Abstract
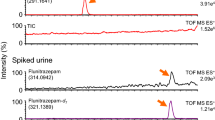
We demonstrate the suitability of a fast, green, easy-to-perform, and modified sample extraction procedure, i.e., dispersive liquid–liquid microextraction (DLLME) for the determination of efavirenz (EFV) in human plasma. Data acquisition was done by gas chromatography–mass spectrometry (GC–MS) in the selected ion monitoring (SIM) mode. The simplicity of the method lies in, among others, the avoidance of the use of large organic solvent volumes as mobile phases and non-volatile buffers that tend to block the plumbing in high-performance liquid chromatography (HPLC). Chromatographic and mass spectral parameters were optimized using bovine whole blood for matrix matching due to insufficient human plasma. Method validation was accomplished using the United States Food and Drug Administration (USFDA) 2018 guidelines. The calibration curve was linear with a dynamic range of 0.10–2.0 μg/mL and an R2 value of 0.9998. The within-run accuracy and precision were both less than 20% at the lower limit of quantification (LLOQ) spike level. The LLOQ was 0.027 μg/mL which compared well with some values but was also orders of magnitude better than others reported in the literature. The percent recovery was 91.5% at the LLOQ spike level. The DLLME technique was applied in human plasma samples from patients who were on treatment with EFV. The human plasma samples gave concentrations of EFV ranging between 0.14–1.00 μg/mL with three samples out of seven showing concentrations that fell within or close to the recommended therapeutic range.
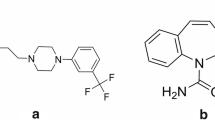
Graphical abstract







Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Neogi U, Häggblom A, Singh AK, Rogers LC, Rao SD, Amogne W, Schülter E, Zazzi M, Arnold E, Sarafianos SG, Sönnerborg A. Factors influencing the efficacy of rilpivirine in HIV-1 subtype C in low- and middle-income countries. J Antimicrob Chemother. 2016;71(2):367–71. https://doi.org/10.1093/jac/dkv359.
Hemelaar J, Gouws E, Ghys PD, et al. Global trends in molecular epidemiology of HIV-1 during 2000–2007. AIDS. 2011;25:679–89. https://doi.org/10.1097/QAD.0b013e328342ff93.
The NAMSAL ANRS 12313 Study Group. Dolutegravir-based or low-doseefavirenz–based regimen for the treatment of HIV-1. N Engl J Med. 2019;381:816–26. https://doi.org/10.1056/NEJMoa1904340.
World Health Organization. (WHO) (2019) Update of recommendations on first- and second-line antiretroviral regimens. Geneva, Switzerland: World Health Organization; (WHO/CDS/HIV/19.15). Licence: CC BY-NC-SA 3.0 IGO. Last Accessed 29th September 2020.
Hartman TL, Buckheit RW. The continuing evolution of HIV-1 therapy: identification and development of novel antiretroviral agents targeting viral and cellular targets. Mol Biol Int J. 2012;401965. https://doi.org/10.1155/2012/401965.
Hoen E, Berger J, Calmy A, Moon S. Driving a decade of change: HIV/AIDS, patents and access to medicines for all. J Intern AIDS Soc. 2011;14:15–27. https://doi.org/10.1186/1758-2652-14-15.
Arendt G, De-Nocker D, Von-Giesen HJ, Nolting T. Neuropsychiatric side effects of efavirenz therapy. Expert Opin Drug Saf. 2007;6:147–54. https://doi.org/10.1517/14740338.6.2.147.
Evans-Jones JG, Cottle LE, Back DJ, Gibbons S, Beeching NJ, Carey PB, Khoo SH. Recognition of risk for clinically significant drug interactions among HIV-infected patients receiving antiretroviral therapy. J Clin Infect Dis. 2010;50:1419–21. https://doi.org/10.1086/652149.
Gallant JE, DeJesus E, Arribas JR, Pozniak AL, Gazzard B, Campo RE, Lu B, McColl D, Chuck S, Enejosa J, Toole JJ, Cheng AK. Tenofovir DF, emtricitabine, and efavirenz vs. zidovudine, lamivudine and efavirenz for HIV. New Engl J Med. 2006;354:251–60. https://doi.org/10.1056/NEJMoa051871.
Russo G, Paganotti GM, Soeria-Atmadja S, Haverkamp M, Ramogola-Masire D, Vullo V, Gustafsson LL. Pharmacogenetics of non-nucleoside reverse transcriptase inhibitors (NNRTIs) in resource-limited settings: influence on antiretroviral therapy response and concomitant anti-tubercular, antimalarial and contraceptive treatments. Infect Genet Evol. 2016;37:192–207. https://doi.org/10.1016/j.meegid.2015.11.014.
Apostolova N, Funes HA, Blas-Garcia A, Galindo MJ, Alvarez A, Esplugues JV. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693–708. https://doi.org/10.1093/jac/dkv183.
