Abstract
Summary
EOS biplane radiographs of 117 subjects between 20 and 83 years were analyzed to compute the upper body lever arm over the L1 vertebra and its impact on vertebral strength. Postural sagittal alignment alteration was observed with age and resulted in a greater lever arm causing vertebral strength to decrease.
Purpose
The purpose of this study was to analyze the impact of postural alignment changes with age on vertebral strength using finite element analysis and barycentremetry.
Methods
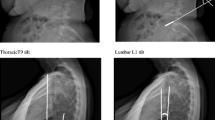
A total of 117 subjects from 20 to 83 years were divided in three age groups: young (20 to 40 years, 62 subjects), intermediate (40 to 60 years, 26 subjects), and elderly (60 years and over, 29 subjects). EOS biplane radiographs were acquired, allowing 3D reconstruction of the spine and body envelope as well as spinal, pelvic, and sagittal alignment parameter measurements. A barycentremetry method allowed the estimation of the mass and center of mass (CoM) position of the upper body above L1, relatively to the center of the L1 vertebra (lever arm). To investigate the effect of this lever arm, vertebral strength of a generic finite element model (with constant geometry and mechanical properties for all subjects) was successively computed applying the personalized lever arm of each subject.
Results
A combination of an increase in thoracic kyphosis, cervical lordosis, and pelvic tilt with a loss of lumbar lordosis was observed between the young and the older groups. Sagittal alignment parameters indicated a more forward position as age increased. The lever arm of the CoM above L1 varied from an average of 1 mm backward for the young group, to averages of 10 and 24 mm forward, respectively, for the intermediate and elderly group. As a result, vertebral strength decreased from 2527 N for the young group to 1820 N for the elderly group.
Conclusion
The global sagittal alignment modifications observed with age were consistent with the literature. Posture alteration with age reduced vertebral strength significantly in this simplified loading model. Postural alignment seems essential to be considered in the evaluation of osteoporotic patients.




Similar content being viewed by others
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Bliuc D, Nguyen ND, Milch VE et al (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521. https://doi.org/10.1001/jama.2009.50
Löffler MT, Jacob A, Valentinitsch A et al (2019) Improved prediction of incident vertebral fractures using opportunistic QCT compared to DXA. Eur Radiol 29:4980–4989. https://doi.org/10.1007/s00330-019-06018-w
Cosman F, Krege JH, Looker AC et al (2017) Spine fracture prevalence in a nationally representative sample of US women and men aged ≥40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013–2014. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 28:1857–1866. https://doi.org/10.1007/s00198-017-3948-9
Oudshoorn C, Hartholt K, Zillikens C et al (2012) Emergency department visits due to vertebral fractures in the Netherlands, 1986–2008: steep increase in the oldest old, strong association with falls. Inj Int J Care Inj 43:458–461. https://doi.org/10.1016/j.injury.2011.09.014
Wang H, Li C, Xiang Q et al (2012) Epidemiology of spinal fractures among the elderly in Chongqing, China. Injury 43:2109–2116. https://doi.org/10.1016/j.injury.2012.04.008
Hu Z, Man GCW, Kwok AKL et al (2018) Global sagittal alignment in elderly patients with osteoporosis and its relationship with severity of vertebral fracture and quality of life. Arch Osteoporos 13:95. https://doi.org/10.1007/s11657-018-0512-y
Fechtenbaum J, Etcheto A, Kolta S et al (2016) Sagittal balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 27:559–567. https://doi.org/10.1007/s00198-015-3283-y
Bassani T, Galbusera F, Luca A et al (2019) Physiological variations in the sagittal spine alignment in an asymptomatic elderly population. Spine J 19:1840–1849. https://doi.org/10.1016/j.spinee.2019.07.016
Amabile C, Le Huec J-C, Skalli W (2018) Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J 27:458–466. https://doi.org/10.1007/s00586-016-4830-8
Crawford RP, Cann CE, Keaveny TM (2003) Finite element models predict in vitro vertebral body compressive strength better than quantitative computed tomography. Bone 33:744–750. https://doi.org/10.1016/S8756-3282(03)00210-2
Li D, Xiao Z, Wang G, Zhao G (2014) Novel, fast and efficient image-based 3D modeling method and its application in fracture risk evaluation. Exp Ther Med 7:1583–1590. https://doi.org/10.3892/etm.2014.1645
Choisne J, Valiadis J-M, Travert C et al (2018) Vertebral strength prediction from bi-planar dual energy x-ray absorptiometry under anterior compressive force using a finite element model: An in vitro study. J Mech Behav Biomed Mater 87:190–196. https://doi.org/10.1016/j.jmbbm.2018.07.026
Imai K (2011) Vertebral fracture risk and alendronate effects on osteoporosis assessed by a computed tomography-based nonlinear finite element method. J Bone Miner Metab 29:645–651. https://doi.org/10.1007/s00774-011-0281-9
Allaire BT, Lu D, Johannesdottir F et al (2019) Prediction of incident vertebral fracture using CT-based finite element analysis. Osteoporos Int 30:323–331. https://doi.org/10.1007/s00198-018-4716-1
