Abstract
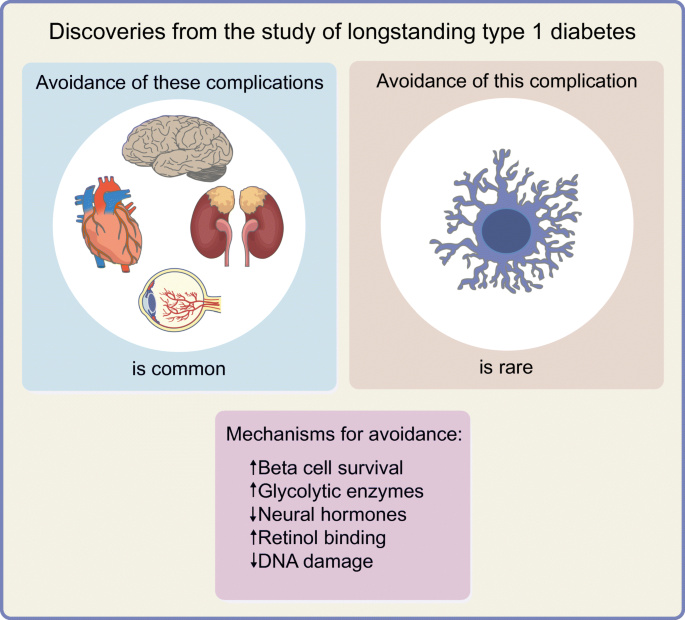
Award programmes that acknowledge the remarkable accomplishments of long-term survivors with type 1 diabetes have naturally evolved into research programmes to determine the factors associated with survivorship and resistance to chronic complications. In this review, we present an overview of the methodological sources of selection bias inherent in survivorship research (selection of those with early-onset diabetes, incidence–prevalence bias and bias from losses to follow-up in cohort studies) and the breadth and depth of literature focusing on this special study population. We focus on the learnings from the study of longstanding type 1 diabetes on discoveries about the natural history of insulin production loss and microvascular complications, and mechanisms associated with them that may in future offer therapeutic targets. We detail descriptive findings about the prevalence of preserved insulin production and resistance to complications, and the putative mechanisms associated with such resistance. To date, findings imply that the following mechanisms exist: strategies to maintain or recover beta cells and their function; activation of specific glycolytic enzymes such as pyruvate kinase M2; modification of AGE production and processing; novel mechanisms for modification of renin–angiotensin–aldosterone system activation, in particular those that may normalise afferent rather than efferent renal arteriolar resistance; and activation and modification of processes such as retinol binding and DNA damage checkpoint proteins. Among the many clinical and public health insights, research into this special study population has identified putative mechanisms that may in future serve as therapeutic targets, knowledge that likely could not have been gained without studying long-term survivors.
Graphical abstract
Similar content being viewed by others
Introduction
Although the discovery of insulin in 1921 converted type 1 diabetes from a universally fatal to a chronic condition, in the middle of that century there was approximately 50% mortality risk, primarily from end-stage renal failure, in people with type 1 diabetes who had survived to their 40s [1]. It was in this context that the Joslin Diabetes Center in Boston acknowledged that surviving decades was a self-management accomplishment worthy of immense pride and accolade [2, 3]. Thus began in 1948 the Joslin Medalist Program awarding 25 year medals and, in later years, the 50 and 75 year medals to honour these duration milestones. Rather than assuming such success is purely behavioural, in 1997 Joslin Diabetes Center investigators began a formal research programme to create cross-sectional and cohort study analyses with the goal of better understanding the factors (genetic, physiological, environmental) associated with protection from complications. Such initiatives were not unique. Many international groups have acknowledged long-term survivors and contributed descriptive and causal inference research into complications susceptibility. Interestingly, mortality rates have appeared to decline in the past decades [4], and it is likely that life expectancy for many people with type 1 diabetes may approach or even exceed that of the age-, sex- and race-standardised general population [5]. Table 1 provides a non-exhaustive list of the investigational centres that have focused on long-term survivors, either through the direct recruitment of participants into traditional cohort studies or through analyses nested within larger longitudinal cohorts and registry designs. Analyses most frequently align with the Joslin Medalist cohort’s initial operating definition of long-duration diabetes exceeding 50 years, yet many of these have examined, for different purposes, cohorts and subgroups of perfectly valid shorter or longer extreme durations (shown in Table 1).
For this review, our main objective was to present the rationale for the study of such a specialised population, present the key methodological issues that inform analytical design, and highlight key research findings that may not have been possible through the study of only participants with diabetes of shorter duration.
Key methodological considerations in the study of longstanding diabetes: Incidence–prevalence bias
The core objective in the study of longstanding diabetes is to better understand an ‘extreme phenotype’ such as an individual who, despite more than 50 years, for example, of diabetes duration has survived without substantial burden of complications. This survival occurred, in part, through the era that included lack of physiological insulins, lack of capacity for self-monitoring of glucose, or even the knowledge of interventions such as intensive insulin therapy, access to measures of mean glucose exposure (e.g. HbA1c), or limitations in the screening tests for early complications [2, 3]. It stands to reason, then, that such an individual is very likely to have a major protective behaviour or environment such as regular exercise or a supportive spouse or social network [6, 7], or perhaps biological resistance to a pathophysiological process, or existence of a protective gene profile. On the other hand, though complications can occur at any age and duration of diabetes beyond 5 years, after 50 years of diabetes there is greater certainty that an individual at risk of an outcome will have declared this risk or not [8]. The extreme phenotype of an individual with 50 years of diabetes without complications could be compared, for example, to an individual with short duration of diabetes who has developed extensive diabetes complications. A less-extreme comparison frequently used is with individuals in whom complications are present (rather than absent) after longstanding diabetes.
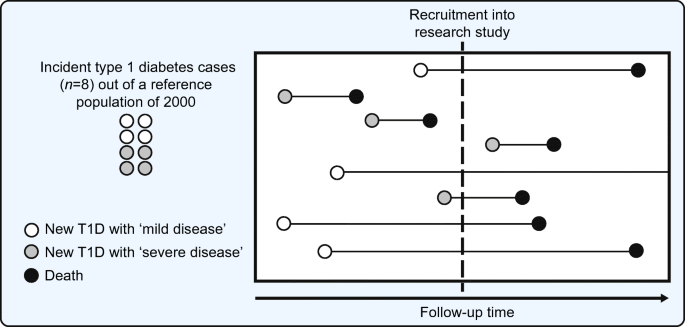
These research approaches, however, are susceptible to forms of selection bias. First, they favour selection of childhood-onset type 1 diabetes. Second, incidence–prevalence bias (frequently referred to as Neyman’s bias or survivor bias) occurs when the risk of a complication is estimated on the basis of data collected at a given time point in a series of survivors rather than data gathered during a certain time period in a study population of incident diabetes [9, 10]. Imagine a hypothetical population cohort of 2000 individuals followed from birth wherein eight individuals develop type 1 diabetes, four of whom have greater disease severity such that they die within a decade and the other four have more indolent disease such that their survivorship is similar to that of the general population. If at a point in time a group of investigators seek to recruit all individuals with type 1 diabetes from this implicit, but unknown, underlying cohort, they are most likely to select those with more indolent diabetes as they are more likely to be alive at the time of screening (see Fig. 1). Furthermore, if they seek individuals with diabetes of 50 years’ duration, those with greater disease severity have not survived for the opportunity to be accrued. However, creating an incident type 1 diabetes cohort does not fully overcome this bias as selection bias may be induced by censorship, either through losses to follow-up or death from competing risks. In summary, selection bias occurs from the focus on childhood-onset type 1 diabetes, the existence of incidence–prevalence bias, and selection from losses to follow-up in cohort studies. Rather than focus on measures such as cumulative incidence, researchers have focused efforts on the less-biased objectives of determining factors associated with the extreme phenotypes, through inventive adaptations of case series and cross-sectional, case–control and cohort study designs.
