Abstract
Objective
Poly(ADP-ribosyl) polymerases (PARPs) are nuclear enzymes with roles in DNA damage recognition and repair. PARP1 inhibition enhances the effects of DNA-damaging agents like doxorubicin. We sought to determine the recommended phase two dose (RP2D) of veliparib with pegylated liposomal doxorubicin (PLD) in breast and recurrent gynecologic cancer patients.
Methods
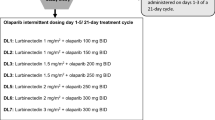
Veliparib and PLD were administered in a standard phase 1, 3 + 3 dose-escalation design starting at 50 mg veliparib BID on days 1–14 with PLD 40 mg/mg2 on day 1 of a 28-day cycle. Dose escalation proceeded in two strata: A (prior PLD exposure) and B (no prior PLD exposure). Patients underwent limited pharmacokinetic (PK) sampling; an expansion PK cohort was added.
Results
44 patients with recurrent ovarian or triple negative breast cancer were enrolled. Median age 56 years; 23 patients BRCA mutation carriers; median prior regimens four. Patients received a median of four cycles of veliparib/PLD. Grade 3/4 toxicities were observed in 10% of patients. Antitumor activity was observed in both sporadic and BRCA-deficient cancers. Two BRCA mutation carriers had complete responses. Two BRCA patients developed oral squamous cell cancers after completing this regimen. PLD exposure was observed to be higher when veliparib doses were > 200 mg BID.
Conclusions
The RP2D is 200 mg veliparib BID on days 1–14 with 40 mg/m2 PLD on day 1 of a 28-day cycle. Anti-tumor activity was seen in both strata. However, given development of long-term squamous cell cancers and the PK interaction observed, efforts should focus on other targeted combinations to improve efficacy.



Similar content being viewed by others
References
Amé J-C, Spenlehauer C, Murcia GD (2004) The PARP superfamily. Bio essays. 26(8):882–893
Farmer H et al (2005) Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434(7035):917–921
Schultz N, Lopez E, Saleh-Gohari N, Helleday T (2003) Poly(ADP-ribose) polymerase (PARP-1) has a controlling role in homologous recombination. Nucleic Acids Res. 31(17):4959–4964
Kummar S et al (2011) Phase 1 study of PARP inhibitor ABT-888 in combination with topotecan in adults with refractory solid tumors and lymphomas. Cancer Res. 71(17):5626–5634
LoRusso PM et al (2016) Phase 1 safety, pharmacokinetic, and pharmacodynamic study of the poly(ADP-ribose) polymerase (PARP) inhibitor veliparib (ABT-888) in combination with irinotecan in patients with advanced solid tumors. Clin Cancer Res. 22(13):3227–3237
Coleman et al (2015) A phase II evaluation of the potent, highly selective PARP inhibitor veliparib in the treatment of persistent or recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer in patients who carry a germline BRCA1 or BRCA2 mutation—an NRG oncology/gynecologic oncology group study. Gynecol Oncol 137(3):386–391
Olsen EA, Kim YH, Kuzel TM et al (2007) Phase IIB multicenter trial of vorinostat in patients with persistent, progressive, or treatment refractory cutaneous T-cell lymphoma. J Clin Oncol 25(21):3109–3115
Munoz-Gamez JA et al (2005) PARP inhibition sensitizes p53-deficient breast cancer cells to doxorubicin-induced apoptosis. Biochem J 386(1):119–125
Uziely B et al (1995) Liposomal doxorubicin: antitumor activity and unique toxicities during two complementary phase I studies. J Clin Oncol 13(7):1777–1785
Muggia FM et al (1997) Phase II study of liposomal doxorubicin in refractory ovarian cancer: antitumor activity and toxicity modification by liposomal encapsulation. J Clin Oncol 15(3):987–993
Gordon AN et al (2000) Phase II study of liposomal doxorubicin in platinum- and paclitaxel-refractory epithelial ovarian cancer. J Clin Oncol 18(17):3093–3100