Briggs AM, van Dieën JH, Wrigley TV et al (2007) Thoracic kyphosis affects spinal loads and trunk muscle force. Phys Ther 87:595–607. https://doi.org/10.2522/ptj.20060119
Bruno AG, Anderson DE, D’Agostino J, Bouxsein ML (2012) The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J Bone Miner Res Off J Am Soc Bone Miner Res 27:2144–2151. https://doi.org/10.1002/jbmr.1658
Buckley JM, Kuo CC, Cheng LC et al (2009) Relative strength of thoracic vertebrae in axial compression versus flexion. Spine J Off J North Am Spine Soc 9:478–485. https://doi.org/10.1016/j.spinee.2009.02.010
Travert C, Jolivet E, Sapin-de Brosses E et al (2011) Sensitivity of patient-specific vertebral finite element model from low dose imaging to material properties and loading conditions. Med Biol Eng Comput 49:1355–1361. https://doi.org/10.1007/s11517-011-0825-0
Cosson P, DUVAL-BEAUPERE G, (1993) Détermination personnalisée in vivo chez l’homme des efforts exercés sur les étages vertébraux thoraciques et lombaires en position debout et assise. Déterm Personnal Vivo Chez Homme Efforts Exerc Sur Étages Vertébraux Thorac Lombaires En Position Debout Assise 5:5–12
Mitton D, Deschênes S, Laporte S et al (2006) 3D reconstruction of the pelvis from bi-planar radiography. Comput Methods Biomech Biomed Engin 9:1–5. https://doi.org/10.1080/10255840500521786
Humbert L, De Guise JA, Aubert B et al (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31:681–687. https://doi.org/10.1016/j.medengphy.2009.01.003
Nérot A, Choisne J, Amabile C et al (2015) A 3D reconstruction method of the body envelope from biplanar X-rays: evaluation of its accuracy and reliability. J Biomech 48:4322–4326. https://doi.org/10.1016/j.jbiomech.2015.10.044
Thenard T, Vergari C, Hernandez T et al (2019) Analysis of center of mass and gravity-induced vertebral axial torque on the scoliotic spine by barycentremetry. Spine Deform 7:525–532. https://doi.org/10.1016/j.jspd.2018.11.007
Dubousset J, Charpak G, Skalli W et al (2010) Eos: a new imaging system with low dose radiation in standing position for spine and bone & joint disorders. J Musculoskelet Res 13:1–12. https://doi.org/10.1142/S0218957710002430
Faro FD, Marks MC, Pawelek J, Newton PO (2004) Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine 29:2284–2289. https://doi.org/10.1097/01.brs.0000142224.46796.a7
Gajny L, Ebrahimi S, Vergari C et al (2019) Quasi-automatic 3D reconstruction of the full spine from low-dose biplanar X-rays based on statistical inferences and image analysis. Eur Spine J 28:658–664. https://doi.org/10.1007/s00586-018-5807-6
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103. https://doi.org/10.1007/s005860050038
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine 19:1611–1618
Amabile C, Pillet H, Lafage V et al (2016) A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults. Eur Spine J 25:3666–3674. https://doi.org/10.1007/s00586-016-4552-y
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34:E599. https://doi.org/10.1097/BRS.0b013e3181aad219
Amabile C, Choisne J, Nérot A et al (2016) Determination of a new uniform thorax density representative of the living population from 3D external body shape modeling. J Biomech 49:1162–1169. https://doi.org/10.1016/j.jbiomech.2016.03.006
Grados F, Marcelli C, Dargent-Molina P et al (2004) Prevalence of vertebral fractures in French women older than 75 years from the EPIDOS study. Bone 34:362–367. https://doi.org/10.1016/j.bone.2003.11.008
Melton LJ, Lane AW, Cooper C et al (1993) Prevalence and incidence of vertebral deformities. Osteoporos Int 3:113–119. https://doi.org/10.1007/BF01623271
Pennec GL, Campana S, Jolivet E et al (2014) CT-based semi-automatic quantification of vertebral fracture restoration. Comput Methods Biomech Biomed Engin 17:1086–1095. https://doi.org/10.1080/10255842.2012.736968
Bouxsein ML, Melton LJ, Riggs BL et al (2006) Age- and sex-specific differences in the factor of risk for vertebral fracture: a population-based study using QCT. J Bone Miner Res 21:1475–1482. https://doi.org/10.1359/jbmr.060606
Kolta S, Kerkeni S, Travert C et al (2012) Variations in vertebral body dimensions in women measured by 3D-XA: a longitudinal in vivo study. Bone 50:777–783. https://doi.org/10.1016/j.bone.2011.12.005
Riggs BL, Melton Iii LJ, Robb RA et al (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res Off J Am Soc Bone Miner Res 19:1945–1954. https://doi.org/10.1359/JBMR.040916
Acknowledgements
The authors thank the ParisTech BiomecAM chair program on subject-specific musculoskeletal modelling and in particular Société Générale and COVEA.
Funding
This work was supported by the ParisTech BiomecAM chair program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The protocol was approved by the Comité de Protection des Personnes Ile-de-France VI Paris (Ethics Committee).
Consent to participate
All subjects provided their written informed consent.
Consent for publication
All subjects provided their written informed consent.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Heidsieck, C., Gajny, L., Travert, C. et al. Effect of postural alignment alteration with age on vertebral strength. Osteoporos Int 33, 443–451 (2022). https://doi.org/10.1007/s00198-021-06093-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06093-0