Abstract
Introduction and hypothesis
Women who perform high-impact activities might be at greater risk of pelvic floor dysfunction (PFD) than those participating in low-impact exercise; however, little is known about whether PFD is more common in one type of high-impact activity than another. The aim of this study was to compare the prevalence of PFD symptoms in women who engage in high-impact activity compared with CrossFit®-brand training (CF).
Methods
An online survey collected data from 1,379 women (521 runners, 858 CF) on exercise participation, parity, and PFD symptoms, via the Pelvic Floor Distress Inventory (PFDI-20). Specific questions from each PFDI-20 subscale further investigated symptoms of pelvic organ prolapse (POP), anal incontinence (AI), as well as stress (SUI) and urgency (UUI) urinary incontinence.
Results
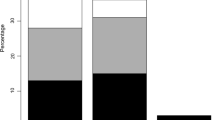
Symptoms of POP and AI were significantly higher in runners (POP 12.7%, AI 34.0%) than in CF (POP 7.8%, p = 0.003; AI 27.7%, p = 0.014). There was no significant difference in SUI symptoms between groups (37.0% vs 41.0% respectively, p = 0.141). Vaginally parous runners reported significantly more symptoms of POP (19.0% vs 12.2%, p = 0.023), AI (39.3% vs 27.2%, p = 0.001), and UUI (36.3% vs 29.0%, p = 0.037) than CF.
Conclusion
Women, particularly parous women, who participate in running, have a higher prevalence of POP and AI symptoms than women who participate in CF. This suggests that CrossFit®-brand training might not be more detrimental to PFD symptoms than other high-impact activity, such as running. This study does not conclude a pelvic floor health benefit of one exercise over another, but highlights that exercise options can be provided to women.


Similar content being viewed by others
References
Bø K, Nygaard IE. Is physical activity good or bad for the female pelvic floor? A narrative review. Sports Med. 2019;50(3):471–84.
Shaw JM, Hamad NM, Coleman TJ, Egger MJ, Hsu Y, Hitchcock R, et al. Intra-abdominal pressures during activity in women using an intra-vaginal pressure transducer. J Sports Sci. 2014;32(12):1176–85.
Teixeira RV, Colla C, Sbruzzi G, Mallmann A, Paiva LL. Prevalence of urinary incontinence in female athletes: a systematic review with meta-analysis. Int Urogynecol J. 2018;29(12):1717–25.
O’Dell KK, Morse AN, Crawford SL, Howard A. Vaginal pressure during lifting, floor exercises, jogging, and use of hydraulic exercise machines. Int Urogynecol J. 2007;18(12):1481–9.
Dietze-Hermosa M, Hitchcock R, Nygaard IE, Shaw JM. Intra-abdominal pressure and pelvic floor health: should we be thinking about this relationship differently? Female Pelvic Med Reconstr Surg. 2020;26(7):409–14.
Wikander L, Cross D, Gahreman DE. Prevalence of urinary incontinence in women powerlifters: a pilot study. Int Urogynecol J 2019;30(12):2031–9.
Brown WJ, Bauman AE, Bull FC, Burton NW. Development of evidence-based physical activity recommendations for adults (18–64 years). Report prepared for the Australian Government Department of Health [Internet]. Canberra ACT: Commonwealth of Australia; 2012. Accessed 12 September 2019. Available from: https://www.health.gov.au/internet/main/publishing.nsf/Content/F01F92328EDADA5BCA257BF0001E720D/$File/DEB-PAR-Adults-18-64years.pdf.
Schmitz KH, Williams NI, Kontos D, Domchek S, Morales KH, Hwang W-T, et al. Dose–response effects of aerobic exercise on estrogen among women at high risk for breast cancer: a randomized controlled trial. Breast Cancer Res Treat. 2015;154(2):309–18.
Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR. High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial. J Bone Miner Res. 2018;33(2):211–20.
Alicea SK, Parrott AD, Manos TM, Kwon YS. Comparison of the affective responses to continuous training and High-intensity interval training protocols: application of the dual-mode model. J Strength Cond Res. 2020. https://doi.org/10.1519/JSC.0000000000003282.
CrossFit, Inc. CrossFit Games: Open Leaderboard [Internet]. USA: 2011. Accessed 1 Sept September 2019. Available from: https://games.crossfit.com/leaderboard/open/2019?view=0&division=2&scaled=0&sort=0.
