Abstract
Introduction
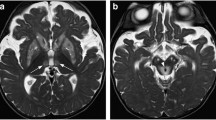
In children, many inherited or acquired neurological disorders may cause bilateral symmetrical signal intensity alterations in the basal ganglia and thalami.
Methods
A literature review was aimed at assisting neuroradiologists, neurologists, infectious diseases specialists, and pediatricians to provide further understanding into the clinical and neuroimaging features in pediatric patients presenting with bilateral symmetrical basal ganglia and thalamic lesions on magnetic resonance imaging (MRI).
Results
We discuss hypoxic-ischemic, toxic, infectious, immune-mediated, mitochondrial, metabolic, and neurodegenerative disorders affecting the basal ganglia and thalami.
Conclusion
Recognition and correct evaluation of basal ganglia abnormalities, together with a proper neurological examination and laboratory findings, may enable the identification of each of these clinical entities and lead to earlier diagnosis.
















Similar content being viewed by others
References
Williams K, Thomson D, Seto I, StaR Child Health Group et al (2012) Standard 6: age groups for pediatric trials. Pediatrics 129(Suppl 3):S153–S160. doi:10.1542/peds.2012-0055I
Tian N, Shaw EC, Zack M et al (2015) Cause-specific mortality among children and young adults with epilepsy: results from the U.S. National Child Death Review Case Reporting System. Epilepsy Behav 45:31–34. doi:10.1016/j.yebeh.2015.02.006
Wallis BA, Watt K, Franklin RC et al (2015) Drowning mortality and morbidity rates in children and adolescents 0-19yrs: a population-based study in Queensland, Australia. PLoS One 10, e0117948. doi:10.1371/journal.pone.0117948
Bhalala US, Koehler RC, Kannan S (2014) Neuroinflammation and neuroimmune dysregulation after acute hypoxic-ischemic injury of developing brain. Front Pediatr 2:144. doi:10.3389/fped.2014.00144
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22:391–397
Ginsberg MD, Hedley-Whyte E, Richardson EP Jr (1976) Hypoxic-ischemic leukoencephalopathy in man. Arch Neurol 33:5–14. doi:10.1001/archneur.1976.00500010007002
Panigrahy A, Blüm S (2007) Advances in magnetic resonance neuroimaging techniques in the evaluation of neonatal encephalopathy. Top Magn Reson Imaging 18:3–29. doi:10.1097/RMR.0b013e318093e6c7
Fink EL, Panigrahy A, Clark RSB et al (2013) Regional brain injury on conventional and diffusion weighted MRI is associated with outcome after pediatric cardiac arrest. Neurocrit Care 19:31–40. doi:10.1007/s12028-012-9706-0
Aoe H, Takeda Y, Kawahara H et al (2006) Clinical significance of T1-weighted MR images following transient cerebral ischemia. J Neurol Sci 241:19–24. doi:10.1016/j.jns.2005.10.013
Cakirer S, Karaarslan E, Arslan A (2003) Spontaneously T1-hyperintense lesions of the brain on MRI: a pictorial review. Curr Probl Diagn Radiol 32:194–217. doi:10.1016/S0363-0188(03)00026-4
Bekiesinska-Figatowska M, Mierzewska H, Jurkiewicz E (2013) Basal ganglia lesions in children and adults. Eur J Radiol 82:837–849. doi:10.1016/j.ejrad.2012.12.006
Malamud N (1950) Status marmoratus; a form of cerebral palsy following either birth injury or inflammation of the central nervous system. J Pediatr 37:610–619
Nucci-da-Silva MP, Amaro E (2009) A systematic review of Magnetic Resonance Imaging and Spectroscopy in brain injury after drowning. Brain Inj 23:707–714. doi:10.1080/02699050903123351
