Abstract
Background
Despite the indications of carboxitherapy in situations of ischemia and necrosis, there is still no scientific evidence to support its clinical applicability. The purpose of this study was to investigate the effect of controlled carbon dioxide insufflation on the viability of dorsal ischemic random skin flaps in rats.
Methods
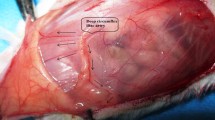
A randomized, single-blind, experimental study was conducted. Thirty-six Wistar-EPM rats were randomly distributed into three groups: group 1 (control using ischemic random skin flap procedure without gas insufflation); group 2 (flap procedure with controlled carbon dioxide insufflation); and group 3 (flap procedure with controlled inert gas insufflation). In groups 2 and 3, gas was insufflated intradermally in rats for 5 s (150 ml/min) using a 0.2-mm needle inserted at a 90° angle to the skin at two points (one located 2.5 cm from the cranial base of the flap and the other 7.5 cm from the midline of the flap). This procedure was repeated for 7 consecutive days. Macroscopic analysis (necrotic area) was performed using the paper-template method proposed by Sasaki and Pang. Microscopic analysis of the vascularization process was performed using hematoxylin and eosin staining.
Results
No statistically significant differences were found for the parameter vascularization, inflammatory infiltrate, and percentage of necrotic area.
Conclusions
Controlled carbon dioxide insufflation did not have a significant impact on the viability of ischemic random skin flaps.
Level of evidence: Not ratable.








Similar content being viewed by others
References
Rednam CK, Wilson RL, Selvaraju V, Rishi MT, Thirunavukkarasu M, Coca-Soliz V, Lakshmanan R, Palesty JA, McFadden DW, Maulik N (2017) Increased survivability of ischemic skin flap tissue in Flk-1+/- mice by Pellino-1 intervention. Microcirculation 24(6). https://doi.org/10.1111/micc.12362
Lucas JB (2017) The physiology and biomechanics of skin flaps. Facial Plast Surg Clin North Am 25(3):303–311. https://doi.org/10.1016/j.fsc.2017.03.003
Karimipour M, Amanzade V, Jabbari N, Farjah GH (2017) Effects of gamma-low dose irradiation on skin flap survival in rats. Phys Med 40:104–109. https://doi.org/10.1016/j.ejmp.2017.07.019
Prado RP, Liebano RE, Hochman BS, Pinfild CE, Ferreira LM (2006) Experimental models for low level laser therapy on isquemic random skin flap in rats. Acta Cir Bras 21:258–262. https://doi.org/10.1590/s0102-86502006000400013
Pinfild CE, Liebano RE, Hochman BS, Ferreira LM (2005) Hellim-neon laser in viability of randon skin flap in rats. Lasers Surg Med 37:74–77. https://doi.org/10.1002/lsm.20190
Nishioka MA (2012) Pinfild CE, Sheliga, TR, Arias VE, Gemes, HC, Ferreira LM: Led (660nm) and laser (670nm)use on skin flap viability: angiogenesis and mast cells on transition line. Lasers Med Sci 27:45–50. https://doi.org/10.1007/s10103-011-1042-7
Kerrigan CL (1983) Skin flap failure: pathophysiology. Plast Reconstr Surg 72(6):766–777. https://doi.org/10.1097/00006534-198312000-00003
Kailiang Z, Yihui Z, Dingsheng L, Xianyao T (2016) Effects of muscone on random skin flap survival in rats. J Reconstr Microsurg 32(3):200–207. https://doi.org/10.1055/s-0035-1565264
Junior IE, Masson IB, Ferreira LM, Liebano RE, Baldan C, Gomes AC (2005) Administração tópica de cloridrato de hidralazina na viabilidade de retalho cutâneo randômico em ratos [Topical administration of hydralazine hydrochloride on the viability of randon skin flaps in rats]. Acta Cir Bras. 20(2):164–7. https://doi.org/10.1590/s0102-86502005000200011 (Portuguese)
Barthe GP, Suarez NC, Ortega JMR (1991) Morphological changes in the vascularisation of delayed flaps in rabbits. Br J Plast Surg 4(4):285–290. https://doi.org/10.1016/0007-1226(91)90073-s
Duarte IS, Gomes HFC, Ferreira LM (1998) Effect of dimethyl sulphoxide on necrosis of skin flaps in rats. Can J Plast Surg 6(2):93–97. https://doi.org/10.1177/229255039800600205
Liebano RE, Ferreira LM, Sabino M (2003) Experimental model for transcutaneous electrical nerve stimulation on ischemic random skin flap in rats. Acta Cir Bras 18:54–59. https://doi.org/10.1590/S0102-86502003001100008