Gordon AN, Fleagle JT, Guthrie D et al (2001) Recurrent epithelial ovarian carcinoma: a randomized phase III study of pegylated liposomal doxorubicin versus topotecan. J Clin Oncol 19(14):3312–3322
O’Brien et al (2004) Reduced cardiotoxicity and comparable efficacy in a phase III trial of pegylated liposomal doxorubicin HCl (CAELYX/Doxil) versus conventional doxorubicin for first-line treatment of metastatic breast cancer. Ann Oncol 15(3):440–449
Muggia C, Safra C (2011) Delayed neoplastic and renal complications in women receiving long-term chemotherapy for recurrent ovarian cancer. J Natl Cancer Inst 103(2):160–161
Nicoletto et al (2006) Phase II study of pegylated liposomal doxorubicin and oxaliplatin in relapsed advanced ovarian cancer. Gynecol Oncol. 100(2):318–323
Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. National Cancer Institute, June 14, 2010. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/CTCAE_4.03.xlsx
Eisenhauer EA et al (2009) New response evaluation criteria in solid tumors: revised RECIST guidelines (Version 1.1). Eur J Cancer 45(2):228–247
Gabizon A et al (2008) An open-label study to evaluate dose and cycle dependence of the pharmacokinetics of pegylated liposomal doxorubicin. Cancer Chemother Pharmacol 61(4):695–702
Parise RA, Shawaqhef M, Egorin MJ, Beumer JH (2008) Liquid chromatography–mass spectrometric assay for the quantitation in human plasma of ABT-888, an orally available, small molecule inhibitor of Poly(ADP-ribose)polymerase. J Chromatogr B 872(1–2):141–147
Muggia F (2013) Squamous cell carcinomas of the tongue and oral cavity as secondary malignancies: what factors are implicated? Oncologist 18(3):245–247
Cannon TL et al (2012) Squamous cell carcinoma of the oral cavity in nonsmoking women: a new and unusual complication of chemotherapy for recurrent Ovarian cancer? Oncologist 17(12):1541–1546
Oliveira-Costa JP et al (2014) BRCA1 and γH2AX as independent prognostic markers in oral squamous cell carcinoma. Oncoscience 1(5):383–391
Akbari MR et al (2008) Germline BRCA2 mutations and risk of esophageal squamous cell carcinoma. Oncogene 27(9):1290–1296
Fong PC et al (2009) Inhibition of Poly(ADP-ribose) Polymerase in tumors from BRCA mutation carriers. N Engl J Med 361(2):123–134
Gordon AN et al (2004) Long-term survival advantage for women treated with pegylated liposomal doxorubicin compared with topotecan in a phase 3 randomized study of recurrent and refractory epithelial ovarian cancer. Gynecol Oncol. 95(1):1–8
Kaye SB et al (2012) Phase II, open-label, randomized, multicenter study comparing the efficacy and safety of olaparib, a poly (ADP-ribose) polymerase inhibitor, and pegylated liposomal doxorubicin in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer. J Clin Oncol 30(4):372–379
Sapir R et al (2008) An open-label study to evaluate dose and cycle dependence of the pharmacokinetics of pegylated liposomal doxorubicin. Cancer Chemother Pharmacol 61(4):695–702
Gabzion A, Shmeeda H, Grenader T (2012) Pharmacological basis of pegylated liposomal doxorubicin: impact of cancer therapy. Eur J Pharm Sci 45(4):388–398
La-Beck NM et al (2012) Factors affecting the pharmacokinetics of pegylated liposomal doxorubicin in patients. Cancer Chemother Pharmacol 69(1):43–50
Ansari L et al (2017) The most prevalent side effects of pegylated liposomal doxorubicin monotherapy in women with metastatic breast cancer: a systematic review of clinical trials. Cancer Gene Ther 24(5):189–193
Smorenburg CH et al (2014) A randomized phase III study comparing pegylated liposomal doxorubicin with capecitabine as first-line chemotherapy in elderly patients with metastatic breast cancer: results of the omega study of the Dutch breast cancer research group BOOG. Ann Oncol. 25(3):99–605