Schematic representation of incidence–prevalence bias. In a hypothetical reference population of 2000 general population members, eight have new onset diabetes. Of these eight index cases, four have ‘mild disease’ such that they survive longer, while four have ‘severe disease’ (perhaps owing to adverse genetic, environmental, behavioural or physiological factors) such that survival is shorter. At the time of recruitment into a research study of type 1 diabetes (indicated by the dashed vertical line in the figure), available cases for recruitment are imbalanced in favour of those with greater survival. Rather than selection of all eight individuals, the four with ‘mild disease’ are available for recruitment but only one with ‘severe disease’ is available. In the process of selection of prevalent type 1 diabetes cases, the probability of selecting individuals with longer survival is greater than if all new-onset cases had been included on their index (diagnosis date). This phenomenon is referred to as incidence–prevalence bias (Neyman’s bias or survivor bias). Incidence–prevalence bias, preferential selection for childhood-onset diabetes and selection based on losses to follow-up (from competing events such as death or outcomes like admission to long-term care facilities) make up the three fundamental sources of selection bias in the traditional cohort studies and registry-based cohort studies for longstanding type 1 diabetes. T1D, type 1 diabetes. Adapted from Tripepi et al. [9]. This figure is available as part of a downloadable slideset
Residual beta cell function in longstanding diabetes
The study of people with longstanding diabetes has drastically changed the traditionally accepted model of type 1 diabetes, which states that endogenous insulin production declines within 5 years of diabetes onset and that there is a complete loss of beta cells and insulin production [11]. While the study of long-term survivors might be expected to overestimate the proportion with endogenous insulin production if it is indeed associated with survival (owing to the issues of selection bias just discussed), we must accept that the finding of even a small proportion of long-term survivors would challenge the traditionally accepted model. Such preservation could protect against hypoglycaemia and extreme glycaemic exposure and therefore may be a key protective factor for the development of glucose-dependent long-term complications such as retinopathy [12,13,14]. Leading advances in this line of research, the Joslin Medalist investigators examined endogenous insulin production through multiple physiological stimuli including random and mixed-meal stimulated C-peptide production, and a hyperglycaemic i.v. clamp with arginine infusion for stimulation of insulin and thus C-peptide production [15]. C-peptide, proinsulin’s cleaved ‘connecting peptide’ between the α- and β-chains that make up the functioning insulin molecule, serves as a dependable measure of endogenous insulin production as it is not present in pharmaceutical insulin. These research methods indicated that a large proportion (one-third to one-half) of the individuals surviving for 50 years had some form of detectable C-peptide production and that levels of production fluctuated over a subsequent follow-up period of 4 years. Furthermore, examination of 68 post-mortem pancreases (from an innovative collaboration with the National Disease Research Interchange and its affiliated organ procurement networks) revealed detectable beta cells in all individuals, either atypically as single cells or within morphologically distinct islets. Although the forces of selection may have led to an overestimate of preserved function, studies of shorter-duration diabetes in which C-peptide expression is substantial suggest that selection cannot fully explain these findings, and detectable beta cells by post-mortem histological examination was ubiquitous [13, 16,17,18]. Large-scale registry data from the Scottish Diabetes Research Network Type 1 Bioresource (SDRNT1BIO) study has revealed that persistent C-peptide secretion may have a particular association with aspects of the type 1 diabetes phenotype, including variants in HLA gene regions that are different from the specific regions associated with early-onset type 1 diabetes [19]. A focus on determining the relevance of these HLA regions and how they impact maintenance of insulin secretion may in future help determine mechanisms of islet cell autoimmunity and may inform novel pathways that could be targeted to limit, or ideally reverse, the loss of insulin production in type 1 diabetes [19]. Taken together, these findings raise the possibility that hypoglycaemia-related outcomes, long-term glycaemic control, and even retinopathy risk may be better in those who maintain some insulin production [14, 20, 21], and that interventions that counteract autoimmunity or that have trophic effects on beta cells could have putative impact beyond the time surrounding the diagnosis of type 1 diabetes.
It is necessary to acknowledge that these study populations may include individuals with a classification of diabetes other than type 1. For example, monogenic diabetes variants (especially the more common HNF1α and HNF4α [also known as HNF1A and HNF4A, respectively] may be confused with a diagnosis of type 1 diabetes [22, 23]. This was systematically studied in the Joslin Medalist cohort in which 7.9% of participants were found to have likely pathogenic variants in genetic studies [15]. However, the relevance of these variants as the sole cause of the diabetes is quite unlikely. Specifically, such monogenic forms of diabetes would most likely be associated with levels of C-peptide much higher than the levels observed in these longevity studies [24]. For example, in a study of 77 individuals with fairly long-duration HNF1α diabetes, the lowest C-peptide level was 0.36 nmol/l, which far exceeded the highest level observed in the Joslin Medalist cohort. Moreover, 0.2 nmol/l has recently been proposed as a threshold above which to prompt monogenic diabetes screening, again exceeding the highest levels in the Joslin Medalist cohort [22]. However, future work should focus on the determination of genetic factors, including the polygenic risk score for type 1 diabetes and targeted genetic screening.
Diabetic kidney disease and renin–angiotensin–aldosterone system activation
Even at the end of the last century it was evident that individuals with longstanding diabetes maintained risk for chronic kidney disease. Research from the Newcastle group demonstrated that albuminuria was present in approximately 27% of individuals with 30 or more years of type 1 diabetes [25] and that this was independently associated with greatly augmented 7 year mortality risk [26, 27]. These prevalence estimates were consistent with Swedish National Registry data showing that chronic kidney disease, primarily defined by albuminuria, was present in nearly half of those with type 1 diabetes of 50 or more years’ duration [28]. Cumulative incidence from these earlier reports stands in contrast to cohorts accrued more recently in which prevalence of albuminuria and chronic kidney dysfunction appears to be much lower, likely in view of secular trends in the use of intensive insulin and renoprotective therapies, as well as the successful strategies in those earlier reports of employing long-term cohort and registry data to reduce selection bias [29, 30]. Though undoubtedly underestimating lifetime diabetic kidney disease (DKD) risk, these studies can nevertheless serve the important purpose of identifying specific pathways and protective factors.