Harder Y, Amon M, Erni D, Menger MD (2004) Evolution of ischemic tissue injury in a random pattern flap: a new mouse model using intravital microscopy. J Surg Res 121(2):197–205. https://doi.org/10.1016/j.jss.2004.03.026
Abla LE, Gomes HC, Percario S, Ferreira LM (2005) Acetylcysteine in random skin flap in rats. Acta Cir Bras 20(2):121–123. https://doi.org/10.1590/s0102-86502005000200004
Doghaim NN, El-Tatawy RA, Neinaa YME, Abd El-Samd MM (2018) Study of the efficacy of carboxytherapy in alopecia. J Cosmet Dermatol 17(6):1275–1285. https://doi.org/10.1111/jocd.12501
Pianez LR, Custódio FS, Guidi RM, Nunes de Freitas J, Sant’Ana E (2016) Effectiveness of carboxytherapy in the treatment of cellulite in healthy women: a pilot study. Clin Cosmet Investig Dermatol 9:183–90. https://doi.org/10.2147/CCID.S102503
Brandi C, D’Anielo C, Grimaldi L, Bosi B, Dei I, Lattarulo P, Alessandrini C (2001) Carbon dioxide theraphy in the treatment of localized adiposities: clinical study and histopathological correlations. Aesthetic Plast Surg 25:170–74. https://doi.org/10.1007/s002660010116
Toriyama T, Kumada Y, Matsubara T, Murata A, Ogino A, Hayashi H, Nakashima H, Takahashi H, Matsuo H, Kawahara H (2002) Efeito do dióxido de carbono em pacientes portadores de arteriopatia periférica com isquemia crítica. Int Angiol 21(4):367–373
Bunyatyan ND, Drogovoz SM, Kononenko AV, Prokofiev AB (2018) Karboksiterapiia - odno iz innovatsionnykh napravleniĭ v kurortologii [Carboxytherapy - an innovative trend in resort medicine]. Vopr Kurortol Fizioter Lech Fiz Kult. 95(5):72–76. https://doi.org/10.17116/kurort20189505172 (Russian)
Ferreira JC, Haddad A, Tavares SA (2008) Increase in collagen turnover induced by intradermal injection of carbon dioxide in rats. J Drugs Dermatol 7(3):201–206
Ferreira LM, Silva EK, Jaimovich CA, Calazans D, Silva ER, Furtado FA, Cosac O, Nader P, Corrêa WEMY (2012) Carboxiterapia: buscando evidência para aplicação em cirurgia plástica e dermatologia. Rev Bras Cir Plástica 27:350–351. https://doi.org/10.1590/S1983-51752012000300002
Somez A, Yaman M, Yalcin O, Ersoy B, Serin M, Sav A (2009) Carbon dioxide therapy increases capillary formation on random pedicle skin flaps in the rat. J Plast Surg 62:236–37. https://doi.org/10.1016/j.bjps.2009.01.067
Sasaki GH, Pang CY (1980) Hemodynamics and viability of acute neurovascular island skin flaps in rats. Plast Reconstr Surg 65:152–158. https://doi.org/10.1097/00006534-198002000-00005
Korlof B, Ugland O (1966) Flaps and flap necrosis Improving the circulation in skin flaps with Complamin and with Dicoumarol: animal experiments. Acta Chir Scand 131(5):408–412
Qiu D, Wang X, Wang X, Jiao Y, Li Y, Jiang D (2019) Risk factors for necrosis of skin flap like wounds after ED debridement and suture. Am J Emerg Med 37(5):828–831. https://doi.org/10.1016/j.ajem.2018.07.049
Estevão LR, Medeiros JP, Baratella-Evêncio L, Simões RS, MendonçaFde S, Evêncio-Neto J (2013) Effects of the topical administration of copaiba oil ointment (Copaifera langsdorffii) in skin flaps viability of rats. Acta Cir Bras 28(12):863–869. https://doi.org/10.1590/s0102-86502013001200009
Peng-Fu Xu, Fang M-J, Jin Y-Z et al (2017) Effect of oxytocin on the survival of random skin flaps. Oncotarget 8(54):92955–92965. https://doi.org/10.18632/oncotarget.21696
Cury V, Bossini PS, Fangel R, Crusca Jde S, Renno AC, Parizotto NA (2009) The effects of 660nm and 780nm laser irradiation on viability of random skin flap in rats. Photomed Laser Surg 27(5):27–32. https://doi.org/10.1089/pho.2008.2383
Bossini PS, Fangel R, Habenschus RM, Renno AC, Benze B, Zuanon JA, Neto CB, Parizotto NA (2009) Low-level laser therapy (670 nm) on viability of random skin flap in rats. Lasers Med Sci 24(2):209–213. https://doi.org/10.1007/s10103-008-0551-5
Costa CS, Otoch JP, Seelander MCL, das Neves RX, Martinez CAR, Margarido NF (2011) Avaliação citométrica dos adipócitos localizados no subcutaneo da parede anterior do abdome após infiltração percutanea de CO2. Rev Col Bras Cir 38(1):15–23. https://doi.org/10.1590/S0100-69912011000100004