Donnerer J, Kronawetter M, Kapper A, Haas I, Kessler HH. Therapeutic drug monitoring of the HIV / AIDS drugs abacavir, zidovudine, efavirenz, nevirapine, indinavir, lopinavir, and nelfinavir. Aust J Pharm. 2003;69:197–204. https://doi.org/10.1159/000073664.
Langmann P, Zilly M, Weissbrich B, Desch S, Väth T, Klinker H. Therapeutic drug monitoring of Indinavir in HIV-infected patients undergoing HAART. J Infect Dis. 2002;30:13–6. https://doi.org/10.1007/s15010-001-1111-0.
Rezk NL, Tidwell RR, Kashuba ADM. High-performance liquid chromatography assay for the quantification of HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors in human plasma. J Chromatogr B. 2004;805:241–7. https://doi.org/10.1016/j.jchromb.2004.03.002.
Sarasa-Nacenta M, Lopez-pua Y, Lopez-Cortes LF, Mallolas J, Gatell JM, Carne X. Determination of efavirenz in human plasma by high-performance liquid chromatography with ultraviolet detection. J Chromatogr B. 2001;763:53–9. https://doi.org/10.1016/s0378-4347(01)00357-7.
Dailly E, Raffi F, Jolliet P. Determination of atazanavir and other antiretroviral drugs (indinavir, amprenavir, nelfinavir and its active metabolite M8, saquinavir, ritonavir, lopinavir, nevirapine and efavirenz) plasma levels by high performance liquid chromatography with UV detection. J Chromatogr B. 2004;813:353–8. https://doi.org/10.1016/j.jchromb.2004.10.005.
Ramachandran G, Kumar AKH, Swaminathan S, Venkatesan P, Kumaraswami V, Greenblatt DJ. Simple and rapid liquid chromatography method for determination of efavirenz in plasma. J Chromatogr. 2006;835(2006):131–5. https://doi.org/10.1016/j.jchromb.2006.03.014.
Fox D, Connor RO, Mallon P, Mcmahon G. Simultaneous determination of efavirenz, rifampicin and its metabolite desacetyl rifampicin levels in human plasma. J Pharmaceut Biomed Anal. 2011;56:785–91. https://doi.org/10.1016/j.jpba.2011.07.041.
Hoffman JT, Rossi SS, Espina-Quinto R, Letendre S, Capparelli EV. Determination of efavirenz in human dried blood spots by reversed-phase high-performance liquid chromatography with UV detection. J Ther Drug Monit. 2013;35:203–8. https://doi.org/10.1097/FTD.0b013e31827fb72b.
Ren C, Fan-Havard P, Schlabritz-Loutsevitch N, Ling Y, Chan KK, Liu Z. A sensitive and specific liquid chromatography/tandem mass spectrometry method for quantification of nevirapine and its five metabolites and their pharmacokinetics in baboons. J Biomed Chromatogr. 2009;24:717–26. https://doi.org/10.1002/bmc.1353.
Theron A, Cromarty D, Rheeders M, Viljoen M. Determination of salivary efavirenz by liquid chromatography coupled with tandem mass spectrometry. J Chromatogr B. 2010;878:2886–90. https://doi.org/10.1016/j.jchromb.2010.08.051.
Zhang L, Sun J, Chen J, Jia XF, Shen F, Lu HZ. An LC–MS/MS method for simultaneous quantification of seven anti-HIV medicines in plasma of HIV-infected patients. Pharm Anal Acta. 2010;1:102. https://doi.org/10.4172/2153-2435.1000102.
Soldin SJ, Soukhov N, Janici N, Jonklaas J, Soldin OP. The measurement of free thyroxine by isotope dilution tandem mass spectrometry. Clin Chimica Acta. 2005;358:113–8. https://doi.org/10.1016/j.cccn.2005.02.010.
Sichilongo K, Mwando E, Sepako E, Massele A. Comparison of efficiencies of selected sample extraction techniques for the analysis of selected antiretroviral drugs in human plasma using LC-MS. J Pharmacol Toxicol Methods. 2018;89:1–8. https://doi.org/10.1016/j.vascn.2017.10.001.
Srivastava P, Moorthy GS, Gross R, Barrett JS. A sensitive and selective liquid chromatography/tandem mass spectrometry method for quantitative analysis of efavirenz in human plasma. PLoS One. 2013;8:1–9. https://doi.org/10.1371/journal.pone.0063305.
Rouzes A, Karine B, Xuere F, Djabarouti S, Pellegrin I, Pellegrin JL, Coupet AC, Augagneur, Budzinski H, Saux MC, Breilh D. Simultaneous determination of the antiretroviral agents: amprenavir , lopinavir, ritonavir, saquinavir and efavirenz in human peripheral blood mononuclear cells by high-performance liquid chromatography – mass spectrometry. J Chromatogr B. 2004;813:209–16. https://doi.org/10.1016/j.jchromb.2004.09.041.