Zanin A, Masiero S, Severino MS et al (2010) A delayed methadone encephalopathy: clinical and neuroradiological findings. J Child Neurol 25:748–751. doi:10.1177/0883073809343318
Wheless JW, Carmant L, Bebin M et al (2009) Magnetic resonance imaging abnormalities associated with vigabatrin in patients with epilepsy. Epilepsia 50:195–205. doi:10.1111/j.1528-1167.2008.01896.x
Pearl PL, Vezina LG, Saneto RP et al (2009) Cerebral MRI abnormalities associated with vigabatrin therapy. Epilepsia 50:184–194. doi:10.1111/j.1528-1167.2008.01728.x
Bazmamoun H, Fayyazi A, Khajeh A et al (2014) A study of methadone-poisoned children referred to Hamadan’s Besat Hospital/Iran. Iran J Child Neurol 8:34–37
Preece NE, Houseman J, King MD et al (2004) Development of vigabatrin-induced lesions in the rat brain studied by magnetic resonance imaging, histology, and immunocytochemistry. Synapse 53:36–43. doi:10.1002/syn.20038
Dracopoulos A, Widjaja E, Raybaud C et al (2010) Vigabatrin-associated reversible MRI signal changes in patients with infantile spasms. Epilepsia 51:1297–1304. doi:10.1111/j.1528-1167.2010.02564.x
Beppu T (2014) The role of MR imaging in assessment of brain damage from carbon monoxide poisoning: a review of the literature. Am J Neuroradiol 35:625–631. doi:10.3174/ajnr.A3489
Velioglu M, Gümüş T, Hüsmen G (2013) Cerebellar lesions in the acute setting of carbon monoxide poisoning. Emerg Radiol 20:255–257. doi:10.1007/s10140-013-1108-x
Ono J, Harada K, Kodaka R et al (1995) Manganese deposition in the brain during long-term total parenteral nutrition. JPEN J Parenter Enteral Nutr 19:310–312
Fell JM, Reynolds AP, Meadows N et al (1996) Manganese toxicity in children receiving long-term parenteral nutrition. Lancet 347:1218–1221
Quaghebeur G, Taylor WJ, Kingsley DP et al (1996) MRI in children receiving total parenteral nutrition. Neuroradiology 38:680–683
Häusler M, Ramaekers VT, Doenges M et al (2002) Neurological complications of acute and persistent Epstein-Barr virus infection in paediatric patients. J Med Virol 68:253–263. doi:10.1002/jmv.10201
Phowthongkum P, Phantumchinda K, Jutivorakool K, Suankratay C (2007) Basal ganglia and brainstem encephalitis, optic neuritis, and radiculomyelitis in Epstein-Barr virus infection. J Infect 54:e141–e144. doi:10.1016/j.jinf.2006.09.007
Baskin HJ, Hedlund G (2007) Neuroimaging of herpesvirus infections in children. Pediatr Radiol 37:949–963. doi:10.1007/s00247-007-0506-1
Abul-Kasim K, Palm L, Maly P, Sundgren PC (2009) The neuroanatomic localization of Epstein-Barr virus encephalitis may be a predictive factor for its clinical outcome: a case report and review of 100 cases in 28 reports. J Child Neurol 24:720–726
Lindsey NP, Hayes EB, Staples JE, Fischer M (2009) West Nile virus disease in children, United States, 1999-2007. Pediatrics 123:e1084–e1089. doi:10.1542/peds.2008-3278
Civen R, Villacorte F, Robles DT et al (2006) West Nile virus infection in the pediatric population. Pediatr Infect Dis J 25:75–78
Weber IB, Lindsey NP, Bunko-Patterson AM et al (2012) Completeness of West Nile virus testing in patients with meningitis and encephalitis during an outbreak in Arizona, USA. Epidemiol Infect 140:1632–1636. doi:10.1017/S0950268811002494
Ali M, Safriel Y, Sohi J et al (2005) West Nile virus infection: MR imaging findings in the nervous system. AJNR Am J Neuroradiol 26:289–297