Through examination of post-mortem renal glomerular specimens from 50 year Medalists, the Joslin investigators were able to determine that those protected from clinical nephropathy displayed exaggerated glycolytic flux. This appears to be associated with decreasing accumulation of toxic glucose metabolites which in turn improves mitochondrial function, podocyte survival and other morphological markers of glomerular pathology. Extending this finding to rodent models, activation of the key glycolytic enzyme pyruvate kinase M2 (PKM2) resulted in normalisation of renal haemodynamic and mitochondrial dysfunction, and subsequent glomerular morphological changes [31,32,33]. While renal handling of dynamic glycolytic flux appeared to be salutary, there are also data to suggest that the renal handling of AGEs may play a role. Higher exposure of kidneys to circulating levels of AGEs would generally be predicted to be associated with chronic kidney disease, such as exposure to higher Nε-(1-carboxyethyl)lysine (CEL) and pentosidine level. However, it was observed that lower levels of certain AGEs (Nε-carboxymethyl-lysine [CML] and fructosyl lysine) were associated with nephropathy [30], perhaps through increased renal processing of these toxic metabolites leading to their increased clearance but resulting in greater renal tubule-interstitial exposure and damage [34]. Similar lower levels of other markers of protein glycation damage were observed for retinopathy and other complications in Joslin Medalists [30]. This concept that hyperglycaemia may initiate renal damage by altering both haemodynamics and metabolism to cause dysfunction of renal vascular, glomerular and tubulo-interstitial cells in parallel is plausible since therapeutics that only affect haemodynamics, such as traditional inhibition of the renin–angiotensin–aldosterone system (RAAS), have not appeared to substantially counteract the burden of kidney disease in diabetes populations [31, 35].
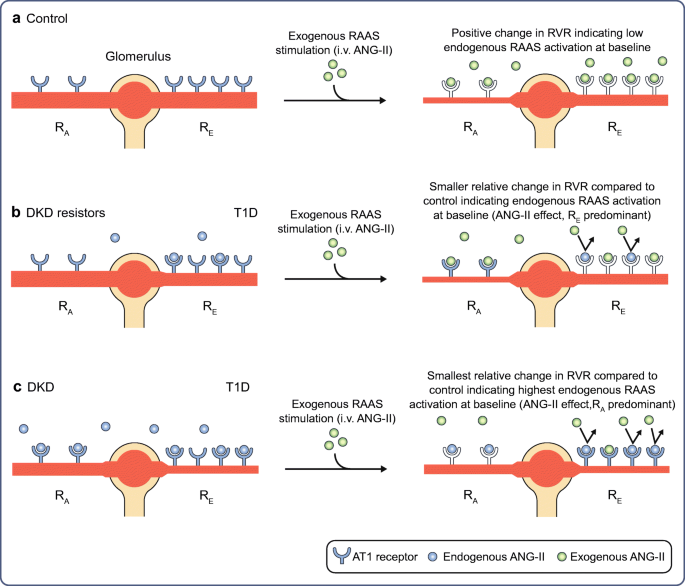
In our own work in the Canadian Study for Longevity in Type 1 Diabetes, we committed to a primary outcome of determining the significance of RAAS activation on DKD. If indeed RAAS activation is the fundamental process of renal injury in type 1 diabetes, certainly this should be evident among individuals with a lifetime of diabetes in that they will have declared with certainty their risk of chronic kidney disease onset. By way of background, it has been established that a subset of individuals (even those with short-duration type 1 diabetes) exhibit hyperglycaemia-induced RAAS activation, in turn leading to increased renal vascular resistance (RVR) and consequent increased glomerular pressure and renal hyperfiltration as compared with during euglycaemia [36]. In those of intermediate age and diabetes duration, evidence of this activation appears to be amplified such that RVR is further increased compared with age- and sex-matched control individuals, and it is associated with the development of indicators of clinical chronic kidney disease [37, 38]. To probe the level of endogenous intrarenal RAAS activity, we applied an infusion of angiotensin-II (ANG-II) to people with 50 years or more of diabetes and a second group of generally age- and sex-matched non-diabetes control individuals to induce angiotensin 1 (AT1) receptors. AT1 receptors are primarily located on the efferent arteriole and their stimulation causes constriction of the efferent arteriole and raises intraglomerular pressure. The physiological role of this mechanism is to maintain glomerular filtration on renal blood flow in the setting of hypovolaemia or hypotension. Abnormal neurohormonal activation induced by hyperglycaemia in diabetes, rather than serving the purpose to maintain glomerular filtration, raises intraglomerular pressure to levels that can induce renal injury. Study of renal haemodynamics has established the degree of change in RVR as the reference measure of endogenous intrarenal RAAS activation. In simple terms, an individual who responds less to exogenous stimulation of the RAAS using ANG-II infusion has developed resistance to its effect because of chronic, maximal stimulation by endogenous ANG-II. An exaggerated RVR response to ANG-II is indicative of lower, nearer normal, endogenous RAAS activation [39,40,41,42,43]. We found that even nephropathy resistors (long-term survivors of type 1 diabetes without evidence of chronic kidney disease) did indeed have evidence of a substantial degree of endogenous RAAS activation compared with non-diabetic control individuals. This effect was most pronounced on the traditional target of this neurohormonal activation, the efferent arteriole (Fig. 2). Individuals with nephropathy had an even greater degree of RAAS activation; however, rather than the predominant effect being constriction of the efferent arteriole, there was greater dilatation of the afferent arteriole, with an amplified effect of increasing intraglomerular pressure (Fig. 2).
RAAS activation in longstanding type 1 diabetes. In individuals with longstanding type 1 diabetes, when compared with age- and sex-matched control individuals, abnormal afferent arteriolar dilatation, rather than classical efferent constriction, is associated with DKD. AT1 receptors are predominantly expressed at the renal efferent arteriole with less relative expression at the afferent arteriole. In non-diabetic control individuals (a), upon exogenous RAAS stimulation with i.v. infusion of ANG-II, ANG-II freely interacts with available AT1 receptors at the afferent and efferent arterioles, initiating vasoconstrictive responses. In individuals with type 1 diabetes without DKD (DKD resistors) (b), locally within the kidney there is more endogenous intrarenal ANG-II at baseline occupying AT1 receptors (relative to non-diabetes controls), predominantly at the efferent arterioles compared with the afferent arterioles. In contrast, in individuals with DKD (c), there is exaggerated expression of endogenous ANG-II both at the afferent and efferent arterioles at baseline, such that upon exogenous RAAS stimulation, there are fewer AT1 receptors available for ANG-II binding and therefore fewer vasoconstrictive changes relative to DKD resistors and controls predominantly at the afferent arteriole. This finding indicates that abnormal dilatation of the afferent arteriole is a key feature of individuals with DKD after longstanding type 1 diabetes, a process not amenable to pharmacological inhibition from angiotensin converting enzyme inhibitors or aldosterone receptor blockers. RA, renal afferent arteriole; RE, renal efferent arteriole; T1D, type 1 diabetes. Republished with permission of the American Society for Clinical Investigation from Lovshin et al. [29]; permission conveyed through Copyright Clearance Center, Inc. This figure is available as part of a downloadable slideset
This was an important finding from a pathophysiological perspective, simply because RAAS inhibitors, the mainstay of management of DKD, are expected to exert protective effect through inhibition of efferent arteriolar AT1 receptors, leading to relative dilatation and reduction in renovascular resistance. However, given that the dominant finding was abnormal afferent arteriolar dilatation leading to greater intraglomerular pressure in individuals with DKD, this could explain the incomplete renoprotection observed with RAAS inhibitors [35]. In our study of renal haemodynamic abnormalities, we found that higher-than-normal uric acid was associated with afferent arteriolar dysfunction [44, 45]. Nevertheless, a recent definitive clinical trial of uric-acid-lowering therapy in people with type 1 diabetes did not protect against renal function loss over 3 years [46]. The second putative strategy would be the normalisation of afferent arteriolar tone induced by sodium–glucose cotransporter (SGLT) inhibition, which has a proven dramatic cardio-renal protective effect in those with type 2 diabetes [47, 48], and substantial supportive physiological evidence in type 1 diabetes [49, 50]. The findings from the study of longstanding diabetes, in addition to key findings related to endogenous mechanisms of protection from cardiovascular [6, 28, 51,52,53,54,55,56,57,58,59,60,61,62] and renal disease, such as maintenance of circulating progenitor cells [63], strongly support further research into the potential major effect of pharmacotherapies such as SGLT inhibition on cardio-renal protection in those with type 1 diabetes, especially on the progression of DKD and heart failure.
