Abstract
Purpose
The occurrence of thigh pain following cementless total hip arthroplasty (THA) may be dependent on multiple factors, which may differ with design of the prosthesis. Thus, this study aimed to investigate the frequency of thigh pain following cementless THA using a short, tapered-wedge stem to identify risk factors for thigh pain.
Methods
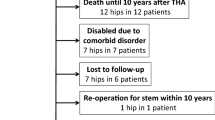
This retrospective cohort study analysed 222 joints of patients who underwent THA with a short, tapered-wedge stem. Thigh pain was evaluated using a questionnaire during each follow-up visit, and the clinical and radiographic assessments were compared.
Results
Thigh pain occurred in 37 patients (16.7%) during the follow-up period. The pain started two to 24 months after THA. Multivariate analysis demonstrated that higher University of California, Los Angeles, activity rating (odds ratio 7.2; 95% confidence interval (CI) 3.0–17.2); Dorr type C femoral bone shape (odds ratio 1.5; 95% CI 1.1–2.0); and stem tip-cortical bone contact (odds ratio 8.2; 95% CI 2.3–29.4) were significant risk factors of thigh pain following THA. Post-operatively, cortical hypertrophy at Gruen zone 4 was significantly found in patients with thigh pain (p value = 0.032).
Conclusion
Risk factors of pain following THA with short, tapered-wedge stem were high activity level, Dorr type C femoral bone shape, and stem tip contacting the distal bone surface. Moreover, post-operative cortical hypertrophy at the distal stem tip significantly increased the incidence of thigh pain. Therefore, we must pay attention to the aforementioned factors to avoid post-operative thigh pain when using a short, tapered-wedge stem.




Similar content being viewed by others
References
Caton J, Prudhon JL (2011) Over 25 years survival after Charnley’s total hip arthroplasty. Int Orthop 35:185–188. https://doi.org/10.1007/s00264-010-1197-z
Aldinger PR, Jung AW, Breusch SJ, Ewerbeck V, Parsch D (2009) Survival of the cementless Spotorno stem in the second decade. Clin Orthop Relat Res 467:2297–2304. https://doi.org/10.1007/s11999-009-0906-7
Pivec R, Johnson AJ, Mears SC, Mont MA (2012) Hip arthroplasty. Lancet 380:1768–1777. https://doi.org/10.1016/S0140-6736(12)60607-2
Barrack RL, Paprosky W, Butler RA, Palafox A, Szuszczewicz E, Myers L (2000) Patients’ perception of pain after total hip arthroplasty. J Arthroplast 15:590–596. https://doi.org/10.1054/arth.2000.6634
Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H (2006) Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand 50:495–500. https://doi.org/10.1111/j.1399-6576.2006.00976.x
Domb B, Hostin E, Mont MA, Hungerford DS (2000) Cortical strut grafting for enigmatic thigh pain following total hip arthroplasty. Orthopedics 23:21–24
Lavernia C, D’Apuzzo M, Hernandez VH, Lee DJ (2005) Patient-perceived outcomes in thigh pain after primary arthroplasty of the hip. Clin Orthop Relat Res 441:268–273. https://doi.org/10.1097/00003086-200512000-00041
Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L (1992) Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br 74:63–66
Nam D, Nunley RM, Clohisy JC, Lombardi AV, Berend KR, Barrack RL (2019) Does patient-reported perception of pain differ based on surgical approach in total hip arthroplasty? Bone Joint J 101-B:31–36. https://doi.org/10.1302/0301-620X.101B6.BJJ-2018-1575.R1
Nam D, Nunley RM, Sauber TJ, Johnson SR, Brooks PJ, Barrack RL (2015) Incidence and location of pain in young, active patients following hip arthroplasty. J Arthroplast 30:1971–1975. https://doi.org/10.1016/j.arth.2015.05.030
Engh CA, Bobyn JD (1988) The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res:7–28