Whitley RJ, MacDonald N, Asher DM (2000) American Academy of Pediatrics. Technical report: transmissible spongiform encephalopathies: a review for pediatricians. Committee on Infectious Diseases. Pediatrics 106:1160–1165
Zeng H, Quinet S, Huang W et al (2013) Clinical and MRI features of neurological complications after influenza A (H1N1) infection in critically ill children. Pediatr Radiol 43:1182–1189. doi:10.1007/s00247-013-2682-5
Kim JH, Choi BS, Jung C et al (2011) Diffusion-weighted imaging and magnetic resonance spectroscopy of sporadic Creutzfeldt-Jakob disease: correlation with clinical course. Neuroradiology 53:939–945. doi:10.1007/s00234-010-0820-4
Tomiyasu M, Aida N, Watanabe Y et al (2012) Monitoring the brain metabolites of children with acute encephalopathy caused by the H1N1 virus responsible for the 2009 influenza pandemic: a quantitative in vivo 1H MR spectroscopy study. Magn Reson Imaging 30:1527–1533. doi:10.1016/j.mri.2012.05.007
Mizuguchi M, Abe J, Mikkaichi K et al (1995) Acute necrotising encephalopathy of childhood: a new syndrome presenting with multifocal, symmetric brain lesions. J Neurol Neurosurg Psychiatry 58:555–561
Wong AM, Simon EM, Zimmerman RA et al (2006) Acute necrotizing encephalopathy of childhood: correlation of MR findings and clinical outcome. Am J Neuroradiol 27:1919–1923
Dale RC (2005) Post-streptococcal autoimmune disorders of the central nervous system. Dev Med Child Neurol 47:785–791. doi:10.1111/j.1469-8749.2005.tb01079.x
Rubio-Agustí I, Dalmau J, Sevilla T et al (2011) Isolated hemidystonia associated with NMDA receptor antibodies. Mov Disord 26:351–352. doi:10.1002/mds.23315
Kim S-H, Huh S-Y, Hyun J-W et al (2014) A longitudinal brain magnetic resonance imaging study of neuromyelitis optica spectrum disorder. PLoS ONE 9, e108320. doi:10.1371/journal.pone.0108320
Zuccoli G, Panigrahy A, Sreedher G et al (2014) Vasogenic edema characterizes pediatric acute disseminated encephalomyelitis. Neuroradiology 56:679–684. doi:10.1007/s00234-014-1379-2
Robertson WC, Smith CD (2002) Sydenham’s chorea in the age of MRI: a case report and review. Pediatr Neurol 27:65–67
Swedo SE, Seidlitz J, Kovacevic M et al (2015) Clinical presentation of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections in research and community settings. J Child Adolesc Psychopharmacol 25:26–30. doi:10.1089/cap.2014.0073
Giedd JN, Rapoport JL, Garvey MA et al (2000) MRI assessment of children with obsessive-compulsive disorder or tics associated with streptococcal infection. Am J Psychiatry 157:281–283
Elia J, Dell ML, Friedman DF et al (2005) PANDAS with catatonia: a case report. Therapeutic response to lorazepam and plasmapheresis. J Am Acad Child Adolesc Psychiatry 44:1145–1150. doi:10.1097/01.chi.0000179056.54419.5e
Kumar A, Williams MT, Chugani HT (2015) Evaluation of basal ganglia and thalamic inflammation in children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection and Tourette syndrome: a positron emission tomographic (PET) study using 11C-[R]-PK11195. J Child Neurol 30:749–756. doi:10.1177/0883073814543303
Ben Azoun M, Tatencloux S, Deiva K, Blanc P (2014) Two pediatric cases of anti-NMDA receptor antibody encephalitis. Arch Pédiatr 21:1216–1219. doi:10.1016/j.arcped.2014.08.020
Tzoulis C, Vedeler C, Haugen M et al (2013) Progressive striatal necrosis associated with anti-NMDA receptor antibodies. BMC Neurol 13:55. doi:10.1186/1471-2377-13-55