Peripheral and central nervous system disease
Though people with diabetes are susceptible to a number of types of peripheral nerve damage, by far the most common is the symmetrical, length-dependent clinical presentation of diabetic distal symmetric polyneuropathy [64]. When compared with other complications, such neuropathy has received less focus in previous studies of longevity cohorts, likely owing to the complexities in objective tests for its identification and quantification of severity. Using self-reported outcome scales or physical examination scales, it has been determined that 40–60% of individuals with longstanding diabetes may be resistant to the development of clinical neuropathy [30, 65,66,67]. However, in our Canadian Study for Longevity in Type 1 Diabetes research programme, we focused on objective measures of neuropathy examining peripheral nerve function. When subjected to objective testing, we found that the presence of at least one neuropathic symptom or sign corroborated by abnormal peripheral nerve function by the gold standard nerve conduction study testing in those with 50 or more years of diabetes was nearly ubiquitous (approximately 90% of participants studied) [68]. Neuropathy was associated with accentuated diabetes-related distress and depressive symptoms (even independent of the presence of neuropathic pain symptoms), greater than the level of distress associated with any other diabetes complication [69]. Furthermore, we found sex differences such that women appeared to have a greater burden of neuropathic pain than men even with lower severity of objective peripheral nerve dysfunction [68]. These findings have implications for treatment of people with neuropathy, in which strategies to reduce emotional distress and sex-specific strategies for the management of neuropathic pain should be considered.
Several research groups have examined aspects of cognitive function and dementia as central nervous system complications of diabetes [70]. The University of California at San Francisco group have contributed systematically through use of administrative databases (in which at least approximately 5% of those with 50 or more years of type 1 diabetes carry a diagnosis of dementia) and cross-sectional (and future cohort) methods through the Study Of Longevity In Diabetes (SOLID). In SOLID, though the researchers did not define the proportion of participants with dementia, they found a number of factors to be associated with cognition: one’s self-determination for diabetes management (‘locus of control’); glycaemic exposure; history of severe hypoglycaemia; history of diabetic ketoacidosis; history of traumatic brain injury; and sleep quality [71,72,73,74,75,76]. Of great historical concern was the potential causal association between hypoglycaemia and subsequent cognitive impairment. This association was not observed in shorter duration of diabetes [77]. However, in SOLID, focusing on long-duration diabetes, recent severe hypoglycaemia was associated with an OR of 3.22 (95% CI 1.30, 7.90) for impaired global cognition and 3.15 (95% CI 1.19, 8.29) for cognitive impairment on the language domain, each defined by standardised z scores of less than 1.5 SD below the population mean from cognitive assessment tests. The Joslin Medalist Study similarly evaluated factors associated with cognitive functioning and found influence of concomitant CVD and retinopathy [70]. There is currently a major research effort examining cognitive function and neuro-imaging in the study population from the Diabetes Control and Complications Trial and Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC), now followed for over 30 years, as it includes a greater proportion of older adults reaching 50 years duration [78]. Additionally, compared with the studies discussed above, this analysis will permit evaluation of causality between hypoglycaemia and diabetic ketoacidosis with the risk of long-term cognitive impairment. The burden of cognitive dysfunction and dementia in those with longstanding diabetes and the identification of interventions for prevention of decline represent an urgent research need.
Retinopathy and macular oedema
Although still susceptible to secular trends and the same forces of selection bias described previously (childhood-onset diabetes, incidence–prevalence bias, death and competing risks), cohort studies have suggested that the cumulative incidence of diabetic retinopathy likely exceeds 90% in people with type 1 diabetes, and that of macular oedema is likely substantially lower [79,80,81]. However, selected cohorts with longstanding type 1 diabetes demonstrate larger proportions of individuals free of retinopathy and macular oedema even after 50 or more years of diabetes duration (e.g. 35% of the Joslin Medalists and 16% of participants in the Canadian Study of Longevity in Type 1 Diabetes) [30, 82]. The role of long-term excess glycaemic exposure (and the formation of AGEs) has been clear from multiple experimental sources [83], including the Joslin Medalist Study that found higher levels of plasma carboxyethyl lysine and pentosidine but not traditional markers of glycaemic exposure (discussed above in the context of renal injury) also associated with the presence of retinopathy [30]. In that same study, individuals free of retinopathy appeared to be at minimal risk of progression [30]; the forces of selection may explain this so it is important that clinicians consider the appropriate risk factor modification for prevention of incidence and progression of complications at any age or duration. However, a number of mechanisms have been identified to potentially explain resistance to retinopathy and other complications. Higher concentrations of retinol binding protein 3 (RBP3), a transport protein secreted mainly by the retinal photoreceptors, were observed in those resistant to the development of retinopathy [84, 85]. This fundamental discovery was of great importance as RBP3 overexpression in resistors could affect multiple known pathological pathways including inhibition of the tyrosine phosphorylation of vascular endothelial growth factor receptors, decreasing glucose uptake via GLUT1 into retinal endothelial cells and Müller cells, thus acting as a countermeasure to the downstream hyperglycaemia-induced injurious pathways including local cytokine production [86]. Additionally, impaired growth, reprogramming and differentiation of circulating inducible pluripotent stem cells were observed in those with any complication (but prevalence and severity of retinopathy was the greatest), and genomic and proteomic analysis revealed association with DNA damage checkpoint proteins, specifically the miT-200 microRNA transcriptional regulator [87]. Differential exaggerated responses to RAAS activation in the peripheral vasculature of those with proliferative retinopathy were observed in Canadian participants such that even in the absence of kidney disease, neurohormonal abnormalities are a fundamental pathway in those with retinopathy and longstanding type 1 diabetes duration as they have been demonstrated to have particular effect on novel aspects of renal vascular (afferent arteriole) and peripheral vascular dysfunction [52].
Taken together as an extensive literature, the study of retinopathy in longstanding diabetes has identified that greater glycaemic exposure and its downstream injurious mechanisms can putatively be modified by overexpression of a retinol binding protein pathway and that modification of the DNA damage checkpoint pathways in circulating stem cells and novel pharmacological mechanisms for modifying RAAS activation may serve as potential therapeutic targets for diabetes complications.
