Abstract
Pediatric lumbar puncture can be challenging or unsuccessful for several reasons. At the same time, the excellent sonographic window into the pediatric spine provides a distinct opportunity for ultrasound-guided lumbar puncture. Minimal cerebrospinal fluid and thecal displacement by subdural or epidural hematomas are common after failed clinical attempts. Ultrasound is useful for determining a safe infraconal level for subarachnoid access. Real-time guidance increases not only the success rate but also the safety of diagnostic lumbar puncture and injections for chemotherapy and myelography. In this article, we discuss clinical and technical factors for ultrasound-guided pediatric lumbar puncture.








Similar content being viewed by others
References
Özdamar E, Özkaya AK, Güler E et al (2015) Ultrasound-assisted lumbar puncture in pediatric emergency department. Pediatr Emerg Care. doi:10.1097/PEC.0000000000000593
Nomura JT, Leech SJ, Shenbagamurthi S et al (2007) A randomized controlled trial of ultrasound-assisted lumbar puncture. J Ultrasound Med 26:1341–1348
Brousseau A-A, Parent DM-C (2016) Towards evidence based emergency medicine: Best BETs from the Manchester Royal Infirmary. BET 3: Advantages of ultrasound-assisted lumbar puncture. Emerg Med J 33:163–165
Strony R (2010) Ultrasound-assisted lumbar puncture in obese patients. Crit Care Clin 26:661–664
Shaikh F, Brzezinski J, Alexander S et al (2013) Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta-analysis. BMJ 346:f1720
Grau T, Leipold RW, Conradi R et al (2001) Ultrasound imaging facilitates localization of the epidural space during combined spinal and epidural anesthesia. Reg Anesth Pain Med 26:64–67
Coley DB, Shiels EW II, Hogan JM (2001) Diagnostic and interventional ultrasonography in neonatal and infant lumbar puncture. Pediatr Radiol 31:399–402
Abukawa Y, Hiroki K, Morioka N et al (2015) Ultrasound versus anatomical landmarks for caudal epidural anesthesia in pediatric patients. BMC Anesthesiol 15:102
Glatstein MM, Zucker-Toledano M, Arik A et al (2011) Incidence of traumatic lumbar puncture: experience of a large, tertiary care pediatric hospital. Clin Pediatr 50:1005–1009
Rankin J, Wang VJ, Goodarzian F et al (2016) Intravenous fluid bolus prior to neonatal and infant lumbar puncture: a sonographic assessment of the subarachnoid space after intravenous fluid administration. JAMA Pediatr 170:e154636
Park Y, Lee J-H, Park KD et al (2013) Ultrasound-guided vs. fluoroscopy-guided caudal epidural steroid injection for the treatment of unilateral lower lumbar radicular pain: a prospective, randomized, single-blind clinical study. Am J Phys Med Rehabil 92:575–586
Sandoval M, Shestak W, Stürmann K et al (2004) Optimal patient position for lumbar puncture, measured by ultrasonography. Emerg Radiol 10:179–181
Öncel S, Günlemez A, Anik Y et al (2013) Positioning of infants in the neonatal intensive care unit for lumbar puncture as determined by bedside ultrasonography. Arch Dis Child Fetal Neonatal Ed 98:F133–F135
Abo A, Chen L, Johnston P et al (2010) Positioning for lumbar puncture in children evaluated by bedside ultrasound. Pediatrics 125:e1149–e1153
Cadigan BA, Cydulka RK, Werner SL et al (2011) Evaluating infant positioning for lumbar puncture using sonographic measurements. Acad Emerg Med Off J Soc Acad Emerg Med 18:215–218
Nigrovic LE, Kuppermann N, Neuman MI (2007) Risk Factors for traumatic or unsuccessful lumbar punctures in children. Ann Emerg Med 49:762–771
Baxter AL, Fisher RG, Burke BL et al (2006) Local anesthetic and stylet styles: factors associated with resident lumbar puncture success. Pediatrics 117:876–881
Koch BL, Moosbrugger EA, Egelhoff JC (2007) Symptomatic spinal epidural collections after lumbar puncture in children. AJNR Am J Neuroradiol 28:1811–1816
Lo MD, Parisi MT, Brown JC et al (2013) Sitting or tilt position for infant lumbar puncture does not increase ultrasound measurements of lumbar subarachnoid space width. Pediatr Emerg Care 29:588–591
Wang PI, Wang AC, Naidu JO et al (2013) Sonographically guided lumbar puncture in pediatric patients. J Ultrasound Med 32:2191–2197
Hazra AK, Bhattacharya D, Mukherjee S et al (2016) Ultrasound versus fluoroscopy-guided caudal epidural steroid injection for the treatment of chronic low back pain with radiculopathy: a randomised, controlled clinical trial. Indian J Anaesth 60:388–392
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
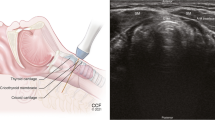
Appendix 1 Land-marking technique for lumbar puncture using ultrasound
Appendix 1 Land-marking technique for lumbar puncture using ultrasound
-
Patient is positioned in left lateral decubitus, flexed at hip and knee.
-
Sagittal ultrasound image is obtained to identify upper sacral margin (S1).
-
Ultrasound probe is moved cephalad to identify L3 and L4 vertebral body levels, which are marked by horizontal lines on the skin on either side of the probe.
-
Axial ultrasound scanning is performed to identify the midline (spinous process) at the L3 and L4 levels, and is marked by vertical lines on the skin to transect the previously marked horizontal lines.
-
Axial scanning is performed on the midline (vertical line) in the interspinous space (between the two horizontal lines) with gradual cephalad angulation of the transducer to obtain a clear view of the ligamentum flavum–posterior dura echogenicity. This transducer angle is eyeballed to determine the angle of needle entry.
-
Measurement of skin-to-posterior-dura distance is obtained in the last axial image.
-
Skin preparation and sterile draping are conducted.
-
The spinal needle is introduced into the L3–L4 interspace on the previously marked vertical line, along the predetermined angle.
Rights and permissions
About this article
Cite this article
Muthusami, P., Robinson, A.J. & Shroff, M.M. Ultrasound guidance for difficult lumbar puncture in children: pearls and pitfalls. Pediatr Radiol 47, 822–830 (2017). https://doi.org/10.1007/s00247-017-3794-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3794-0