Huang Y, Gandhi M, Greenblatt RM, Gee W, Lin EST, Messenkoff N. Sensitive analysis of anti-HIV drugs, efavirenz, lopinavir and ritonavir, in human hair by liquid chromatography coupled with tandem mass spectrometry. Rapid Commun Mass Spectrom. 2008;22:3401–9. https://doi.org/10.1002/rcm.3750.
Lemmer P, Schneider S, Schuman M, Omes C, Arendt V, Tayari JC, Fundira L, Wennig R. Determination of nevirapine and efavirenz in plasma using GC/MS in selected ion monitoring mode. J Ther Drug Monit. 2002;27:521–5. https://doi.org/10.1097/01.ftd.0000164613.91555.2e.
González O, Alonso RM. Validation of bioanalytical chromatographic methods for the quantification of drugs in biological fluids. Handbook of Analytical Separations. 2020;7:115–34.
Ridgway K (2019). https://www.anatune.co.uk/wp-content/uploads/2019/04/AS224-Automated-solvent-extraction-LLME-and-DLLME-of-Flavours-from-a-selection-of-fruit-beverages.pdf last accessed 3rd august 2020.
USFDA (2018). Bioanalytical method validation guidance for industry, https://www.fda.gov/media/70858/download last accessed 7th august 2020.
Azadeh M, Gorovits B, Kamerud J, MacMannis S, Safavi A, Sailstad J, Sondag P. Calibration curves in quantitative ligand binding assays: recommendations and best practices for preparation, design, and editing of calibration curves. AAPS J. 2018;20:22. https://doi.org/10.1208/s12248-017-0159-430.
Cheng CL, Chou CH, Yoa-Pu Huc O. Determination of lamotrigine in small volumes of plasma by high-performance liquid chromatography. J Chromatogr B. 2005;817:199–206. https://doi.org/10.1016/j.jchromb.2004.12.004.
Cheng CL, Chou CH, Yoa-Pu Huc O. Determination of delavirdine in very small volumes of plasma by high-performance liquid chromatography with fluorescence detection. J Chromatogr B. 2002;769:297–303. https://doi.org/10.1016/S1570-0232(02)00015-6.
Heydari R, Rashidipour M, Naleini N. Determination of efavirenz in plasma by dispersive liquid-liquid micro-extraction coupled to high-performance liquid chromatography. Current Anal Chem. 2014;10:280–7. https://doi.org/10.2174/15734110113099990003.
Polson C, Sarkar P, Incledon B, Raguvaran V, Grant R. Optimization of protein precipitation based upon effectiveness of protein removal and ionization effect in liquid chromatography– tandem mass spectrometry. J Chromatogr B. 2003;785:263–75. https://doi.org/10.1016/S1570-0232(02)00914-5.
Toribio-Delgado AF, Robles-Gil MC, Maynar-Mariño M, Olcina-Camacho G, Maynar-Mariño JI. Is deproteinization necessary in the determination of human plasmatic steroids by GC/IT-MS/MS analysis? J Applied Bioanal. 2015;1:10–8. https://doi.org/10.17145/jab.15.003(ISSN 2405-710X).
Wisconsin Department of Natural Resources Laboratory Certification Program (1996) Analytical detection limit guidance & laboratory guide for determining method detection limits. https://dnr.wi.gov/regulations/labcert/documents/guidance/-LODguide.pdf Last Accessed 8th March 2021.
Matuszewski BK, Constanzer ML, Chavez-Eng CM. Strategies for the assessment of matrix effect in quantitative bioanalytical methods based on HPLC - MS / MS. Intern J Anal Chem. 2003;75:3019–30. https://doi.org/10.1021/ac020361s.
Bednasz CJ, Venuto CS, Ma Q, Daar ES, Sax PE, Fischl MA, Collier AC, Smith KY, Tierney C, Yang Y, Wilding GE, Morse GD. Efavirenz therapeutic range in HIV-1 treatment-naive participants. Ther Drug Monit. 2017;39:596–603. https://doi.org/10.1097/FTD.0000000000000443.
Kankaanpää A, Turtiainen S, Meririnne E, Ariniemi K, Ristola M, Kuoppasalmi K. Determination of the non-nucleoside reverse transcriptase inhibitor efavirenz in human plasma by gas chromatography mass spectrometry. Ther Drug Mont. 2007;29:513–4.
Acknowledgements
The authors thank the University of Botswana and the Ministry of Health and Wellness for granting ethical approval.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Ethical approval to conduct this study was obtained from the University of Botswana Office of Research and Development (Reference Number RES/IRB/CHMS/014) and Human Research Development Division (HRDD) (Reference Number HPDME: 13/18/1).
Consent to participate
Informed consent was obtained from all participants before enrolment in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Masenga, W., Paganotti, G.M., Seatla, K. et al. A fast-screening dispersive liquid–liquid microextraction–gas chromatography–mass spectrometry method applied to the determination of efavirenz in human plasma samples. Anal Bioanal Chem 413, 6401–6412 (2021). https://doi.org/10.1007/s00216-021-03604-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-021-03604-0