Abstract
Purpose
To evaluate the impact of dedicated reader education on accuracy/confidence of peripheral zone index cancer and anterior prostate cancer (PCa) diagnosis with mpMRI; secondary aim was to assess the ability of readers to differentiate low-grade cancer (Gleason 6 or below) from high-grade cancer (Gleason 7+).
Materials and methods
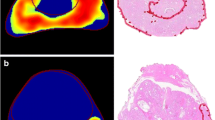
Five blinded radiology fellows evaluated 31 total prostate mpMRIs in this IRB-approved, HIPAA-compliant, retrospective study for index lesion detection, confidence in lesion diagnosis (1–5 scale), and Gleason grade (Gleason 6 or lower vs. Gleason 7+). Following a dedicated education program, readers reinterpreted cases after a memory extinction period, blinded to initial reads. Reference standard was established combining whole mount histopathology with mpMRI findings by a board-certified radiologist with 5 years of prostate mpMRI experience.
Results
Index cancer detection: pre-education accuracy 74.2%; post-education accuracy 87.7% (p = 0.003). Confidence in index lesion diagnosis: pre-education 4.22 ± 1.04; post-education 3.75 ± 1.41 (p = 0.0004). Anterior PCa detection: pre-education accuracy 54.3%; post-education accuracy 94.3% (p = 0.001). Confidence in anterior PCa diagnosis: pre-education 3.22 ± 1.54; post-education 4.29 ± 0.83 (p = 0.0003). Gleason score accuracy: pre-education 54.8%; post-education 73.5% (p = 0.0005).
Conclusions
A dedicated reader education program on PCa detection with mpMRI was associated with a statistically significant increase in diagnostic accuracy of index cancer and anterior cancer detection as well as Gleason grade identification as compared to pre-education values. This was also associated with a significant increase in reader diagnostic confidence. This suggests that substantial interobserver variability in mpMRI interpretation can potentially be reduced with a focus on education and that this can occur over a fellowship training year.


Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, et al. (2011) SEER Cancer Statistics Review, 1975–2010. National Cancer Institute, Bethesda, MD, based on November 2012 SEER data submission, posted to the SEER web site. http://www.seercancergov/csr/1975_2010. Accessed 8 June 2013.
Gupta RT, Kauffman CR, Polascik TJ, Taneja SS, Rosenkrantz AB (2013) The state of prostate MRI in 2013. Oncology 27(4):262–270
Mufarrij P, Sankin A, Godoy G, Lepor H (2010) Pathologic outcomes of candidates for active surveillance undergoing radical prostatectomy. Urology 76(3):689–692
Barentsz JO, Richenberg J, Clements R, et al. (2012) ESUR prostate MR guidelines 2012. Eur Radiol 22(4):746–757
Ruprecht O, Weisser P, Bodelle B, Ackermann H, Vogl TJ (2012) MRI of the prostate: interobserver agreement compared with histopathologic outcome after radical prostatectomy. Eur J Radiol 81(3):456–460
Mullerad M, Hricak H, Wang L, et al. (2004) Prostate cancer: detection of extracapsular extension by genitourinary and general body radiologists at MR imaging. Radiology 232(1):140–146
Noguchi M, Stamey TA, McNeal J, Nolley R (2003) Prognostic factors for multifocal prostate cancer in radical prostatectomy specimens: lack of significance of secondary cancers. J Urol 170(2):459–463
Wise AM, Stamey TA, McNeal JE, Clayton JL (2002) Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology 60(2):264–269
Rosenkrantz AB, Deng F-M, Kim S, et al. (2012) Prostate cancer: multiparametric MRI for index lesion localization: a multiple-reader study. AJR Am J Roentgenol 199(4):830–837
Turkbey B, Mani H, Shah V, et al. (2011) Multiparametric 3 T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol 186(5):1818–1824
Dickinson L, Ahmed HU, Allen C, et al. (2013) Scoring systems used for the interpretation and reporting of multiparametric MRI for prostate cancer detection, localization, and characterization: could standardization lead to improved utilization of imaging within the diagnostic pathway? J Magn Reson Imag 37(1):48–58
Dickinson L, Ahmed HU, Allen C, et al. (2011) Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: recommendations from a European consensus meeting. Eur Urol 59(4):477–494