Lennon VA, Kryzer TJ, Pittock SJ et al (2005) IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med 202:473–477. doi:10.1084/jem.20050304
Wingerchuk DM, Lennon VA, Pittock SJ et al (2006) Revised diagnostic criteria for neuromyelitis optica. Neurology 66:1485–1489
Tenembaum S, Chitnis T, Ness J, Hahn JS, International Pediatric MS Study Group (2007) Acute disseminated encephalomyelitis. Neurology 68:S23–S36. doi:10.1212/01.wnl.0000259404.51352.7f
Krupp LB, Banwell B, Tenembaum S et al (2007) Consensus definitions proposed for pediatric multiple sclerosis and related disorders. Neurology 68:S7–S12
Schor NF (2000) Neurology of systemic autoimmune disorders: a pediatric perspective. Semin Pediatr Neurol 7:108–117
Zuccoli G, Crowley H, Cecil KM (2013) Inherited metabolic and neurodegenerative disorders. In: Caffeys Pediatr. Diagn. Imaging, 12th edn. Elsevier Health Sciences, Philadelphia, pp 330–357
Autti T, Joensuu R, Aberg L (2007) Decreased T2 signal in the thalami may be a sign of lysosomal storage disease. Neuroradiology 49:571–578. doi:10.1007/s00234-007-0220-6
Provenzale JM, Barboriak DP, Sims K (1995) Neuroradiologic findings in fucosidosis, a rare lysosomal storage disease. Am J Neuroradiol 16:809–813
Arii J, Tanabe Y (2000) Leigh syndrome: serial MR imaging and clinical follow-up. AJNR Am J Neuroradiol 21:1502–1509
Warmuth-Metz M, Hofmann E, Büsse M, Solymosi L (1999) Uncommon morphologic characteristics in Leigh’s disease. AJNR Am J Neuroradiol 20:1158–1160
Sener RN (2004) Diffusion magnetic resonance imaging patterns in metabolic and toxic brain disorders. Acta Radiol 45:561–570
Rossi A, Biancheri R, Bruno C et al (2003) Leigh syndrome with COX deficiency and SURF1 gene mutations: MR imaging findings. Am J Neuroradiol 24:1188–1191
Krägeloh-Mann I, Grodd W, Schöning M et al (1993) Proton spectroscopy in five patients with Leigh’s disease and mitochondrial enzyme deficiency. Dev Med Child Neurol 35:769–776
Brismar J, Ozand PT (1995) CT and MR of the brain in glutaric acidemia type I: a review of 59 published cases and a report of 5 new patients. AJNR Am J Neuroradiol 16:675–683
Desai NK, Runge VM, Crisp DE et al (2003) Magnetic resonance imaging of the brain in glutaric acidemia type I: a review of the literature and a report of four new cases with attention to the basal ganglia and imaging technique. Investig Radiol 38:489–496. doi:10.1097/01.rli.0000080405.62988.f6
Manoli I, Venditti CP (1993) Methylmalonic acidemia. GeneReviews(®)
Baumgarter ER, Viardot C (1995) Long-term follow-up of 77 patients with isolated methylmalonic acidaemia. J Inherit Metab Dis 18:138–142
Sobrido MJ, Coppola G, Oliveira J, et al. (1993) Primary familial brain calcification. GeneReviews(®)
Livingston JH, Stivaros S, van der Knaap MS, Crow YJ (2013) Recognizable phenotypes associated with intracranial calcification. Dev Med Child Neurol 55:46–57. doi:10.1111/j.1469-8749.2012.04437.x
Illum F, Dupont E (1985) Prevalences of CT-detected calcification in the basal ganglia in idiopathic hypoparathyroidism and pseudohypoparathyroidism. Neuroradiology 27:32–37
Brunetti-Pierri N, Scaglia F (2008) GM1 gangliosidosis: review of clinical, molecular, and therapeutic aspects. Mol Genet Metab 94:391–396. doi:10.1016/j.ymgme.2008.04.012
Regier DS, Tifft CJ (1993) GLB1-related disorders. GeneReviews(®)
