Abstract
Background
Artificial intelligence models have been successful in analyzing ordinary photographic images. One type of artificial intelligence model is object detection, where a labeled bounding box is drawn around an area of interest. Object detection can be applied to medical imaging tasks.
Objective
To demonstrate object detection in identifying rickets and normal wrists on pediatric wrist radiographs using a small dataset, simple software and modest computer hardware.
Materials and methods
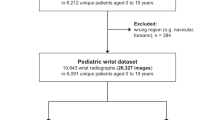
The institutional review board at Children’s Healthcare of Atlanta approved this study. The radiology information system was searched for radiographic examinations of the wrist for the evaluation of rickets from 2007 to 2018 in children younger than 7 years of age. Inclusion criteria were an exam type of “Rickets Survey” or “Joint Survey 1 View” with reports containing the words “rickets” or “rachitic.” Exclusion criteria were reports containing the words “renal,” “kidney” or “transplant.” Two pediatric radiologists reviewed the images and categorized them as either rickets or normal. Images were annotated by drawing a labeled bounding box around the distal radial and ulnar metaphases. The training dataset was created from images acquired from Jan. 1, 2007, to Dec. 31, 2017. This included 104 wrists with rickets and 264 normal wrists. This training dataset was used to create the object detection model. The testing dataset consisted of images acquired during the 2018 calendar year. This included 20 wrists with rickets and 37 normal wrists. Model sensitivity, specificity and accuracy were measured.
Results
Of the 20 wrists with rickets in the testing set, 16 were correctly identified as rickets, 2 were incorrectly identified as normal and 2 had no prediction. Of the 37 normal wrists, 33 were correctly identified as normal, 2 were incorrectly identified as rickets and 2 had no prediction. This yielded a sensitivity and specificity of 80% and 95% for wrists with rickets and 89% and 90% for normal wrists. Overall model accuracy was 86%.
Conclusion
Object detection can identify rickets on pediatric wrist radiographs. Object detection models can be developed with a small dataset, simple software tools and modest computing power.











Similar content being viewed by others
References
Asada N, Doi K, MacMahon H et al (1990) Potential usefulness of an artificial neural network for differential diagnosis of interstitial lung diseases: pilot study. Radiology 177:857–860
Gross GW, Boone JM, Greco-Hunt V, Greenberg B (1990) Neural networks in radiologic diagnosis; II. Interpretation of neonatal chest radiographs. Invest Radiol 25:1017–1023
Scott JA, Palmer EL (1993) Neural network analysis of ventilation-perfusion lung scans. Radiology 186:661–664
Tourassi GD, Floyd CE, Sostman HD, Coleman RE (1993) Acute pulmonary embolism: artificial neural network approach for diagnosis. Radiology 189:555–558
Boone JM (1993) Neural networks at the crossroads. Radiology 189:357–359
West E, Mutasa S, Zhu Z, Ha R (2019) Global trend in artificial intelligence–based publications in radiology from 2000 to 2018. AJR Am J Roentgenol 213:1204–1206
Boone JM, Gross GW, Greco-Hunt V (1990) Neural networks in radiologic diagnosis. I. Introduction and illustration. Investig Radiol 25:1012–1016
Reinus WR (1997) Machines that learn: can they learn to interpret radiographs? AJR Am J Roentgenol 169:19–21
Chartrand G, Cheng PM, Vorontsov E et al (2017) Deep learning: a primer for radiologists. Radiographics 37:2113–2131
Erickson BJ, Korfiatis P, Akkus Z, Kline TL (2017) Machine learning for medical imaging. Radiographics 37:505–515
Kahn CE Jr (2017) From images to actions: opportunities for artificial intelligence in radiology. Radiology 285:719–720
Kohli M, Prevedello LM, Filice RW, Geis JR (2017) Implementing machine learning in radiology practice and research. AJR Am J Roentgenol 208:754–760
Handelman GS, Kok HK, Chandra RV et al (2019) Peering into the black box of artificial intelligence: evaluation metrics of machine learning methods. AJR Am J Roentgenol 212:38–43
Moore MM, Slonimsky E, Long AD et al (2019) Machine learning concepts, concerns and opportunities for a pediatric radiologist. Pediatr Radiol 49:509–516
Soffer S, Ben-Cohen A, Shimon O et al (2019) Convolutional neural networks for radiologic images: a radiologist’s guide. Radiology 290:590–606
England JR, Gross JS, White EA et al (2018) Detection of traumatic pediatric elbow joint effusion using a deep convolutional neural network. AJR Am J Roentgenol 211:1361–1368
