.
Conclusion
GSW mechanism to the liver is associated with a higher incidence of liver–related complications than blunt force injury.
Similar content being viewed by others
References
Malhotra AK, Fabian TC, Croce MA, et al. Blunt hepatic injury: a paradigm shift from operative to nonoperative management in the 1990s. Ann Surg. 2000;231(6):804–13. https://doi.org/10.1097/00000658-200006000-00004.
Christmas AB, Wilson AK, Manning B, et al. Selective management of blunt hepatic injuries including nonoperative management is a safe and effective strategy. Surgery. 2005;138(4):606–10. https://doi.org/10.1016/j.surg.2005.07.018 (discussion 610-1).
Doklestić K, Djukić V, Ivančević N, et al. Severe blunt hepatic trauma in polytrauma patient—management and outcome. Srp Arh Celok Lek. 2015;143(7–8):416–22. https://doi.org/10.2298/sarh1508416d.
Bala M, Gazalla SA, Faroja M, et al. Complications of high grade liver injuries: management and outcomewith focus on bile leaks. Scand J Trauma Resusc Emerg Med. 2012;20:20. https://doi.org/10.1186/1757-7241-20-20.
Demetriades D, Rabinowitz B, Sofianos C. Non-operative management of penetrating liver injuries: a prospective study. Br J Surg. 1986;73(9):736–7. https://doi.org/10.1002/bjs.1800730919.
Schellenberg M, Benjamin E, Piccinini A, Inaba K, Demetriades D. Gunshot wounds to the liver: No longer a mandatory operation. J Trauma Acute Care Surg. 2019;87(2):350–5. https://doi.org/10.1097/ta.0000000000002356.
Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, Kaups K, Schuster K, Tominaga GT, AAST Patient Assessment Committee. Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg. 2018;85(6):1119–22.
Keizer AA, Arkenbosch JHC, Kong VY, et al. Blunt and penetrating liver trauma have similar outcomes in the modern era. Scand J Surg. 2021;110(2):208–13. https://doi.org/10.1177/1457496920921649.
Demetriades D, Gomez H, Chahwan S, et al. Gunshot injuries to the liver: the role of selective nonoperative management. J Am Coll Surg. 1999;188(4):343–8. https://doi.org/10.1016/s1072-7515(98)00315-9.
Navsaria PH, Nicol AJ, Krige JE, Edu S. Selective nonoperative management of liver gunshot injuries. Ann Surg. 2009;249(4):653–6. https://doi.org/10.1097/SLA.0b013e31819ed98d.
Navsaria P, Nicol A, Krige J, Edu S, Chowdhury S. Selective nonoperative management of liver gunshot injuries. Eur J Trauma Emerg Surg. 2019;45(2):323–8. https://doi.org/10.1007/s00068-018-0913-z.
Marr JD, Krige JE, Terblanche J. Analysis of 153 gunshot wounds of the liver. Br J Surg. 2000;87(8):1030–4. https://doi.org/10.1046/j.1365-2168.2000.01487.x.
Kozar RA, Moore JB, Niles SE, et al. Complications of nonoperative management of high-grade blunt hepatic injuries. J Trauma. 2005;59(5):1066–71. https://doi.org/10.1097/01.ta.0000188937.75879.ab.
Carrillo EH, Platz A, Miller FB, Richardson JD, Polk HC Jr. Non-operative management of blunt hepatic trauma. Br J Surg. 1998;85(4):461–8. https://doi.org/10.1046/j.1365-2168.1998.00721.x.
Hommes M, Kazemier G, Schep NW, Kuipers EJ, Schipper IB. Management of biliary complications following damage control surgery for liver trauma. Eur J Trauma Emerg Surg. 2013;39(5):511–6. https://doi.org/10.1007/s00068-013-0304-4.
Asensio JA, Demetriades D, Chahwan S, et al. Approach to the management of complex hepatic injuries. J Trauma. 2000;48(1):66–9. https://doi.org/10.1097/00005373-200001000-00011.
Li M, Yu WK, Wang XB, Ji W, Li JS, Li N. Non-operative management of isolated liver trauma. Hepatobil Pancreat Dis Int. 2014;13(5):545–50. https://doi.org/10.1016/s1499-3872(14)60049-7.
Kozar RA, Moore FA, Cothren CC, et al. Risk factors for hepatic morbidity following nonoperative management: multicenter study. Arch Surg. 2006;141(5):451–8. https://doi.org/10.1001/archsurg.141.5.451 (discussion 458-9).
Afifi I, Abayazeed S, El-Menyar A, Abdelrahman H, Peralta R, Al-Thani H. Blunt liver trauma: a descriptive analysis from a level I trauma center. BMC Surg. 2018;18(1):42. https://doi.org/10.1186/s12893-018-0369-4.
Brillantino A, Iacobellis F, Festa P, et al. Non-operative management of blunt liver trauma: safety, efficacy and complications of a standardized treatment protocol. Bull Emerg Trauma. 2019;7(1):49–54. https://doi.org/10.29252/beat-070107.
Dabbs DN, Stein DM, Scalea TM. Major hepatic necrosis: a common complication after angioembolization for treatment of high-grade liver injuries. J Trauma. 2009;66(3):621–7. https://doi.org/10.1097/TA.0b013e31819919f2 (discussion 627-9).
Samuels JM, Urban S, Peltz E, et al. A modern, multicenter evaluation of hepatic angioembolization—complications and readmissions persist. Am J Surg. 2020;219(1):117–22. https://doi.org/10.1016/j.amjsurg.2019.06.021.
Schnüriger B, Inderbitzin D, Schafer M, Kickuth R, Exadaktylos A, Candinas D. Concomitant injuries are an important determinant of outcome of high-grade blunt hepatic trauma. Br J Surg. 2009;96(1):104–10. https://doi.org/10.1002/bjs.6439.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yong Fu, Meghan Lewis, Delbrynth Mitchao, Elizabeth Benjamin, and Monica Wong declare that they have no conflict of interest. Demetrios Demetriades is an editorial board member of the European Journal of Trauma and Emergency Surgery.
Ethical statement
This study has been approved by the appropriate ethics committee (University of Southern California Institutional Review Board) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, Y., Lewis, M.R., Mitchao, D.P. et al. Gunshot wound versus blunt liver injuries: different liver-related complications and outcomes. Eur J Trauma Emerg Surg 49, 505–512 (2023). https://doi.org/10.1007/s00068-022-02096-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02096-6