Bott S, Young M, Kellett M, Parkinson M (2002) Anterior prostate cancer: is it more difficult to diagnose? BJU Int 89(9):886–889
Akin O, Riedl CC, Ishill NM, et al. (2010) Interactive dedicated training curriculum improves accuracy in the interpretation of MR imaging of prostate cancer. Eur Radiol 20(4):995–1002
Riches SF, Payne GS, Morgan VA, et al. (2009) MRI in the detection of prostate cancer: combined apparent diffusion coefficient, metabolite ratio, and vascular parameters. AJR Am J Roentgenol 193(6):1583–1591
Vourganti S, Rastinehad A, Yerram NK, et al. (2012) Multiparametric magnetic resonance imaging and ultrasound fusion biopsy detect prostate cancer in patients with prior negative transrectal ultrasound biopsies. J Urol 188(6):2152–2157
Tsivian M, Gupta RT et al. Multiparametric magnetic resonance imaging for detection and localization of prostate cancer: diagnostic properties (in press)
Eifler JB, Feng Z, Lin BM, et al. (2013) An updated prostate cancer staging nomogram (Partin tables) based on cases from 2006 to 2011. BJU Int 111(1):22–29
D’Amico AV, Whittington R, Malkowicz SB, et al. (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280(11):969–974
Kobus T, Vos PC, Hambrock T, et al. (2012) Prostate cancer aggressiveness: in vivo assessment of MR spectroscopy and diffusion-weighted imaging at 3 T. Radiology 265(2):457–467
Woodfield CA, Tung GA, Grand DJ, et al. (2010) Diffusion-weighted MRI of peripheral zone prostate cancer: comparison of tumor apparent diffusion coefficient with Gleason score and percentage of tumor on core biopsy. AJR Am J Roentgenol 194(4):W316–W322
Hambrock T, Somford DM, Huisman HJ, et al. (2011) Relationship between apparent diffusion coefficients at 3.0-T MR imaging and Gleason grade in peripheral zone prostate cancer. Radiology 259(2):453–461
Acknowledgments
The authors gratefully acknowledge the contributions of Steven Breault, M.D., Andrew Buck, M.D., Lauren Burke, M.D., Ghaneh Fananapazir, M.D., Alex Kim, M.D., Evan Kulbacki, M.D., Samantha Lipman, B.S., John Madden, M.D, Ph.D., Kathryn Nightingale, Ph.D., Arthur Parsee, M.D., and Jose Pratts, M.D., without whom this project would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was performed at the Departments of Radiology, Surgery and Biomedical Engineering at Duke University Medical Center.
Appendix: Multiparametric MRI acquisition parameters
Appendix: Multiparametric MRI acquisition parameters
Array spatial sensitivity-encoding technique (parallel imaging) factor of 2–3 was used in all sequences.
T2-weighted Imaging Parameters
-
TR range/TE range = 3700–4610/84–102 (milliseconds, ms)
-
Matrix size = 448 × 360 (Axial); 384 × 230–260 (Coronal, Sagittal)
-
Echo-train length = 25
-
Number of signals acquired = 3
-
Section thickness = 3 mm
-
Intersection gap = 0 mm
-
FOV = 16 cm
Diffusion-weighted imaging parameters
-
TR range/TE range = 8000/80
-
Matrix size = 160 × 160
-
b values = 0 and 800 s/mm2
-
Number of signals acquired = 6
-
Slice thickness = 3 mm
-
Gap = 0 mm
-
FOV = 16 cm
T1-weighted, 3D, gradient-echo, and free-breathing axial DCE MR images covering the entire prostate were acquired starting 11 s before the IV administration of gadopentetate dimeglumine (Magnevist, Bayer Pharma AG) at a dose of 0.1 mmol/kg, followed by a 20-mL saline flush at a rate of 2.0 mL/s.
DCE MRI Parameters
-
TR range/TE range = 4.09/1.44
-
Matrix size = 192 × 160
-
Flip angle = 15°
Interpolated slice thickness = 3 mm with temporal resolution of 5–6 s for approximately 5–6 min (approximately 70 sets of images were acquired to monitor the time course of contrast agent uptake and clearance within the prostate).
Rights and permissions
About this article
Cite this article
Garcia-Reyes, K., Passoni, N.M., Palmeri, M.L. et al. Detection of prostate cancer with multiparametric MRI (mpMRI): effect of dedicated reader education on accuracy and confidence of index and anterior cancer diagnosis. Abdom Imaging 40, 134–142 (2015). https://doi.org/10.1007/s00261-014-0197-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0197-7