Concluding considerations
In this review, we have focused on the learnings from the study of longstanding type 1 diabetes on discoveries about the natural history of insulin production loss and microvascular complications and the mechanisms associated with them that may in future offer therapeutic targets. Such fundamental findings likely could not have occurred without studying the extraordinary people who have survived longstanding diabetes. To date, prominent among these potentially beneficial approaches are strategies to maintain or recover existing beta cells and their function, activation of specific glycolytic enzymes (e.g. PKM2), modification of AGE production and processing, novel mechanisms for modification of RAAS activation (in particular, those that may normalise afferent rather than efferent renal arteriolar resistances), and activation and modification of processes such as retinol binding and DNA damage checkpoint proteins. Highlighting these particular discoveries in no way is meant to overshadow the wealth of descriptive data from longevity studies, implications on process of care and public health policies [66], or the need to better implement and emphasise standard clinical practices in the management of this unique patient group [51]. Additionally, we must further the knowledge on specific findings such as poorer bone health despite maintenance of adequate levels of bone density [88,89,90], the dramatically high risk of troublesome cheiroarthropathy [91], a better understanding of heart failure and atherosclerotic CVD, and the wealth of research around mental health, diabetes-specific emotional distress, and the factors associated with the resilience shown by so many outstanding people with a lifetime of type 1 diabetes.
Abbreviations
- ANG-II:
-
Angiotensin-II
- AT1:
-
Angiotensin 1
- DKD:
-
Diabetic kidney disease
- PKM2:
-
Pyruvate kinase M2
- RAAS:
-
Renin–angiotensin–aldosterone system
- RBP3:
-
Retinol binding protein 3
- RVR:
-
Renal vascular resistance
- SGLT:
-
Sodium–glucose cotransporter
- SOLID:
-
Study Of Longevity In Diabetes
References
Krolewski AS, Warram JH, Christlieb AR, Busick EJ, Kahn CR (1985) The changing natural history of nephropathy in type I diabetes. Am J Med 78:785–794. https://doi.org/10.1016/0002-9343(85)90284-0
Clarke SF, Foster JR (2012) A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. Br J Biomed Sci 69:83–93
Bliss M (1993) The history of insulin. Diabetes Care 16(Suppl 3):4–7
Rawshani A, Rawshani A, Franzen S et al (2017) Mortality and Cardiovascular Disease in Type 1 and Type 2 Diabetes. N Engl J Med 376:1407–1418. https://doi.org/10.1056/NEJMoa1608664
The Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group (2016) Mortality in Type 1 Diabetes in the DCCT/EDIC Versus the General Population. Diabetes Care 39:1378–1383. https://doi.org/10.2337/dc15-2399
He ZH, D’Eon SA, Tinsley LJ et al (2015) Cardiovascular disease protection in long-duration type 1 diabetes and sex differences. Diabetes Care 38:e73–e74. https://doi.org/10.2337/dc15-0017
Altman JJ, Vincent-Cassy C, Feldman-Billard S (2009) Improvements in the lifestyle of patients who have had type 1 diabetes for 50 years: an optimistic message. Diabetologia 52:364–366. https://doi.org/10.1007/s00125-008-1216-4
The Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group et al (2015) Effect of intensive diabetes therapy on the progression of diabetic retinopathy in patients with type 1 diabetes: 18 years of follow-up in the DCCT/EDIC. Diabetes 64:631–642
Tripepi G, Jager KJ, Dekker FW, Wanner C, Zoccali C (2008) Bias in clinical research. Kidney Int 73:148–153. https://doi.org/10.1038/sj.ki.5002648
Hernan MA, Hernandez-Diaz S, Robins JM (2004) A structural approach to selection bias. Epidemiology 15:615–625. https://doi.org/10.1097/01.ede.0000135174.63482.43
DiMeglio LA, Evans-Molina C, Oram RA (2018) Type 1 diabetes. Lancet 391:2449–2462
Roep BO, Stobbe I, Duinkerken G et al (1999) Auto- and alloimmune reactivity to human islet allografts transplanted into type 1 diabetic patients. Diabetes 48:484–490
Greenbaum CJ, Anderson AM, Dolan LM et al (2009) Preservation of beta-cell function in autoantibody-positive youth with diabetes. Diabetes Care 32:1839–1844. https://doi.org/10.2337/dc08-2326
Keenan HA, Sun JK, Levine J et al (2010) Residual insulin production and pancreatic β-cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes 59:2846–2853. https://doi.org/10.2337/db10-0676
Yu MG, Keenan HA, Shah HS et al (2019) Residual beta cell function and monogenic variants in long-duration type 1 diabetes patients. J Clin Invest 129:3252–3263
McGee P, Steffes M, Nowicki M et al (2014) Insulin secretion measured by stimulated C-peptide in long-established Type 1 diabetes in the Diabetes Control and Complications Trial (DCCT)/ Epidemiology of Diabetes Interventions and Complications (EDIC) cohort: a pilot study. Diabet Med 31:1264–1268
Davis AK, DuBose SN, Haller MJ et al (2015) Prevalence of detectable C-Peptide according to age at diagnosis and duration of type 1 diabetes. Diabetes Care 38:476–481. https://doi.org/10.2337/dc14-1952
Oram RA, Jones AG, Besser RE et al (2014) The majority of patients with long-duration type 1 diabetes are insulin microsecretors and have functioning beta cells. Diabetologia 57:187–191. https://doi.org/10.1007/s00125-013-3067-x
McKeigue PM, Spiliopoulou A, McGurnaghan S et al (2019) Persistent C-peptide secretion in Type 1 diabetes and its relationship to the genetic architecture of diabetes. BMC Med 17:165
Lovblom L, Cardinez N, Orszag A et al (2019) 126 - Prevalence of Detectable C-peptide in Longstanding Type 1 Diabetes (T1D). Can J Diabetes 43:S43. https://doi.org/10.1016/j.jcjd.2019.07.135
Rother KI, Harlan DM (2010) Comment on: Keenan et al. (2010) residual insulin production and pancreatic ss-Cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes 2010;59:2846–2853. Diabetes 59:e26 author reply e27
Broome DT, Pantalone KM, Kashyap SR, Philipson LH (2020) Approach to the Patient with MODY-Monogenic Diabetes. J Clin Endocrinol Metab 106:237–250
Thirumalai A, Holing E, Brown Z, Gilliam LK (2013) A case of hepatocyte nuclear factor-1b (TFC2) maturity onset diabetes of the young misdiagnosed as type 1 diabetes and treated unnecessarily with insulin. J Diabetes 5:462–464
Szopa M, Klupa T, Kapusta M et al (2019) A decision algorithm to identify patients with high probability of monogenic diabetes due to HNF1A mutations. Endocrine 64:75–81. https://doi.org/10.1007/s12020-019-01863-7
Mackin P, Macleod JM, New JP, Marshall SM (1996) Renal function in long-duration type I diabetes. Diabetes Care 19:249–251. https://doi.org/10.2337/diacare.19.3.249
