Abstract
Purpose
The objective of this study was to clarify the clinical value of the posterior cruciate ligament index (PCLI) in anterior cruciate ligament (ACL) rupture, to explore the relationship between the PCLI and course of disease, and to identify the influencing factors of the PCLI.
Methods
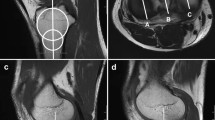
The PCLI was defined a quotient of the X (the tibial and femoral PCL attachments) and the Y (the maximum perpendicular distance from X to the PCL). A total of 858 patients were enrolled in this case–control study, including 433 patients with ACL ruptures who were assigned to the experimental group and 425 patients with meniscal tears (MTs) who were allocated to the control group. Some patients in the experimental group have collateral ligament rupture (CLR). Information, such as the patient’s age, sex, and course of disease, was recorded. All patients underwent magnetic resonance imaging (MRI) preoperatively, and the diagnosis was confirmed with the aid of arthroscopy. The PCLI and the depth of the lateral femoral notch sign (LFNS) were calculated based on the MRI findings, and the characteristics of the PCLI were explored.
Results
The PCLI in the experimental group (5.1 ± 1.6) was significantly smaller than that in the control group (5.8 ± 1.6) (P < 0.05). The PCLI gradually decreased with time and was only 4.8 ± 1.4 in patients in the chronic phase (P < 0.05). This change was not due to the decrease in X but rather the increase in Y. The results also showed that the PCLI was not related to the depth of the LFNS or injuries of other structures in the knee joint. Furthermore, when the optimal cut-off point of the PCLI was 5.2 (area under the curve = 71%), the specificity and the sensitivity were 84% and 67%, respectively, but the Youden index was just 0.3 (P < 0.05).
Conclusion
The PCLI decreases due to the increase in Y instead of the decrease in X with time, especially in the chronic phase. The change in X in this process may be offset during imaging. In addition, there are fewer influencing factors that lead to changes in the PCLI. Therefore, it can be used as a reliable indirect sign of ACL rupture. However, it is difficult to quantify the diagnostic criteria of the PCLI in clinical practice. Thus, the PCLI as a reliable indirect sign of ACL rupture is associated with the course of knee joint injury, and it can be used to describe the instability of the knee joint.
Levels of evidence
III.


Similar content being viewed by others
Availability of data and material
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Berthold D, Muench L, Herbst E, Mayr F, Chadayammuri V, Imhoff A et al (2021) High prevalence of a deep lateral femoral notch sign in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 29:1018–1024
Boeree N, Ackroyd C (1992) Magnetic resonance imaging of anterior cruciate ligament rupture. A new diagnostic sign. J Bone Joint Surg Br 74:614–616
Bonanzinga T, Grassi A, Altomare D, Lucidi G, Macchiarola L, Zaffagnini S et al (2022) High return to sport rate and few re-ruptures at long term in professional footballers after anterior cruciate ligament reconstruction with hamstrings. Knee Surg Sports Traumatol Arthrosc 30:3681–3688
Burgers PT, Den Hollander PH (2016) A typical sign on a plain knee radiograph. BMJ 355:i6021
Chen J, Xu C, Cho E, Huangfu X, Zhao J (2021) Reconstruction for chronic ACL tears with or without anterolateral structure augmentation in patients at high risk for clinical failure: a randomized clinical trial. J Bone Joint Surg Am 103:1482–1490
Diermeier T, Rothrauff B, Engebretsen L, Lynch A, Ayeni O, Paterno M et al (2020) Treatment after anterior cruciate ligament injury: panther symposium ACL treatment consensus group. Knee Surg Sports Traumatol Arthrosc 28:2390–2402
Dimitriou D, Reimond M, Foesel A, Baumgaertner B, Zou D, Tsai TY et al (2020) The deep lateral femoral notch sign: a reliable diagnostic tool in identifying a concomitant anterior cruciate and anterolateral ligament injury. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06278-w
Flint J, Wade A, Giuliani J, Rue J (2014) Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med 42:235–241
Gong H, Wang H, Zhang X, Fu L, Chen L (2022) Diagnostic value of the lateral femoral notch sign and kissing contusion in patients with anterior cruciate ligament injuries: a case-control study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04366-9
Hassebrock J, Gulbrandsen M, Asprey W, Makovicka J, Chhabra A (2020) Knee ligament anatomy and biomechanics. Sports Med Arthrosc Rev 28:80–86
Herbst E, Hoser C, Tecklenburg K, Filipovic M, Dallapozza C, Herbort M et al (2015) The lateral femoral notch sign following ACL injury: frequency, morphology and relation to meniscal injury and sports activity. Knee Surg Sports Traumatol Arthrosc 23:2250–2258
Huang H, Nagao M, Nishio H, Kaneko H, Saita Y, Takazawa Y et al (2021) Remnant preservation provides good clinical outcomes after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 29:3763–3772
Huang T, Liu Z, Hong C, Wang C, Hsu K, Kuan F et al (2022) The lateral femoral notch sign and coronal lateral collateral ligament sign in magnetic resonance imaging failed to predict dynamic anterior tibial laxity. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-022-05368-9
Karnuta J, Dalton S, Bena J, Farrow L, Featherall J, Jones M et al (2021) Do narcotic use, physical therapy location, or payer type predict patient-reported outcomes after anterior cruciate ligament reconstruction? Orthop J Sports Med 9:2325967121994833
Kennedy M, Strauss M, LaPrade R (2020) Injury of the meniscus root. Clin Sports Med 39:57–68