Larson DB, Chen MC, Lungren MP et al (2018) Performance of a deep-learning neural network model in assessing skeletal maturity on pediatric hand radiographs. Radiology 287:313–322
Halabi SS, Prevedello LM, Kalpathy-Cramer J et al (2019) The RSNA pediatric bone age machine learning challenge. Radiology 290:498–503
Rayan JC, Reddy N, Kan JH et al (2019) Binomial classification of pediatric elbow fractures using a deep learning multiview approach emulating radiologist decision making. Radiology: Artificial Intelligence 1:e180015
Reddy NE, Rayan JC, Annapragada AV et al (2020) Bone age determination using only the index finger: a novel approach using a convolutional neural network compared with human radiologists. Pediatr Radiol 50:516–523
Yi PH, Kim TK, Wei J et al (2019) Automated semantic labeling of pediatric musculoskeletal radiographs using deep learning. Pediatr Radiol 49:1066–1070
Mahomed N, van Ginneken B, Philipsen RHHM et al (2020) Computer-aided diagnosis for World Health Organization-defined chest radiograph primary-endpoint pneumonia in children. Pediatr Radiol 50:482–491
Otjen JP, Stanescu AL, Alessio AM, Parisi MT (2020) Ovarian torsion: developing a machine-learned algorithm for diagnosis. Pediatr Radiol 50:706–714
Zheng Q, Shellikeri S, Huang H et al (2020) Deep learning measurement of leg length discrepancy in children based on radiographs. Radiology 296:152–158
Shore RM, Chesney RW (2012) Rickets: part I. Pediatr Radiol 43:140–151
Creo AL, Thacher TD, Pettifor JM et al (2017) Nutritional rickets around the world: an update. Paediatr Int Child Health 37:84–98
Thacher TD, Fischer PR, Tebben PJ et al (2013) Increasing incidence of nutritional rickets: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc 88:176–183
Kawamura R RectLabel. https://rectlabel.com. Accessed 18 May 2020
Apple, Inc. Turi Create. https://github.com/apple/turicreate. Accessed 18 May 2020
Python Software Foundation Python. https://www.python.org. Accessed 18 May 2020
Project Jupyter. Jupyter. https://jupyter.org/index.html. Accessed 18 May 2020
Apple, Inc. How it works. https://apple.github.io/turicreate/docs/userguide/object_detection/how-it-works.html. Accessed 18 May 2020
Redmon J, Divvala S, Girshick R, Farhadi A (2015) You only look once: unified, real-time object detection. arXiv preprint arXiv:1506.02640
Redmon J, Farhadi A (2016) YOLO9000: better, faster, stronger. arXiv preprint arXiv:1612.08242
Sundaram M (1989) Renal osteodystrophy. Skeletal Radiol 18:415–426
Shore RM, Chesney RW (2013) Rickets: part II. Pediatr Radiol 43:152–172
Chang CY, Rosenthal DI, Mitchell DM et al (2016) Imaging findings of metabolic bone disease. Radiographics 36:1871–1887
Oestreich AE (2015) Concave distal end of ulna metaphysis alone is not a sign of rickets. Pediatr Radiol 45:998–1000
Thian YL, Li Y, Jagmohan P et al (2019) Convolutional neural networks for automated fracture detection and localization on wrist radiographs. Radiology: Artificial Intelligence 1:e180001. https://doi.org/10.1148/ryai.2019180001
Annarumma M, Withey SJ, Bakewell RJ et al (2019) Automated triaging of adult chest radiographs with deep artificial neural networks. Radiology 291:196–202
Seah JCY, Tang JSN, Kitchen A et al (2019) Chest radiographs in congestive heart failure: visualizing neural network learning. Radiology 290:514–522
Flanders AE, Prevedello LM, Shih G et al (2020) Construction of a machine learning dataset through collaboration: the RSNA 2019 brain CT hemorrhage challenge. Radiology: Artificial Intelligence 2:e190211. https://doi.org/10.1148/ryai.2020190211
Thomas KA, Kidziński Ł, Halilaj E et al (2020) Automated classification of radiographic knee osteoarthritis severity using deep neural metworks. Radiology: Artificial Intelligence 2:e190065. https://doi.org/10.1148/ryai.2020190065
Willemink MJ, Koszek WA, Hardell C et al (2020) Preparing medical imaging data for machine learning. Radiology 295:4–15
Liu F, Guan B, Zhou Z et al (2019) Fully automated diagnosis of anterior cruciate ligament tears on knee MR images by using deep learning. Radiology: Artificial Intelligence 1:180091
W3Schools Python Tutorial. https://www.w3schools.com/python/default.asp. Accessed 18 May 2020
Philbrick KA, Yoshida K, Inoue D et al (2018) What does deep learning see? Insights from a classifier trained to predict contrast enhancement phase from CT images. AJR Am J Roentgenol 211:1184–1193
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meda, K.C., Milla, S.S. & Rostad, B.S. Artificial intelligence research within reach: an object detection model to identify rickets on pediatric wrist radiographs. Pediatr Radiol 51, 782–791 (2021). https://doi.org/10.1007/s00247-020-04895-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-020-04895-8