Arun CS, Stoddart J, Mackin P, MacLeod JM, New JP, Marshall SM (2003) Significance of microalbuminuria in long-duration type 1 diabetes. Diabetes Care 26:2144–2149. https://doi.org/10.2337/diacare.26.7.2144
Stadler M, Auinger M, Anderwald C et al (2006) Long-term mortality and incidence of renal dialysis and transplantation in type 1 diabetes mellitus. J Clin Endocrinol Metab 91:3814–3820. https://doi.org/10.1210/jc.2006-1058
Adamsson Eryd S, Svensson AM, Franzen S, Eliasson B, Nilsson PM, Gudbjornsdottir S (2017) Risk of future microvascular and macrovascular disease in people with Type 1 diabetes of very long duration: a national study with 10-year follow-up. Diabet Med 34:411–418. https://doi.org/10.1111/dme.13266
Lovshin JA, Boulet G, Lytvyn Y et al (2018) Renin-angiotensin-aldosterone system activation in long-standing type 1 diabetes. JCI Insight 3:e96968
Sun JK, Keenan HA, Cavallerano JD et al (2011) Protection from retinopathy and other complications in patients with type 1 diabetes of extreme duration: the joslin 50-year medalist study. Diabetes Care 34:968–974. https://doi.org/10.2337/dc10-1675
Gordin D, Shah H, Shinjo T et al (2019) Characterization of Glycolytic Enzymes and Pyruvate Kinase M2 in Type 1 and 2 Diabetic Nephropathy. Diabetes Care 42:1263–1273. https://doi.org/10.2337/dc18-2585
Qi W, Li Q, Gordin D, King GL (2018) Preservation of renal function in chronic diabetes by enhancing glomerular glucose metabolism. J Mol Med (Berl) 96:373–381. https://doi.org/10.1007/s00109-018-1630-0
Qi W, Keenan HA, Li Q et al (2017) Pyruvate kinase M2 activation may protect against the progression of diabetic glomerular pathology and mitochondrial dysfunction. Nat Med 23:753–762. https://doi.org/10.1038/nm.4328
Perkins BA, Rabbani N, Weston A et al (2012) Serum levels of advanced glycation endproducts and other markers of protein damage in early diabetic nephropathy in type 1 diabetes. PLoS One 7:e35655. https://doi.org/10.1371/journal.pone.0035655
Jones CA, Krolewski AS, Rogus J, Xue JL, Collins A, Warram JH (2005) Epidemic of end-stage renal disease in people with diabetes in the United States population: do we know the cause? Kidney Int 67:1684–1691. https://doi.org/10.1111/j.1523-1755.2005.00265.x
Miller JA (1999) Impact of hyperglycemia on the renin angiotensin system in early human type 1 diabetes mellitus. J Am Soc Nephrol 10:1778–1785
Nosadini R, Velussi M, Brocco E et al (2006) Increased renal arterial resistance predicts the course of renal function in type 2 diabetes with microalbuminuria. Diabetes 55:234–239
Vervoort G, Wetzels JF, Lutterman JA, van Doorn LG, Berden JH, Smits P (1999) Elevated skeletal muscle blood flow in noncomplicated type 1 diabetes mellitus: role of nitric oxide and sympathetic tone. Hypertension 34:1080–1085. https://doi.org/10.1161/01.HYP.34.5.1080
Matsumoto N, Ishimura E, Taniwaki H et al (2000) Diabetes mellitus worsens intrarenal hemodynamic abnormalities in nondialyzed patients with chronic renal failure. Nephron 86:44–51. https://doi.org/10.1159/000045711
Ronnback M, Fagerudd J, Forsblom C, Pettersson-Fernholm K, Reunanen A, Groop PH (2004) Altered age-related blood pressure pattern in type 1 diabetes. Circulation 110:1076–1082. https://doi.org/10.1161/01.CIR.0000139903.29522.8D
Herbert KE, Mistry Y, Hastings R, Poolman T, Niklason L, Williams B (2008) Angiotensin II-mediated oxidative DNA damage accelerates cellular senescence in cultured human vascular smooth muscle cells via telomere-dependent and independent pathways. Circ Res 102:201–208. https://doi.org/10.1161/CIRCRESAHA.107.158626
Kunieda T, Minamino T, Nishi J et al (2006) Angiotensin II induces premature senescence of vascular smooth muscle cells and accelerates the development of atherosclerosis via a p21-dependent pathway. Circulation 114:953–960. https://doi.org/10.1161/CIRCULATIONAHA.106.626606
Cherney DZ, Reich HN, Miller JA et al (2010) Age is a determinant of acute hemodynamic responses to hyperglycemia and angiotensin II in humans with uncomplicated type 1 diabetes mellitus. Am J Physiol Regul Integr Comp Physiol 299:R206–R214
Lytvyn Y, Har R, Locke A et al (2017) Renal and Vascular Effects of Uric Acid Lowering in Normouricemic Patients With Uncomplicated Type 1 Diabetes. Diabetes 66:1939–1949
Lytvyn Y, Bjornstad P, Lovshin JA et al (2019) Association between uric acid, renal haemodynamics and arterial stiffness over the natural history of type 1 diabetes. Diabetes Obes Metab 21:1388–1398. https://doi.org/10.1111/dom.13665
Doria A, Galecki AT, Spino C et al (2020) Serum Urate Lowering with Allopurinol and Kidney Function in Type 1 Diabetes. N Engl J Med 382:2493–2503. https://doi.org/10.1056/NEJMoa1916624
Zelniker TA, Wiviott SD, Raz I et al (2019) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 393:31–39. https://doi.org/10.1016/S0140-6736(18)32590-X
Perkovic V, Jardine MJ, Neal B et al (2019) Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med 380:2295–2306. https://doi.org/10.1056/NEJMoa1811744
Cherney DZ, Perkins BA, Soleymanlou N et al (2014) Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 129:587–597. https://doi.org/10.1161/CIRCULATIONAHA.113.005081
Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ (2016) Sodium Glucose Cotransporter 2 Inhibitors in the Treatment of Diabetes Mellitus: Cardiovascular and Kidney Effects, Potential Mechanisms, and Clinical Applications. Circulation 134:752–772. https://doi.org/10.1161/CIRCULATIONAHA.116.021887
Bai JW, Boulet G, Halpern EM et al (2016) Cardiovascular disease guideline adherence and self-reported statin use in longstanding type 1 diabetes: results from the Canadian study of longevity in diabetes cohort. Cardiovasc Diabetol 15:14
Lovshin JA, Bjornstad P, Lovblom LE et al (2018) Atherosclerosis and Microvascular Complications: Results From the Canadian Study of Longevity in Type 1 Diabetes. Diabetes Care 41:2570–2578. https://doi.org/10.2337/dc18-1236
Theilade S, Rossing P, Jensen JS, Jensen MT (2018) Arterial-ventricular coupling in type 1 diabetes: arterial stiffness is associated with impaired global longitudinal strain in type 1 diabetes patients-the Thousand & 1 Study. Acta Diabetol 55:21–29. https://doi.org/10.1007/s00592-017-1062-2
Hjortebjerg R, Tarnow L, Jorsal A et al (2015) IGFBP-4 Fragments as Markers of Cardiovascular Mortality in Type 1 Diabetes Patients With and Without Nephropathy. J Clin Endocrinol Metab 100:3032–3040
Grauslund J, Jørgensen TM, Nybo M, Green A, Rasmussen LM, Sjølie AK (2010) Risk factors for mortality and ischemic heart disease in patients with long-term type 1 diabetes. J Diabetes Complicat 24:223–228
Conway BN, Aroda VR, Maynard JD et al (2012) Skin intrinsic fluorescence is associated with coronary artery disease in individuals with long duration of type 1 diabetes. Diabetes Care 35:2331–2336