Erol I, Alehan F, Pourbagher MA et al (2006) Neuroimaging findings in infantile GM1 gangliosidosis. Eur J Paediatr Neurol 10:245–248. doi:10.1016/j.ejpn.2006.08.005
Kaback MM, Desnick RJ (1993) Hexosaminidase A deficiency. GeneReviews(®)
Kroll RA, Pagel MA, Roman-Goldstein S et al (1995) White matter changes associated with feline GM2 gangliosidosis (Sandhoff disease): correlation of MR findings with pathologic and ultrastructural abnormalities. AJNR Am J Neuroradiol 16:1219–1226
Yüksel A, Yalçinkaya C, Işlak C et al (1999) Neuroimaging findings of four patients with Sandhoff disease. Pediatr Neurol 21:562–565
Chen CY, Zimmerman RA, Lee CC et al (1998) Neuroimaging findings in late infantile GM1 gangliosidosis. AJNR Am J Neuroradiol 19:1628–1630
Wilken B, Dechent P, Hanefeld F, Frahm J (2008) Proton MRS of a child with Sandhoff disease reveals elevated brain hexosamine. Eur J Paediatr Neurol 12:56–60. doi:10.1016/j.ejpn.2007.05.008
Jan W, Zimmerman RA, Wang ZJ et al (2003) MR diffusion imaging and MR spectroscopy of maple syrup urine disease during acute metabolic decompensation. Neuroradiology 45:393–399. doi:10.1007/s00234-003-0955-7
Ha JS, Kim T-K, Eun B-L et al (2004) Maple syrup urine disease encephalopathy: a follow-up study in the acute stage using diffusion-weighted MRI. Pediatr Radiol 34:163–166. doi:10.1007/s00247-003-1058-7
Brismar J, Aqeel A, Brismar G et al (1990) Maple syrup urine disease: findings on CT and MR scans of the brain in 10 infants. Am J Neuroradiol 11:1219–1228
Sato T, Muroya K, Hanakawa J et al (2014) Neonatal case of classic maple syrup urine disease: usefulness of (1) H-MRS in early diagnosis. Pediatr Int 56:112–115. doi:10.1111/ped.12211
Heindel W, Kugel H, Wendel U et al (1995) Proton magnetic resonance spectroscopy reflects metabolic decompensation in maple syrup urine disease. Pediatr Radiol 25:296–299
Yalcinkaya C, Benbir G, Salomons GS et al (2005) Atypical MRI findings in Canavan disease: a patient with a mild course. Neuropediatrics 36:336–339. doi:10.1055/s-2005-872878
Janson CG, McPhee SWJ, Francis J et al (2006) Natural history of Canavan disease revealed by proton magnetic resonance spectroscopy (1H-MRS) and diffusion-weighted MRI. Neuropediatrics 37:209–221. doi:10.1055/s-2006-924734
Tissières P, Chevret L, Debray D, Devictor D (2003) Fulminant Wilson’s disease in children: appraisal of a critical diagnosis. Pediatr Crit Care Med 4:338–343. doi:10.1097/01.PCC.0000074268.77622.DE
Yüce A, Koçak N, Demir H et al (2003) Evaluation of diagnostic parameters of Wilson’s disease in childhood. Indian J Gastroenterol 22:4–6
Dhawan A, Taylor RM, Cheeseman P et al (2005) Wilson’s disease in children: 37-year experience and revised King’s score for liver transplantation. Liver Transpl 11:441–448. doi:10.1002/lt.20352
Arnon R, Calderon JF, Schilsky M et al (2007) Wilson disease in children: serum aminotransferases and urinary copper on triethylene tetramine dihydrochloride (trientine) treatment. J Pediatr Gastroenterol Nutr 44:596–602. doi:10.1097/MPG.0b013e3180467715
Marcellini M, Di Ciommo V, Callea F et al (2005) Treatment of Wilson’s disease with zinc from the time of diagnosis in pediatric patients: a single-hospital, 10-year follow-up study. J Lab Clin Med 145:139–143
Kumagi T, Horiike N, Michitaka K et al (2004) Recent clinical features of Wilson’s disease with hepatic presentation. J Gastroenterol 39:1165–1169. doi:10.1007/s00535-004-1466-y
