Abstract
Introduction and hypothesis
The vaginal pessary is a conservative method for treating pelvic organ prolapse (POP). It is able to reduce symptoms with minimal complications, improving quality of life (QOL). This study’s hypothesis was that the use of pessaries decreases quantitative measures and improves women’s QOL. We aimed to evaluate the effects of the use of a ring pessary on the quantitative measurements of POP by the Pelvic Organ Prolapse Quantification (POP-Q) and on QOL.
Methods
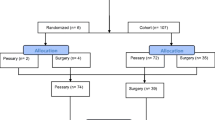
Prospective cohort study divided in two stages. In stage I POP-Q and QOL were assessed prior to the use of the ring pessary and in stage II after its use for at least 4 months with pessary removal 72 h before clinical evaluation. Wilcoxon tests were performed for necessary comparisons and Spearman’s tests for calculating correlations.
Results
One hundred thirty-six women were evaluated, of which 50 were included. There was a decrease in POP in at least one of the vaginal compartments in the women included. When assessing individual measures (Ba, Bp and C), reductions in all measures were observed. There was also an improvement in the general and specific quality of life of women.
Conclusion
The ring pessary proved to be a good therapeutic option, with a reduction in POP-Q measurements and/or absence of POP progression in the short term and an improvement in women’s QOL.




Similar content being viewed by others
References
Abrams P, Cardoso L, Khoury S, Wein A. Incontinence. Tokyo: ICUD; 2017.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2009;194:1455–61. https://doi.org/10.1016/j.ajog.2006.01.060.
Coelho SCA, Castro EB, Juliato CR. Female pelvic organ prolapse using pessaries: systematic review. Int Urogynecol J. 2016;27:1797–803. https://doi.org/10.1007/s00192-016-2991-y.
Jones KA, Shepherd JP, Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in inpatient prolapse procedures in the United States, 1979-2006. Am J Obstet Gynecol. 2010;202:501–7. https://doi.org/10.1016/j.ajog.2010.01.017.
Yang JF, Han JS, Zhu FL, Wang YT, Yao Y, Qiao J. Clinical study on silicone pessary in the treatment of pelvic organ prolapse. Zhonghua Fu Chan Ke Za Zhi. 2012;47:487–91.
Babet HCL, Bart MWB, Alfredo LM. Pessary treatment for pelvic organ prolapse and health-related quality of life: a review. Int Urogynecol J. 2011;22:637–44.
Komesu YM, Rogers RG, Rode MA, Craig EC, Schrader RM, Gallegos KA, et al. Patient-selected goal attainment for pessary wearers: what is the clinical relevance? Am J Obstet Gynecol. 2008;198:577577. https://doi.org/10.1016/j.ajog.2007.12.033.
Patel M, Mellen C, O’Sullivan DM, LaSala CA. Impact of pessary use on prolapse symptoms, quality of life, and body image. Am J Obstet Gynecol. 2010;202:1–4. https://doi.org/10.1097/SPV.0b013e31823a8186.
Jones K, Yang L, Lowder JL, Meyn L, Ellison R, Zyczynski HM, et al. Effect of pessary use on genital hiatus measurements in women with pelvic organ prolapse. Obstet Gynecol. 2008;112:630–6. https://doi.org/10.1097/AOG.0b013e318181879f.
Handa VL, Jones M. Do pessaries prevent the progression of pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:349–51.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Ciconelli RM, Ferraz MB, Santos N, Meinão I, Quaresma MR. Tradução para a língua portuguesa do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36). Rev Bras Reumatol. 1994;39:143–50.
Oliveira MS, Tamanini JTN, Cavalcanti GA. Validation of the prolapse quality-of-life questionnaire (P-QOL) in Portuguese version in Brazilian women. Int Urogynecol J. 2009;20:1191–202. https://doi.org/10.1007/s00192-009-0934-6.
Hall A, Theofrastous J, Cundiff G, Harris R, Hamilton L, Swift S, et al. Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol. 1966;175:1467–71.
Matsubara S, Ohki Y. Can a ring pessary have a lasting effect to reverse uterine prolapse even after its removal? J Obstet Gynaecol Res. 2010;36:459–61.
Clemons JL (2008). Vaginal pessary treatment of prolapse and incontinence. Up-To-Date https://www.uptodate.com/contents/vaginal-pessaries-indications-devices-and-approach-to-selection. Accessed 10 January 2020.
Manchana T, Bunyavejchevin S. Impact on quality of life after ring pessary use for pelvic organ prolapse. Int Urogynecol J. 2012;23:873–7. https://doi.org/10.1007/s00192-011-1634-6.
Coelho SCA, Marangoni-Junior M, Brito LGO, Castro EB, Juliato CRT. Quality of life and vaginal symptoms of postmenopausal women using pessary for pelvic organ prolapse: a prospective study. Rev Assoc Med Bras. 2018;64:1103–7. https://doi.org/10.1590/1806-9282.64.12.1103.
Komesu YM, Rogers RG, Rode MA, Craig EC, Gallegos KA, Montoya AR, et al. Pelvic floor symptom changes in pessary users. Am J Obstet Gynecol. 2007;197:1–6.
Lamers BH, Broekman BM, Milani AL. Pessary treatment for pelvic organ prolapse and health-related quality of life: a review. Int Urogynecol J. 2011;22:637–44. https://doi.org/10.1007/s00192-011-1390-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mendes, L.C., Bezerra, L.R.P.S., Bilhar, A.P.M. et al. Symptomatic and anatomic improvement of pelvic organ prolapse in vaginal pessary users. Int Urogynecol J 32, 1023–1029 (2021). https://doi.org/10.1007/s00192-020-04540-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04540-w