Holte KB, Svanteson M, Hanssen KF, Haig Y, Solheim S, Berg TJ (2019) Undiagnosed coronary artery disease in long-term type 1 diabetes. The Dialong study. J Diabetes Complicat 33:383–389. https://doi.org/10.1016/j.jdiacomp.2019.01.006
Larsen J, Brekke M, Sandvik L, Arnesen H, Hanssen KF, Dahl-Jorgensen K (2002) Silent coronary atheromatosis in type 1 diabetic patients and its relation to long-term glycemic control. Diabetes 51:2637–2641. https://doi.org/10.2337/diabetes.51.8.2637
Orchard TJ, Olson JC, Erbey JR et al (2003) Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 26:1374–1379. https://doi.org/10.2337/diacare.26.5.1374
Pongrac Barlovic D, Harjutsalo V, Gordin D et al (2018) The Association of Severe Diabetic Retinopathy With Cardiovascular Outcomes in Long-standing Type 1 Diabetes: A Longitudinal Follow-up. Diabetes Care 41:2487–2494. https://doi.org/10.2337/dc18-0476
Turek SJ, Hastings SM, Sun JK, King GL, Keenan HA (2013) Sexual dysfunction as a marker of cardiovascular disease in males with 50 or more years of type 1 diabetes. Diabetes Care 36:3222–3226. https://doi.org/10.2337/dc13-0294
Vaisar T, Kanter JE, Wimberger J et al (2020) High Concentration of Medium-Sized HDL Particles and Enrichment in HDL Paraoxonase 1 Associate With Protection From Vascular Complications in People With Long-standing Type 1 Diabetes. Diabetes Care 43:178–186
Hernandez SL, Gong JH, Chen L et al (2014) Characterization of circulating and endothelial progenitor cells in patients with extreme-duration type 1 diabetes. Diabetes Care 37:2193–2201
Pop-Busui R, Boulton AJ, Feldman EL et al (2017) Diabetic Neuropathy: A Position Statement by the American Diabetes Association. Diabetes Care 40:136–154
Weisman A, Rovinski R, Farooqi MA et al (2016) Commonly Measured Clinical Variables Are Not Associated With Burden of Complications in Long-standing Type 1 Diabetes: Results From the Canadian Study of Longevity in Diabetes. Diabetes Care 39:e67–e68
Weisman A, Lovblom LE, Keenan HA et al (2018) Diabetes Care Disparities in Long-standing Type 1 Diabetes in Canada and the U.S.: A Cross-sectional Comparison. Diabetes Care 41:88–95
Cardinez N, Lovblom LE, Bai JW et al (2018) Sex differences in neuropathic pain in longstanding diabetes: Results from the Canadian Study of Longevity in Type 1 Diabetes. J Diabetes Complicat 32:660–664. https://doi.org/10.1016/j.jdiacomp.2018.05.001
Cardinez N, Lovblom LE, Orszag A, Bril V, Cherney DZ, Perkins BA (2019) Sex differences in neuropathy & neuropathic pain: A brief report from the Phase 2 Canadian Study of Longevity in Type 1 Diabetes. J Diabetes Complicat 33:107397. https://doi.org/10.1016/j.jdiacomp.2019.06.002
Bai JW, Lovblom LE, Cardinez M et al (2017) Neuropathy and presence of emotional distress and depression in longstanding diabetes: Results from the Canadian study of longevity in type 1 diabetes. J Diabetes Complicat 31:1318–1324. https://doi.org/10.1016/j.jdiacomp.2017.05.002
Musen G, Tinsley LJ, Marcinkowski KA et al (2018) Cognitive Function Deficits Associated With Long-Duration Type 1 Diabetes and Vascular Complications. Diabetes Care 41:1749–1756. https://doi.org/10.2337/dc17-1955
Gilsanz P, Albers K, Beeri MS, Karter AJ, Quesenberry CP Jr, Whitmer RA (2018) Traumatic brain injury associated with dementia risk among people with type 1 diabetes. Neurology 91:e1611–e1618
Lacy ME, Gilsanz P, Eng CW, Beeri MS, Karter AJ, Whitmer RA (2020) Recurrent diabetic ketoacidosis and cognitive function among older adults with type 1 diabetes: findings from the Study of Longevity in Diabetes. BMJ Open Diabetes Res Care 8. https://doi.org/10.1016/j.ajo.2020.12.001
Lacy ME, Gilsanz P, Karter AJ, Quesenberry CP, Pletcher MJ, Whitmer RA (2018) Long-term Glycemic Control and Dementia Risk in Type 1 Diabetes. Diabetes Care 41:2339–2345. https://doi.org/10.2337/dc18-0073
Lacy ME, Gilsanz P, Eng C, Beeri MS, Karter AJ, Whitmer RA (2020) Severe Hypoglycemia and Cognitive Function in Older Adults With Type 1 Diabetes: The Study of Longevity in Diabetes (SOLID). Diabetes Care 43:541–548. https://doi.org/10.2337/dc19-0906
Gilsanz P, Lacy ME, Beeri MS, Karter AJ, Eng CW, Whitmer RA (2020) Sleep Quality and Cognitive Function in Type 1 Diabetes: Findings From the Study of Longevity in Diabetes (SOLID). Alzheimer Dis Assoc Disord 34:18–24
Eng CW, Gilsanz P, Lacy ME, Beeri MS, Whitmer RA (2020) Locus of Control and Cognition in Older Adults With Type 1 Diabetes: Evidence For Sex Differences From the Study of Longevity in Diabetes (SOLID). Alzheimer Dis Assoc Disord 34:25–30
The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group et al (2007) Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med 356:1842–1852. https://doi.org/10.1056/NEJMoa066397
Jacobson AM, Ryan CM, Cleary PA et al (2011) Biomedical risk factors for decreased cognitive functioning in type 1 diabetes: an 18 year follow-up of the Diabetes Control and Complications Trial (DCCT) cohort. Diabetologia 54:245–255. https://doi.org/10.1007/s00125-010-1883-9
Schreur V, van Asten F, Ng H et al (2018) Risk factors for development and progression of diabetic retinopathy in Dutch patients with type 1 diabetes mellitus. Acta Ophthalmol 96:459–464. https://doi.org/10.1111/aos.13815
Lee R, Wong TY, Sabanayagam C (2015) Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond) 2:17
Klein R, Knudtson MD, Lee KE, Gangnon R, Klein BE (2009) The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXIII: the twenty-five-year incidence of macular edema in persons with type 1 diabetes. Ophthalmology 116:497–503. https://doi.org/10.1016/j.ophtha.2008.10.016
Lovshin JA, Lytvyn Y, Lovblom LE et al (2019) Retinopathy and RAAS Activation: Results From the Canadian Study of Longevity in Type 1 Diabetes. Diabetes Care 42:273–280. https://doi.org/10.2337/dc18-1809
Klein BEK, Horak KL, Maynard JD, Lee KE, Klein R (2017) Association of Skin Intrinsic Fluorescence with Retinal Microvascular Complications of Long Term Type 1 Diabetes in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmic Epidemiol 24:211–216. https://doi.org/10.1080/09286586.2016.1269934
Yokomizo H, Maeda Y, Park K et al (2019) Retinol binding protein 3 is increased in the retina of patients with diabetes resistant to diabetic retinopathy. Sci Transl Med 11:eaau6627
Fickweiler W, Aiello LP, Sun JK, King GL (2019) Retinol binding protein 3 as biomarker for diabetic retinopathy. Ann Transl Med 7:706. https://doi.org/10.21037/atm.2019.10.95
Marsh S, Nakhoul FM, Skorecki K et al (2000) Hypoxic induction of vascular endothelial growth factor is markedly decreased in diabetic individuals who do not develop retinopathy. Diabetes Care 23:1375–1380. https://doi.org/10.2337/diacare.23.9.1375
Bhatt S, Gupta MK, Khamaisi M et al (2015) Preserved DNA Damage Checkpoint Pathway Protects against Complications in Long-Standing Type 1 Diabetes. Cell Metab 22:239–252. https://doi.org/10.1016/j.cmet.2015.07.015