Whiteside LA (1989) The effect of stem fit on bone hypertrophy and pain relief in cementless total hip arthroplasty. Clin Orthop Relat Res:138–147
Amendola RL, Goetz DD, Liu SS, Callaghan JJ (2017) Two- to 4-year followup of a short stem tha construct: excellent fixation, thigh pain a concern. Clin Orthop Relat Res 475:375–383. https://doi.org/10.1007/s11999-016-4974-1
Maier MW, Streit MR, Innmann MM, Kruger M, Nadorf J, Kretzer JP, Ewerbeck V, Gotterbarm T (2015) Cortical hypertrophy with a short, curved uncemented hip stem does not have any clinical impact during early follow-up. BMC Musculoskelet Disord 16:371. https://doi.org/10.1186/s12891-015-0830-9
Pepke W, Nadorf J, Ewerbeck V, Streit MR, Kinkel S, Gotterbarm T, Maier MW, Kretzer JP (2014) Primary stability of the Fitmore stem: biomechanical comparison. Int Orthop 38:483–488. https://doi.org/10.1007/s00264-013-2138-4
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 17-27
Dorr LD (1986) Total hip replacement using APR system. Tech Orthop 22
Engh CA, Bobyn JD, Glassman AH (1987) Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg (Br) 69:45–55
Noble PC, Box GG, Kamaric E, Fink MJ, Alexander JW, Tullos HS (1995) The effect of aging on the shape of the proximal femur. Clin Orthop Relat Res 31-44
Albers A, Aoude AA, Zukor DJ, Huk OL, Antoniou J, Tanzer M (2016) Favorable results of a short, tapered, highly porous, proximally coated cementless femoral stem at a minimum 4-year follow-up. J Arthroplast 31:824–829. https://doi.org/10.1016/j.arth.2015.08.020
Ulivi M, Orlandini LC, Meroni V, Lombardo MDM, Peretti GM (2018) Clinical performance, patient reported outcome, and radiological results of a short, tapered, porous, proximally coated cementless femoral stem: results up to seven years of follow-up. J Arthroplast 33:1133–1138. https://doi.org/10.1016/j.arth.2017.11.046
Pierannunzii LM (2008) Thigh pain after total hip replacement: a pathophysiological review and a comprehensive classification. Orthopedics 31:691–699; quiz 700-691. https://doi.org/10.3928/01477447-20110505-05
Dalury DF, Kelley TC, Adams MJ (2012) Modern proximally tapered uncemented stems can be safely used in Dorr type C femoral bone. J Arthroplast 27:1014–1018. https://doi.org/10.1016/j.arth.2011.12.019
Paul JP (1999) Strength requirements for internal and external prostheses. J Biomech 32:381–393. https://doi.org/10.1016/s0021-9290(98)00190-0
Tsubosaka M, Hayashi S, Hashimoto S, Takayama K, Kuroda R, Matsumoto T (2018) Patients with a Dorr type C femoral bone require attention for using a Summit cementless stem: results of total hip arthroplasty after a minimum follow-up period of 5 years after insertion of a Summit cementless stem. J Orthop Sci 23:671–675. https://doi.org/10.1016/j.jos.2018.05.001
Jo WL, Lee YK, Ha YC, Park MS, Lyu SH, Koo KH (2016) Frequency, developing time, intensity, duration, and functional score of thigh pain after cementless total hip arthroplasty. J Arthroplast 31:1279–1282. https://doi.org/10.1016/j.arth.2015.12.016
Fottner A, Woiczinski M, Kistler M, Schroder C, Schmidutz TF, Jansson V, Schmidutz F (2018) Varus malalignment of cementless hip stems provides sufficient primary stability but highly increases distal strain distribution. Clin Biomech (Bristol, Avon) 58:14–20. https://doi.org/10.1016/j.clinbiomech.2018.07.006
Braun A, Papp J, Reiter A (2003) The periprosthetic bone remodelling process--signs of vital bone reaction. Int Orthop 27(Suppl 1):S7–S10
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hayashi, S., Hashimoto, S., Matsumoto, T. et al. Risk factors of thigh pain following total hip arthroplasty with short, tapered-wedge stem. International Orthopaedics (SICOT) 44, 2553–2558 (2020). https://doi.org/10.1007/s00264-020-04762-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04762-z