Forner LB, Beckman EM, Smith MD. Symptoms of pelvic organ prolapse in women who lift heavy weights for exercise: a cross-sectional survey. Int Urogynecol J 2019;31(8):1551–8.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13.
World Health Organization. Obesity: preventing and managing the global epidemic [Internet]. Geneva Switzerland: WHO; 2000. Accessed 1 December 2019. Available from: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/.
Tegerstedt G, Maehle-Schmidt M, Nyrén O, Hammarström M. Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J. 2005;16(6):497–503.
Sultan AH, Monga A, Lee J, Emmanuel A, Norton C, Santoro G, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female anorectal dysfunction. Int Urogynecol J. 2017;28(1):5–31.
Haylen BT, de RD, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Gafni-Kane A, Goldberg RP, Sand PK, Botros SM. Enhanced interpretability of the PFDI-20 with establishment of reference scores among women in the general population. Neurourol Urodyn. 2012;31(8):1252–7.
Brennand E, Ruiz-Mirazo E, Tang S, Kim-Fine S. Urinary leakage during exercise: problematic activities, adaptive behaviors, and interest in treatment for physically active Canadian women. Int Urogynecol J. 2018;29(4):497–503.
High R, Thai K, Virani H, Kuehl T, Danford J. Prevalence of pelvic floor disorders in female CrossFit athletes. Female Pelvic Med Reconstr Surg. 2019;26(8):498–502..
Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654.
Yi J, Tenfelde S, Tell D, Brincat C, Fitzgerald C. Triathlete risk of pelvic floor disorders, pelvic girdle pain, and female athlete triad. Female Pelvic Med Reconstr Surg. 2016;22(5):373–6.
Srikanthan P, Horwich TB, Tseng CH. Relation of muscle mass and fat mass to cardiovascular disease mortality. Am J Cardiol. 2016;117(8):1355–60.
Vitton V, Baumstarck-Barrau K, Brardjanian S, Caballe I, Bouvier M, Grimaud J-C. Impact of high-level sport practice on anal incontinence in a healthy young female population. J Womens Health. 2011;20(5):757–63.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6.
De Oliveira EP, Burini RC, Jeukendrup A. Gastrointestinal complaints during exercise: prevalence, etiology, and nutritional recommendations. Sports Med. 2014;44(Suppl 1):79–85.
Yang J, Cheng JW, Wagner H, Lohman E, Yang SH, Krishingner GA, et al. The effect of high impact crossfit exercises on stress urinary incontinence in physically active women. Neurourol Urodyn. 2019;38(2):749–56.
Elks W, Jaramillo-Huff A, Barnes KL, Petersen TR, Komesu YM. The stress urinary incontinence in CrossFit (SUCCeSS) study. Female Pelvic Med Reconstr Surg. 2020;26(2):101–6.
Salvatore S, Serati M, Laterza R, Uccella S, Torella M, Bolis P-F. The impact of urinary stress incontinence in young and middle-age women practising recreational sports activity: an epidemiological study. Br J Sports Med. 2009;43(14):1115–8.
Dobrowolski SL, Pudwell J, Harvey M-A. Urinary incontinence among competitive rope-skipping athletes: a cross-sectional study. Int Urogynecol J 2019;31(5):881–6.
Jelovsek J, Barber M, Karram M, Walters M, Paraiso M. Randomised trial of laparoscopic Burch colposuspension versus tension-free vaginal tape: long-term follow up. BJOG. 2007;115(2):219–25.
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. J Clin Epidemiol. 2000;53(11):1150–7.
Mannella P, Palla G, Bellini M, Simoncini T. The female pelvic floor through midlife and aging. Maturitas. 2013;76(3):230–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Author L.B. Forner is a private practice physiotherapist and has accepted brand ambassador fees for Procter and Gamble Australia. Authors E.M. Beckman and M.D. Smith declare that they have no conflicts of interest.
Financial disclaimer
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Forner, L.B., Beckman, E.M. & Smith, M.D. Do women runners report more pelvic floor symptoms than women in CrossFit®? A cross-sectional survey. Int Urogynecol J 32, 295–302 (2021). https://doi.org/10.1007/s00192-020-04531-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04531-x