Alhuzaim ON, Lewis EJH, Lovblom LE et al (2019) Bone mineral density in patients with longstanding type 1 diabetes: Results from the Canadian Study of Longevity in Type 1 Diabetes. J Diabetes Complicat 33:107324
Maddaloni E, D’Eon S, Hastings S et al (2017) Bone health in subjects with type 1 diabetes for more than 50 years. Acta Diabetol 54:479–488. https://doi.org/10.1007/s00592-017-0973-2
Biragova MS, Gracheva SA, Glazunova AM et al (2016) The role of mineral and bone disorders in the development and progression of cardiac and renal pathology in patients with type 1 diabetes mellitus of long duration. Diabetes Res Clin Pract 118:29–37. https://doi.org/10.1016/j.diabres.2016.04.049
Holte KB, Juel NG, Brox JI et al (2017) Hand, shoulder and back stiffness in long-term type 1 diabetes; cross-sectional association with skin collagen advanced glycation end-products. The Dialong study. J Diabetes Complicat 31:1408–1414
Keenan HA, Costacou T, Sun JK et al (2007) Clinical factors associated with resistance to microvascular complications in diabetic patients of extreme disease duration: the 50-year medalist study. Diabetes Care 30:1995–1997. https://doi.org/10.2337/dc06-2222
Bain SC, Gill GV, Dyer PH et al (2003) Characteristics of Type 1 diabetes of over 50 years duration (the Golden Years Cohort). Diabet Med 20:808–811. https://doi.org/10.1046/j.1464-5491.2003.01029.x
Prior SL, Tang TS, Gill GV, Bain SC, Stephens JW (2011) Adiponectin, total antioxidant status, and urine albumin excretion in the low-risk “Golden Years” type 1 diabetes mellitus cohort. Metab Clin Exp 60:173–179. https://doi.org/10.1016/j.metabol.2009.12.008
Gordin D, Harjutsalo V, Tinsley L et al (2018) Differential Association of Microvascular Attributions With Cardiovascular Disease in Patients With Long Duration of Type 1 Diabetes. Diabetes Care 41:815–822. https://doi.org/10.2337/dc17-2250
Juel NG, Brox JI, Brunborg C, Holte KB, Berg TJ (2017) Very High Prevalence of Frozen Shoulder in Patients With Type 1 Diabetes of ≥45 Years’ Duration: The Dialong Shoulder Study. Arch Phys Med Rehabil 98:1551–1559. https://doi.org/10.1016/j.apmr.2017.01.020
Guo J, Naimi AI, Brooks MM, Muldoon MF, Orchard TJ, Costacou T (2020) Mediation analysis for estimating cardioprotection of longitudinal RAS inhibition beyond lowering blood pressure and albuminuria in type 1 diabetes. Ann Epidemiol 41:7–13.e11. https://doi.org/10.1016/j.annepidem.2019.12.004
Braffett BH, Dagogo-Jack S, Bebu I et al (2019) Association of Insulin Dose, Cardiometabolic Risk Factors, and Cardiovascular Disease in Type 1 Diabetes During 30 Years of Follow-up in the DCCT/EDIC Study. Diabetes Care 42:657–664. https://doi.org/10.2337/dc18-1574
Otani T, Kasahara T, Miura J, Uchigata Y, Babazono T (2019) Clinical background of Japanese patients with type 1 diabetes mellitus who have received insulin therapy for 50 years or longer. Diabetol Int 10:288–294. https://doi.org/10.1007/s13340-019-00393-x
Bjornstad P, Lovshin JA, Lytvyn Y et al (2018) Adiposity Impacts Intrarenal Hemodynamic Function in Adults With Long-standing Type 1 Diabetes With and Without Diabetic Nephropathy: Results From the Canadian Study of Longevity in Type 1 Diabetes. Diabetes Care 41:831–839. https://doi.org/10.2337/dc17-2475
Bjornstad P, Singh SK, Snell-Bergeon JK et al (2019) The relationships between markers of tubular injury and intrarenal haemodynamic function in adults with and without type 1 diabetes: Results from the Canadian Study of Longevity in Type 1 Diabetes. Diabetes Obes Metab 21:575–583. https://doi.org/10.1111/dom.13556
Boulet G, Halpern EM, Lovblom LE et al (2016) Prevalence of Insulin Pump Therapy and Its Association with Measures of Glycemic Control: Results from the Canadian Study of Longevity in Type 1 Diabetes. Diabetes Technol Ther 18:298–307. https://doi.org/10.1089/dia.2015.0216
Distiller LA, Joffe BI, Melville V, Welman T, Distiller GB (2006) Carotid artery intima-media complex thickening in patients with relatively long-surviving type 1 diabetes mellitus. J Diabetes Complicat 20:280–284. https://doi.org/10.1016/j.jdiacomp.2005.07.012
Mäkimattila S, Ylitalo K, Schlenzka A et al (2002) Family histories of Type II diabetes and hypertension predict intima-media thickness in patients with Type I diabetes. Diabetologia 45:711–718. https://doi.org/10.1007/s00125-002-0817-6
Acknowledgements
We wish to thank the many inspiring participants who have taken part in studies that focus on longstanding type 1 diabetes survivorship. For the Canadian Study of Longevity in Type 1 Diabetes project, we thank our key study co-investigators: G. Boulet (L’Université de Laval); J. Lovshin, M. H. Brent, N. Paul and V. Bril (all at the University Health Network); and H. A. Keenan (Joslin Diabetes Center). We thank E. M. Halpern, D. Eldelekli (Lunenfeld-Tanenbaum Research Institute) and G. Boulet (L’Université de Laval) for their valuable recruitment work, including translation for our French-speaking participants.
Authors’ relationships and activities
BAP has received speaker honoraria from Abbott, Medtronic, Insulet and Novo-Nordisk, research support to his research institute from Boehringer Ingelheim and the Bank of Montreal (BMO), and has served as a consultant to Boehringer Ingelheim, Abbott and Novo-Nordisk. LEL receives support from a CIHR Canada Graduate Scholarship Doctoral Award. DZIC is supported by a Department of Medicine, University of Toronto Merit Award and receives support from the CIHR, Diabetes Canada and the Heart and Stroke Richard Lewar Centre of Excellence. All other authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
We acknowledge the support from Diabetes Canada and JDRF Canada (grant no. 17-2013-312) and its Canadian Clinical Trial Network, BMO (the Bank of Montreal), and Boehringer Ingelheim, as well as Randy and Jenny Frisch and The Harvey and Annice Frisch Family Fund, the contributions of David and Jill Wright, and the Menkes Family Fund. BAP is grateful for funding from the Sam and Judy Pencer Family Chair in Diabetes Clinical Research.
Author information
Authors and Affiliations
Contributions
All authors were responsible for drafting the article and revising it critically for important intellectual content. All authors approved the version to be published.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Slideset of figures
(PPTX 273 kb)
Rights and permissions
About this article
Cite this article
Perkins, B.A., Lovblom, L.E., Lanctôt, S.O. et al. Discoveries from the study of longstanding type 1 diabetes. Diabetologia 64, 1189–1200 (2021). https://doi.org/10.1007/s00125-021-05403-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05403-9