Harbeck N et al (2016) A randomized phase III study evaluating pegylated liposomal doxorubicin versus capecitabine as first-line therapy for metastatic breast cancer: results of the PELICAN study. Breast Cancer Res Treat 161(1):63–72
Marth C et al (2017) ENGOT-ov-6/TRINOVA-2: randomised, double-blind, phase 3 study of pegylated liposomal doxorubicin plus trebananib or placebo in women with recurrent partially platinum-sensitive or resistant Ovarian cancer. Eur J Cancer 70:111–121
Soumerai JD et al (2017) The PARP inhibitor veliparib can be safely added to bendamustine and rituximab and has preliminary evidence of activity in B-cell lymphoma. Clin Cancer Res 23(15):4119–4126
Stoller R et al (2017) Phase I study of veliparib in combination with gemcitabine. Cancer Chemother Pharmacol. 80(3):631–643
Niu J et al (2017) Parent-metabolite pharmacokinetic modeling and pharmacodynamics of veliparib (ABT-888), a PARP inhibitor, in patients with BRCA 1/2-mutated cancer or parp-sensitive tumor types. J Clin Pharmacol 57(8):977–987
Landrum LE et al (2016) A phase I trial of pegylated liposomal doxorubicin, carboplatin, bevacizumab, and veliparib in recurrent, platinum-sensitive ovarian, primary peritoneal and fallopian tube cancer: an NRG oncology/gynecologic oncology group study. Gynecol Oncol 140(2):204–209
AbbVie (2017) AbbVie announces topline results from two phase 3 studies investigating veliparib in combination with chemotherapy for the treatment of patients with advanced or metastatic squamous non-small cell lung cancer and early-stage triple-negative breast cancer. https://news.abbvie.com/news/abbvie-announces-topline-results-from-two-phase-3-studies-investigating-veliparib-in-combination-with-chemotherapy-for-treatment-patients-with-advanced-or-metastatic-squamous-non-small-cell-lung-cancer-and-early-stage-triple-negative-breast-cancer.htm. Accessed 1 May 2019
Han HS et al (2018) Veliparib with temozolomide or carboplatin/paclitaxel versus placebo with BRCA1/2 locally recurrent/metastatic breast cancer: randomized phase II study. Ann Oncol. 29(1):154–161
Author information
Authors and Affiliations
Contributions
Dr. BP, Dr. JAS, Dr. SVB, Dr. LV, Dr. DLH, Dr. AT, and Dr. FM are oncologists who participated in this clinical trial by enrolling patients. Dr. AB analyzed the data sets for this trial and assisted Dr. BP in writing the manuscript. Dr. MK analyzed and calculated the statistics for this manuscript. BFK and JHB completed the veliparib pharmacokinetics portions of this trial and assisted in writing these sections of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Pothuri reports grants from NIH/NCI CRADL award (US Government), which were awarded to specifically fund this project. Dr. Pothuri reports consulting fees from Tesaro, Astra Zeneca and Eisai. Dr. Beumer reports research funding to his institute from AbbVie. He has also declared a conflict of interest with the National Cancer Institute (NCI), he has received grant funding, P30CA047904 and UM1CA186690. Dr. Tiersten reports consulting fees and non-financial support from Puma, Astra Zeneca, Novartis, Eisai, Genetech-roche, and Immunomedics, all outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pothuri, B., Brodsky, A.L., Sparano, J.A. et al. Phase I and pharmacokinetic study of veliparib, a PARP inhibitor, and pegylated liposomal doxorubicin (PLD) in recurrent gynecologic cancer and triple negative breast cancer with long-term follow-up. Cancer Chemother Pharmacol 85, 741–751 (2020). https://doi.org/10.1007/s00280-020-04030-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-020-04030-2