Korthaus A, Warncke M, Pagenstert G, Krause M, Frosch K, Kolb JP et al (2022) Lateral femoral notch sign and posterolateral tibial plateau fractures and their associated injuries in the setting of an anterior cruciate ligament rupture. Arch Orthop Trauma Surg 142:1605–1612
Kumaki D, Tensho K, Iwaya M, Iwaasa T, Yoshida K, Koyama S et al (2022) Macroscopic and microscopic findings of multi-folded hamstring grafts of anatomical double-bundle ACL reconstruction 13 years after surgery. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07185-y
LaPrade C, Civitarese D, Rasmussen M, LaPrade R (2015) Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med 43:3077–3092
Lasmar R, Marques de Almeida A, Serbino J, Mota Albuquerque R, Hernandez A (2010) Importance of the different posterolateral knee static stabilizers: biomechanical study. Clinics (Sao Paulo) 65:433–440
Liu S, Osti L, Dorey F, Yao L (1994) Anterior cruciate ligament tear. A new diagnostic index on magnetic resonance imaging. Clin Orthop 302:147–150
Lucidi G, Grassi A, Di Paolo S, Agostinone P, Neri M, Macchiarola L et al (2021) The lateral femoral notch sign is correlated with increased rotatory laxity after anterior cruciate ligament injury: pivot shift quantification with a surgical navigation system. Am J Sports Med 49:649–655
Macchiarola L, Pizza N, Patania V, Grassi A, Dal Fabbro G, Marcacci M et al (2023) Double-bundle non-anatomic ACL revision reconstruction with allograft resulted in a low revision rate at 10 years. Knee Surg Sports Traumatol Arthrosc 31:340–348
Markolf K, Mensch J, Amstutz H (1976) Stiffness and laxity of the knee–the contributions of the supporting structures. A quantitative in vitro study. J Bone Joint Surg Am 58:583–594
Mather R, Koenig L, Kocher M, Dall T, Gallo P, Scott D et al (2013) Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am 95:1751–1759
Naraghi A, Gupta S, Jacks L, Essue J, Marks P, White L (2012) Anterior cruciate ligament reconstruction: MR imaging signs of anterior knee laxity in the presence of an intact graft. Radiology 263:802–810
Ni QK, Wang XP, Guo Q, Li M, Liu N, Zhang H (2022) High-grade pivot-shift phenomenon after anterior cruciate ligament injury is associated with asymmetry of lateral and medial compartment anterior tibial translation and lateral meniscus posterior horn tears. Knee Surg Sports Traumatol Arthrosc 30:3700–3707
Øiestad B, Engebretsen L, Storheim K, Risberg M (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37:1434–1443
Roberts D, Ageberg E, Andersson G, Fridén T (2007) Clinical measurements of proprioception, muscle strength and laxity in relation to function in the ACL-injured knee. Knee Surg Sports Traumatol Arthrosc 15:9–16
Siwiński D, Ziemiański A (1998) Value of posterior cruciate ligament index in the diagnosis of anterior cruciate ligament injuries. Arch Orthop Trauma Surg 118:116–118
Sokal P, Norris R, Maddox T, Oldershaw R (2022) The diagnostic accuracy of clinical tests for anterior cruciate ligament tears are comparable but the Lachman test has been previously overestimated: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30:3287–3303
Theunissen W, van der Steen M, Liu W, Janssen R (2020) Timing of anterior cruciate ligament reconstruction and preoperative pain are important predictors for postoperative kinesiophobia. Knee Surg Sports Traumatol Arthrosc 28:2502–2510
Tung G, Davis L, Wiggins M, Fadale P (1993) Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology 188:661–667
von Essen C, Cristiani R, Lord L, Stålman A (2022) Subsequent surgery after primary ACLR results in a significantly inferior subjective outcome at a 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 30:1927–1936
Willinger L, Balendra G, Pai V, Lee J, Mitchell A, Jones M et al (2022) High incidence of superficial and deep medial collateral ligament injuries in “isolated” anterior cruciate ligament ruptures: a long overlooked injury. Knee Surg Sports Traumatol Arthrosc 30:167–175
Zakharia A, Lameire D, Abdel Khalik H, Kay J, Uddandam A, Nagai K et al (2022) Quadriceps tendon autograft for pediatric anterior cruciate ligament reconstruction results in promising postoperative function and rates of return to sports: a systematic review. Knee Surg Sports Traumatol Arthrosc 30:3659–3672
Zampeli F, Ntoulia A, Giotis D, Stavros R, Mitsionis G, Pappas E et al (2014) The PCL index is correlated with the control of rotational kinematics that is achieved after anatomic anterior cruciate ligament reconstruction. Am J Sports Med 42:665–674
Zbrojkiewicz D, Vertullo C, Grayson J (2018) Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med J Aust 208:354–358
Acknowledgements
Thanked Prof. Lin Chen for her advice and help in this study. Thanked my beloved girlfriend PhD. Danyu Chen for her contribution to this research, and will you marry me?
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
HG contributed to the article writing and data collection. QL and YL contributed to some imaging data and surgery. KH and WZ contributed to part of the statistics of the article. YL, GS and XP directed the writing of the article. YY designed the study and was responsible for the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the ethical committee of Suining Central Hospital (LLSLH20220063).
Informed consent
Our study only involves the image information of patients. It is not necessary to obtain consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gong, H., Li, Q., Len, Y. et al. The posterior cruciate ligament index as a reliable indirect sign of anterior cruciate ligament rupture is associated with the course of knee joint injury. Knee Surg Sports Traumatol Arthrosc 31, 3277–3283 (2023). https://doi.org/10.1007/s00167-023-07357-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07357-4