Abstract
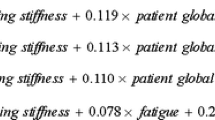
There is an ongoing quest for robust disease activity measures in Ankylosing spondylitis (AS). Thus, we prospectively validated two new disease activity indices, Simplified AS Disease Activity Score (SASDAS) and modified Juvenile Spondyloarthritis Disease Activity Score (JSpADA). Patients with AS were assessed for BASDAI, ASDAS and other outcome measures at baseline and 3 months. Comparisons were drawn between those with juvenile onset, early disease and peripheral involvement, with the rest. Fisher’s r to Z transformation was used to compare correlations. Receiver-operating characteristic (ROC) curves were used to calculate cutoffs for inactive, low, high and very high disease activity. Of the 107 patients (mean age—29 years) of 6-years long disease, 38.3% had a juvenile onset. SASDAS and modified JSpADA exhibited excellent correlation with BASDAI and ASDAS (all p < 0.001) and were higher in active vs. inactive disease. Treatment responders had a greater fall in SASDAS and modified JSpADA as compared to non-responders. The novel scores were higher in those with peripheral disease. Only SASDAS could discriminate early from late disease. Based on the previously proposed cutoffs, optimal scores for inactive, moderate, high and very high disease activity were deduced. SASDAS-CRP showed better internal consistency than SASDAS-ESR and correlated better with ASDAS-CRP in late disease (Z = 3.04; p = 002) and those with adult onset disease (Z = 2.18; p = 0.03). SASDAS and Modified JSpADA perform as well as standard complex scores and have potential for simpler daily use. From our analyses, SASDAS with CRP performs better than SASDAS-ESR, pending further validation.

Similar content being viewed by others
References
Colbert RA (2010) Classification of juvenile spondyloarthritis: enthesitis-related arthritis and beyond. Nat Rev Rheum 6:477–485. https://doi.org/10.1038/nrrheum.2010.103
Flatø B, Hoffmann-Vold AM, Reiff A, Førre Ø, Lien G, Vinje O (2006) Long-term outcome and prognostic factors in enthesitis-related arthritis: a case-control study. Arthritis Rheum 54:3573–3582
Enlow RW, Bias WB, Bluestone R, Arnett FC (1982) Human Lymphocyte Response to Selected Infectious Agents in Reiter’s Syndrome and Ankylosing Spondylitis. Rheum Int 1:171–175. https://doi.org/10.1007/BF00541172
Gupta L, Bhattacharya S, Agarwal V, Aggarwal A (2016) Elevated levels of serum MRP8/14 in ankylosing spondylitis: associated with peripheral arthritis and active disease. Clin Rheumatol 35:3075–3079
Bhattacharya S, Misra R, Aggarwal A (2020) Patients with enthesitis related arthritis show similar monocyte function pattern as seen in adult axial spondyloarthropathy. Pediatr Rheumatol Online J 18:6. https://doi.org/10.1186/s12969-020-0403-9
Gupta L, Ahmed S, Choudhury GD, Misra DP, Agarwal V (2018) Poor quality of life in Indian ankylosing spondylitis patients. Ind J Rheumatol 13:101. https://doi.org/10.4103/injr.injr_108_17
Malaviya AN (2020) Spondyloarthritis in India. Ind J Rheumatol 15:2. https://doi.org/10.4103/0973-3698.284742
Weiss PF, Beukelman T, Schanberg LE, Kimura Y, Colbert RA (2012) CARRA Registry Investigators Enthesitis-related arthritis is associated with higher pain intensity and poorer health status in comparison with other categories of juvenile idiopathic arthritis: the Childhood Arthritis and Rheumatology Research Alliance Registry. J Rheumatol 39:2341–2351
Hamilton-West KE, Quine L (2009) Living with Ankylosing Spondylitis: the patient's perspective. J Health Psychol 14:820–830. https://doi.org/10.1177/1359105309341394
Heuft-Dorenbosch L, van Tubergen A, Spoorenberg A, Landewé R, Dougados M, Mielants H, van der Tempel H, van der Heijde D (2004) The influence of peripheral arthritis on disease activity in ankylosing spondylitis patients as measured with the Bath Ankylosing Spondylitis Disease Activity Index. Arthritis Rheum 51:154–159
Lukas C, Landewé R, Sieper J et al (2009) Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Diss 68:18–24
Aranda-Valera IC, Garrido-Castro JL, Ladehesa-Pineda L, Vazquez-Mellado J, Zarco P, Juanola X, Gonzalez-Navas C, Font-Ugalde P, Castro-Villegas MC (2019) How to calculate the ASDAS based on C-reactive protein without individual questions from the BASDAI: the BASDAI- based ASDAS formula. Rheumatology. https://doi.org/10.1093/rheumatology/kez480
Sommerfleck FA, Schneeberger EE, Buschiazzo EE, Maldonado Cocco JA, Citera G (2012) A simplified version of Ankylosing Spondylitis Disease Activity Score (ASDAS) in patients with Ankylosing spondylitis. Clin Rheumatol 31:1599–1603. https://doi.org/10.1007/s10067-012-2056-7
Bansal N, Duggal L, Jain N (2017) Validity of simplified Ankylosing Spondylitis Disease Activity Scores (SASDAS) in Indian Ankylosing spondylitis patients. J Clin Diagn Res 11:OC06–OC09. https://doi.org/10.7860/JCDR/2017/22665.10540
Weiss PF, Colbert RA, Xiao R, Feudtner C, Beukelman T, DeWitt EM, Pagnini I, Wright TB, Wallace CA (2014) Development and retrospective validation of the juvenile spondyloarthritis disease activity index. Arthritis Care Res 66:1775–1782. https://doi.org/10.1002/acr.22411