Savin E, Bailliart O, Bonnin P, Bedu M, Cheynel J, Coudert J, Martineaud JP (1995) Vasomotor effects of transcutaneous CO2 in stage II peripheral occlusive arterial disease. Angiology 46(9):785–791. https://doi.org/10.1177/000331979504600904
Lang EV, Gossler AA, Fick LJ et al (1999) Carbon dioxide angiography: effect of injection parameters on bolus configuration. J Vasc Interv Radiol 10:41–49. https://doi.org/10.1016/s1051-0443(99)70009-6
Brandi C, Grimaldi L, Nisi G, Brafa A, Campa A, Calambro M, Campana M, D’Aniello C (2010) The role of carbon dioxide therapy in the treatment of chronic wounds. In Vivo. 24(2):223–26
Alam M, Sadhwani D, Geisler A, Aslam I, Makin IRS, Schlessinger DI, Disphanurat W, Pongprutthipan M, Voravutinon N, Weil A, Chen BR, West DP, Veledar E, Poon E (2018) Subcutaneous infiltration of carbon dioxide (carboxytherapy) for abdominal fat reduction: a randomized clinical trial. J Am Acad Dermatol 79(2):320–326. https://doi.org/10.1016/j.jaad.2018.04.038
Podgórna K, Kołodziejczak A, Rotsztejn H (2018) Cutometric assessment of elasticity of skin with striae distensae following carboxytherapy. J Cosmet Dermatol 17(6):1170–1174. https://doi.org/10.1111/jocd.12465
Penhavel MV, Nascimento VH, Durães EF, Carneiro FP, Sousa JB (2013) Effects of carbon dioxide therapy on the healing of acute skin wounds induced on the back of rats. Acta Cir Bras 28(5):334–339. https://doi.org/10.1590/s0102-86502013000500003
Raymundo EC, Hochman B, Nishioka MA, Freitas JOG, Maximino JR, Chadi G (2014) Effects of subcutaneous carbon dioxide on calcitonin gene related peptide and substance P secretion in rat skin. Acta Cir Bras 29(4):224–230. https://doi.org/10.1590/s0102-86502014000400002
Valaro V, Manzo G, Mugnaini F, Bisacci C, Fiorucci P, Rango P, Bisacci R (2007) Carboxitherapy: effects on microcirculation and its use in treatment of severe lymphedema: a review. Acta Phelebol 8:1–13
Lyra MC, Leão Júnior H, Previde Neto S, Orgaes FAFS, Gonella HA (2012) Tratamento de queimaduras de carboxiterapia em modelo experimental. Rev Bras Queimaduras 11(1):2–5
Kołodziejczak A, Podgórna K, Rotsztejn H (2018) Is carboxytherapy a good alternative method in the removal of various skin defects? Dermatol Ther 31(5):e12699. https://doi.org/10.1111/dth.12699
Abramo AC, Teixeira TT (2011) Carboinsuflação em úlceras crônicas dos membros inferiores. Rev Bras Cirurg Plást 26(2):205–210. https://doi.org/10.1590/S1983-51752011000200005
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Mariana Merida Carrillo Negrao participated in study conception and design, data collection, analysis, and interpretation, the technical and surgical procedures, and in writing this manuscript.
Bernardo Sérgio Hochman Rzeszetkowski participated in study conception and design.
Luiz José Muaccad Gama participated in data collection, analysis, and interpretation and in the technical procedures.
José da Conceição Carvalho Júnior participated in critical revision and final approval of this manuscript.
Lydia Masako Ferreira participated in study conception and design and in the critical revision and final approval of this manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Research Ethics Committee and the Animal Use Ethics Committee of Federal University of São Paulo under number 0359/12. All use of animals was in agreement with the policies described in the Guide for the Care and Use of Laboratory Animals.
Consent for publication
Upon submission, all authors consent to the publication of the manuscript in the European Journal of Plastic Surgery.
Informed consent
None.
Conflict of interest
Mariana Merida Carrillo Negrao, Bernardo Sérgio Hochman Rzeszetkowski, Luiz José Muaccad Gama, José da Conceição Carvalho Júnior, and Lydia Masako Ferreira declare no competing interests.
Additional information
This work is dedicated to the memory of Bernardo Sérgio Hochman Rzeszetkowski.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Negrao, M.M.C., Rzeszetkowski, B.S.H., Gama, L.J.M. et al. The effect of controlled carbon dioxide insufflation on the viability of ischemic random skin flaps in rats. Eur J Plast Surg 44, 569–576 (2021). https://doi.org/10.1007/s00238-021-01851-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-021-01851-z