Ferenci P, Caca K, Loudianos G et al (2003) Diagnosis and phenotypic classification of Wilson disease. Liver Int 23:139–142
Sánchez-Albisua I, Garde T, Hierro L et al (1999) A high index of suspicion: the key to an early diagnosis of Wilson’s disease in childhood. J Pediatr Gastroenterol Nutr 28:186–190
Tarnacka B, Szeszkowski W, Gołębiowski M, Członkowska A (2010) Brain proton magnetic spectroscopy in long-term treatment of Wilson’s disease patients. Metab Brain Dis 25:325–329. doi:10.1007/s11011-010-9214-x
Nicolas G, Devys D, Goldenberg A et al (2011) Juvenile Huntington disease in an 18-month-old boy revealed by global developmental delay and reduced cerebellar volume. Am J Med Genet A 155:815–818. doi:10.1002/ajmg.a.33911
Reynolds NC, Prost RW, Mark LP, Joseph SA (2008) MR-spectroscopic findings in juvenile-onset Huntington’s disease. Mov Disord 23:1931–1935. doi:10.1002/mds.22245
Straussberg R, Shorer Z, Weitz R et al (2002) Familial infantile bilateral striatal necrosis Clinical features and response to biotin treatment. Neurology 59:983–989
Kornreich L, Bron-Harlev E, Hoffmann C et al (2005) Thiamine deficiency in infants: MR findings in the brain. AJNR Am J Neuroradiol 26:1668–1674
Zeng W-Q, Al-Yamani E, Acierno JS et al (2005) Biotin-responsive basal ganglia disease maps to 2q36.3 and is due to mutations in SLC19A3. Am J Hum Genet 77:16–26. doi:10.1086/431216
Haacke EM, Ayaz M, Khan A et al (2007) Establishing a baseline phase behavior in magnetic resonance imaging to determine normal vs. abnormal iron content in the brain. J Magn Reson Imaging 26:256–264. doi:10.1002/jmri.22987
Gregory A, Hayflick SJ (2011) Genetics of neurodegeneration with brain iron accumulation. Curr Neurol Neurosci Rep 11:254–261. doi:10.1007/s11910-011-0181-3
Hayflick SJ, Hartman M, Coryell J et al (2006) Brain MRI in neurodegeneration with brain iron accumulation with and without PANK2 mutations. AJNR Am J Neuroradiol 27:1230–1233
Morgan NV, Westaway SK, Morton JEV et al (2006) PLA2G6, encoding a phospholipase A2, is mutated in neurodegenerative disorders with high brain iron. Nat Genet 38:752–754. doi:10.1038/ng1826
Kurian MA, Morgan NV, MacPherson L et al (2008) Phenotypic spectrum of neurodegeneration associated with mutations in the PLA2G6 gene (PLAN). Neurology 70:1623–1629. doi:10.1212/01.wnl.0000310986.48286.8e
Illingworth MA, Meyer E, Chong WK et al (2014) PLA2G6-associated neurodegeneration (PLAN): further expansion of the clinical, radiological and mutation spectrum associated with infantile and atypical childhood-onset disease. Mol Genet Metab 112:183–189. doi:10.1016/j.ymgme.2014.03.008
Pagon RA, Adam MP, Ardinger HH, et al., others (2014) Neurodegeneration with brain iron accumulation disorders overview
Sechi G, Serra A (2007) Wernicke’s encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol 6:442–455. doi:10.1016/S1474-4422(07)70104-7
Harper CG, Giles M, Finlay-Jones R (1986) Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry 49:341–345
Vasconcelos MM, Silva KP, Vidal G et al (1999) Early diagnosis of pediatric Wernicke’s encephalopathy. Pediatr Neurol 20:289–294
Gallucci M, Bozzao A, Splendiani A et al (1990) Wernicke encephalopathy: MR findings in five patients. AJNR Am J Neuroradiol 11:887–892