Gupta L, Bhattacharya S, Aggarwal A (2018) Tenascin-C, a biomarker of disease activity in early Ankylosing spondylitis. Clin Rheumatol 37:1401–1405. https://doi.org/10.1007/s10067-017-3938-5
Zanwar A, Phatak S, Aggarwal A (2018) Prospective validation of the Juvenile Spondyloarthritis Disease Activity Index in children with enthesitis-related arthritis. Rheumatology (Oxford) 57:2167–2171. https://doi.org/10.1093/rheumatology/key246
Machado P, Landewé R, Lie E, Kvien TK, Braun J, Baker D, van der Heijde D (2011) Assessment of SpondyloArthritis international Society. Ankylosing Spondylitis Disease Activity Score (ASDAS): defining cut-off values for disease activity states and improvement scores. Ann Rheum Dis 70:47–53. https://doi.org/10.1136/ard.2010.138594
Madsen OR (2018) Stability of fatigue, pain, patient global assessment and the Bath Ankylosing Spondylitis Functional Index (BASFI) in spondyloarthropathy patients with stable disease according to the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). Rheumatol Int 38:425–432. https://doi.org/10.1007/s00296-017-3920-1
Khan NA, Spencer HJ, Abda E et al (2012) Determinants of discordance in patients' and physicians' rating of rheumatoid arthritis disease activity. Arthritis Care Res 64:206–214. https://doi.org/10.1002/acr.20685
Spoorenberg A, van Tubergen A, Landewé R et al (2005) Measuring disease activity in ankylosing spondylitis: patient and physician have different perspectives. Rheumatology 44:789–795. https://doi.org/10.1093/rheumatology/keh595
Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands. Available from: https://www.das-score.nl. Accessed 26 June 2020
Bakker C, Boers M, van der Linden S (1993) Measures to assess ankylosing spondylitis: taxonomy, review and recommendations. J Rheumatol 20:1724–1730
Brandt J, Westhoff G, Rudwaleit M et al (2003) Validierung einer deutschen Version des Fragebogens BASDAI zur Messung der Krankheitsaktivität bei ankylosierender Spondylitis [Adaption and validation of the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) for use in Germany]. Z Rheumatol 62:264–273. https://doi.org/10.1007/s00393-003-0522-y
Stone MA, Inman RD, Wright JG, Maetzel A (2004) Validation exercise of the Ankylosing Spondylitis Assessment Study (ASAS) group response criteria in ankylosing spondylitis patients treated with biologics. Arthritis Rheum 51:316–320. https://doi.org/10.1002/art.20414
Rudwaleit M, Haibel H, Baraliakos X et al (2009) The early disease stage in axial spondyloarthritis: results from the German Spondyloarthritis Inception Cohort. Arthritis Rheum 60:717–727. https://doi.org/10.1002/art.24483
Ostergaard M, Poggenborg RP, Axelsen MB, Pedersen SJ (2010) Magnetic resonance imaging in spondyloarthritis—how to quantify findings and measure response. Best Pract Res Clin Rheumatol 24:637–657. https://doi.org/10.1016/j.berh.2010.06.001
Bennett AN, McGonagle D, O'Connor P et al (2008) Severity of baseline magnetic resonance imaging-evident sacroiliitis and HLA-B27 status in early inflammatory back pain predict radiographically evident ankylosing spondylitis at eight years. Arthritis Rheum 58:3413–3418. https://doi.org/10.1002/art.24024
Nygaard A, Jurik AG, Lund C, Schiøttz-Christensen B (2019) The incidence of bone marrow oedema at the sacroiliac joints in a non-rheumatological population—a retrospective cohort study. BMC Musculoskelet Disord 20:590. https://doi.org/10.1186/s12891-019-2978-1
Sun L, Wu R, Xue Q, Wang F, Lu P (2016) Risk factors of uveitis in ankylosing spondylitis. Medicine 95(28):e4233. https://doi.org/10.1097/MD.0000000000004233
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
LG was involved in ideation, data collection, analysis and manuscript preparation. STG was involved in data analysis and manuscript preparation. HM was involved in data analysis. All authors critically reviewed the manuscript for intelligent inputs. All co-authors have read the final version, approve it and take full responsibility for the integrity of the study and the final manuscript has already been mentioned in the title file.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval information
Due ethics permissions were obtained from the institute ethics committee of SGPGIMS, Lucknow as per local guidelines.
Data sharing statement
All the data pertaining to the study are included in the manuscript and as supplementary material. Previously data presented as a poster at the Indian Rheumatology Association Conference 2019: T G Sundaram (2019). Validation of simplified disease activity score for ankylosing spondylitis. PC0160. IRACON. Indian Journal of Rheumatology.2019: 14 (6)Supplement. S196.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sundaram, T.G., Muhammed, H., Aggarwal, A. et al. A prospective study of novel disease activity indices for ankylosing spondylitis. Rheumatol Int 40, 1843–1849 (2020). https://doi.org/10.1007/s00296-020-04662-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-020-04662-w