Abstract
Objectives
To develop an anthropomorphic phantom closely mimicking patient anatomy and to evaluate the phantom for the simulation of computed tomography (CT)-guided procedures.
Methods
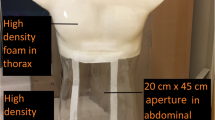
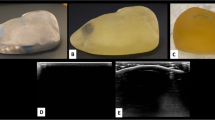
Patient CT images were printed with aqueous potassium iodide solution (1 g/mL) on paper. The printed paper sheets were stacked in alternation with 1-mm thick polyethylene foam layers, cut to the patient shape and glued together to create an anthropomorphic abdomen phantom. Ten interventional radiologists performed periradicular infiltration on the phantom and rated the phantom procedure regarding different aspects of suitability for simulating CT-guided procedures.
Results
Radiopaque printing in combination with polyethylene foam layers achieved a phantom with detailed patient anatomy that allowed needle placement. CT-guided periradicular infiltration on the phantom was rated highly realistic for simulation of anatomy, needle navigation and overall course of the procedure. Haptics were rated as intermediately realistic. Participants strongly agreed that the phantom was suitable for training and learning purposes.
Conclusions
A radiopaque 3D printed, anthropomorphic phantom provides a realistic platform for the simulation of CT-guided procedures. Future work will focus on application for training and procedure optimisation.
Key Points
• Radiopaque 3D printing combined with polyethylene foam achieves patient phantoms for CT-guided procedures.
• Radiopaque 3D printed, anthropomorphic phantoms allow realistic simulation of CT-guided procedures.
• Realistic visual guidance is a key aspect in simulation of CT-guided procedures.
• Three-dimensional printed phantoms provide a platform for training and optimisation of CT-guided procedures.




Similar content being viewed by others
References
Ahlberg G, Enochsson L, Gallagher AG et al (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
MacDonald J, Ketchum J, Williams RG, Rogers LQ (2003) A lay person versus a trained endoscopist: can the preop endoscopy simulator detect a difference? Surg Endosc 17:896–898
Waterman BR, Martin KD, Cameron KL, Owens BD, Belmont PJ (2016) Simulation training improves surgical proficiency and safety during diagnostic shoulder arthroscopy performed by residents. Orthopedics 39:e479–e485
Thomsen AS, Bach-Holm D, Kjærbo H et al (2017) Operating room performance improves after proficiency-based virtual reality cataract surgery Training. Ophthalmology 124:524–531
Draycott TJ, Crofts JF, Ash JP et al (2008) Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol 112:14–20
Pannell JS, Santiago-Dieppa DR, Wali AR et al (2016) Simulator-based angiography and endovascular neurosurgery curriculum: a longitudinal evaluation of performance following simulator-based angiography training. Cureus 8:e756
Barsuk JH, McGaghie WC, Cohen ER, O'Leary KJ, Wayne DB (2009) Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med 37:2697–2701
Zendejas B, Cook DA, Bingener J et al (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg 254:502–509 discussion 509-511
Cohen ER, Feinglass J, Barsuk JH et al (2010) Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simul Healthc 5:98–102
Gomoll AH, O'Toole RV, Czarnecki J, Warner JJ (2007) Surgical experience correlates with performance on a virtual reality simulator for shoulder arthroscopy. Am J Sports Med 35:883–888
Dimmick S, Jones M, Challen J, Iedema J, Wattuhewa U, Coucher J (2007) CT-guided procedures: evaluation of a phantom system to teach accurate needle placement. Clin Radiol 62:166–171
Mendiratta-Lala M, Williams TR, Mendiratta V, Ahmed H, Bonnett JW (2015) Simulation center training as a means to improve resident performance in percutaneous noncontinuous CT-guided fluoroscopic procedures with dose reduction. AJR Am J Roentgenol 204:W376–W383
Gruber-Rouh T, Lee C, Bolck J et al (2015) Intervention planning using a laser navigation system for ct-guided interventions: a phantom and patient study. Korean J Radiol 16:729–735
Jacobi V, Thalhammer A, Kirchner J (1999) Value of a laser guidance system for CT interventions: a phantom study. Eur Radiol 9:137–140
Moser C, Becker J, Deli M, Busch M, Boehme M, Groenemeyer DH (2013) A novel Laser Navigation System reduces radiation exposure and improves accuracy and workflow of CT-guided spinal interventions: a prospective, randomized, controlled, clinical trial in comparison to conventional freehand puncture. Eur J Radiol 82:627–632
Nitta N, Takahashi M, Tanaka T et al (2007) Laser-guided computed tomography puncture system: simulation experiments using artificial phantom lesions and preliminary clinical experience. Radiat Med 25:187–193
Jahnke P, Limberg FR, Gerbl A et al (2017) Radiopaque three-dimensional printing: a method to create realistic CT phantoms. Radiology 282:569–575
Feigl GC, Dreu M, Kastner M et al (2017) Thermocoagulation of the medial branch of the dorsal branch of the lumbal spinal nerve: flouroscopy versus CT. Pain Med 18:36–40
Kroes MW, Busser WM, Fütterer JJ et al (2013) Assessment of needle guidance devices for their potential to reduce fluoroscopy time and operator hand dose during C-arm cone-beam computed tomography-guided needle interventions. J Vasc Interv Radiol 24:901–906
Schulz B, Eichler K, Siebenhandl P et al (2013) Accuracy and speed of robotic assisted needle interventions using a modern cone beam computed tomography intervention suite: a phantom study. Eur Radiol 23:198–204
Won HJ, Kim N, Kim GB, Seo JB, Kim H (2017) Validation of a CT-guided intervention robot for biopsy and radiofrequency ablation: experimental study with an abdominal phantom. Diagn Interv Radiol 23:233–237
Acknowledgements
We thank Christian Althoff, Torsten Diekhoff, Felix Doellinger, Ahi Sema Issever, Matthias Rief, Valentina Romano, Musaab Saleh, Regina Thiel and Elke Zimmermann of the Department of Radiology, Charité–Universitätsmedizin Berlin.
Funding
This study has received funding by the Bundesministerium für Wirtschaft und Energie (DE): 03EFHBE093.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Paul Jahnke.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Patents
Patent applications for the 3D printing method were filed by Dr. Jahnke and PD Dr. Scheel: DE202015104282U1, EP000003135199A1, US020170042501A1.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• observational
• performed at one institution
Rights and permissions
About this article
Cite this article
Jahnke, P., Schwarz, F.B., Ziegert, M. et al. A radiopaque 3D printed, anthropomorphic phantom for simulation of CT-guided procedures. Eur Radiol 28, 4818–4823 (2018). https://doi.org/10.1007/s00330-018-5481-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5481-4