Zuccoli G, Santa Cruz D, Bertolini M et al (2009) MR imaging findings in 56 patients with Wernicke encephalopathy: nonalcoholics may differ from alcoholics. AJNR Am J Neuroradiol 30:171–176. doi:10.3174/ajnr.A1280
Zuccoli G, Siddiqui N, Bailey A, Bartoletti SC (2010) Neuroimaging findings in pediatric Wernicke encephalopathy: a review. Neuroradiology 52:523–529. doi:10.1007/s00234-009-0604-x
Ozand PT, Gascon GG, Al Essa M et al (1998) Biotin-responsive basal ganglia disease: a novel entity. Brain J Neurol 121(Pt 7):1267–1279
Tabarki B, Al-Shafi S, Al-Shahwan S et al (2013) Biotin-responsive basal ganglia disease revisited: clinical, radiologic, and genetic findings. Neurology 80:261–267. doi:10.1212/WNL.0b013e31827deb4c
Zuccoli G, Pipitone N (2009) Neuroimaging findings in acute Wernicke’s encephalopathy: review of the literature. AJR Am J Roentgenol 192:501–508. doi:10.2214/AJR.07.3959
Batshaw ML, Tuchman M, Summar M, Seminara J, Members of the Urea Cycle Disorders Consortium (2014) A longitudinal study of urea cycle disorders. Mol Genet Metab 113:127–130. doi:10.1016/j.ymgme.2014.08.001
Bireley WR, Van Hove JLK, Gallagher RC, Fenton LZ (2012) Urea cycle disorders: brain MRI and neurological outcome. Pediatr Radiol 42:455–462. doi:10.1007/s00247-011-2253-6
Gropman A (2010) Brain imaging in urea cycle disorders. Mol Genet Metab 100(Suppl 1):S20–S30. doi:10.1016/j.ymgme.2010.01.017
Gunz AC, Choong K, Potter M, Miller E (2013) Magnetic resonance imaging findings and neurodevelopmental outcomes in neonates with urea-cycle defects. Int Med Case Rep J 6:41–48. doi:10.2147/IMCRJ.S43513
Pacheco-Colón I, Fricke S, VanMeter J, Gropman AL (2014) Advances in urea cycle neuroimaging: Proceedings from the 4th International Symposium on urea cycle disorders, Barcelona, Spain, September 2013. Mol Genet Metab 113:118–126. doi:10.1016/j.ymgme.2014.05.005
Ranger AM, Chaudhary N, Avery M, Fraser D (2012) Central pontine and extrapontine myelinolysis in children: a review of 76 patients. J Child Neurol 27:1027–1037. doi:10.1177/0883073812445908
Ruzek KA, Campeau NG, Miller GM (2004) Early diagnosis of central pontine myelinolysis with diffusion-weighted imaging. Am J Neuroradiol 25:210–213
Swoboda KJ, Saul JP, McKenna CE et al (2003) Aromatic L-amino acid decarboxylase deficiency: overview of clinical features and outcomes. Ann Neurol 54(Suppl 6):S49–S55. doi:10.1002/ana.10631
Gibson KM, Christensen E, Jakobs C et al (1997) The clinical phenotype of succinic semialdehyde dehydrogenase deficiency (4-hydroxybutyric aciduria): case reports of 23 new patients. Pediatrics 99:567–574
Parviz M, Vogel K, Gibson KM, Pearl PL (2014) Disorders of GABA metabolism: SSADH and GABA-transaminase deficiencies. J Pediatr Epilepsy 3:217–227. doi:10.3233/PEP-14097
Yalçinkaya C, Gibson KM, Gündüz E et al (2000) MRI findings in succinic semialdehyde dehydrogenase deficiency. Neuropediatrics 31:45–46
Acknowledgments
In memory of my dear friend, Massimo Gallucci, Professor of Neuroradiology.
Ethical standards and patient consent
We declare that this manuscript does not contain clinical studies or patient data.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zuccoli, G., Yannes, M.P., Nardone, R. et al. Bilateral symmetrical basal ganglia and thalamic lesions in children: an update (2015). Neuroradiology 57, 973–989 (2015). https://doi.org/10.1007/s00234-015-1568-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-015-1568-7