Abstract
Purpose
Data assessing the effectiveness of intracavernosal injections (ICIs) for the treatment of erectile dysfunction (ED) are limited. This study evaluates intracavernosal injectable therapies for ED and reviews available guidelines that inform clinical practice.
Methods
A systematic search using electronic databases (Medline, Pubmed) was performed for studies investigating injectable management strategies for ED published after 1990. Primary outcome measures were to comparatively evaluate clinical efficacy, continuation rates and adverse event profiles of each injectable agent as monotherapy or in combination. The secondary outcome measurement was to discuss available guidelines that inform clinical practice for injectable agents.
Results
ICIs demonstrate clinical efficacy in 54–100% of patients, early discontinuation rates of ≤ 38% and adverse events in ≤ 26%. Discontinuation rates are typically greatest within 3–6 months of commencement. Anxiety related to the initial injection occurs in approximately 65% and anxiety levels can remain high for 4 months. Approval of intracavernosal injection agents is mainly limited to alprostadil with the recent addition of aviptadil/phentolamine combination therapy in a select few geographical regions. Although combination therapies are attractive alternative options, their formulations are variable and should be standardised before widespread acceptance is achieved.
Conclusions
ICIs are associated with good clinical efficacy rates, high discontinuation rates and a moderate side-effect profile. They represent an important tool in the urological armamentarium for treating ED in patients that cannot tolerate or are refractory to oral therapies.
Similar content being viewed by others
Introduction
Erectile dysfunction (ED) is defined as inadequate erectile function to allow penetrative intercourse on a persistent or recurrent basis [1]. The estimated prevalence of ED in men > 40 years of age is almost 50% [2]. Risk factors for ED become more prevalent and include increasing age, smoking, obesity and systemic cardiovascular medical conditions such as hypertension, dyslipidaemia and diabetes mellitus (DM). In addition, with increasing numbers of male patients undergoing pelvic surgery and pelvic radiation, the burden of ED has risen [3].
A variety of therapeutic agents have been developed for the treatment of ED and their mechanism of action is primarily based on an understanding of the physiology of erections (Fig. 1). Combining pharmacotherapeutic agents can have a synergist effect for improving erectile function as these agents target different points in the erection physiological pathway. Phosphodiesterase inhibitors (PDE-5 inhibitors), such as sildenafil, were introduced in the 1990s and represent the first-line treatment option for men with ED refractory to lifestyle modification. PDE-5 inhibitors are non-invasive, generally well tolerated and efficacious in a large proportion of men. However, in the 25–50% of patients who do not respond and for those whom PDE5 inhibitors are contraindicated, alternative therapies such as intracavernosal injections (ICIs), intraurethral and topical preparations of alprostadil, vacuum devices and penile prosthesis may be considered. The aim of this review is to comparatively evaluate intracavernosal injectable therapies for ED and to appraise guidelines that inform clinical practice.
Methods
Overview of literature search
A systematic literature search of electronic databases (Medline, Pubmed) was performed to identify original peer-reviewed articles that investigated injectable management strategies for ED. The search was conducted using the following search algorithm: “erectile dysfunction” and “intracavernosal “or “intracorporal injections” or “injectables” limited to articles published after 1990. Two authors (CD and GO) independently examined the title and abstract of citations and the full texts of potentially eligible trials were obtained; disagreements were resolved by discussion. The reference lists of retrieved papers were further screened for additional eligible publications. If a patient group was reported twice, the most recent paper was chosen. If data were unclear or incomplete, the corresponding author was contacted to clarify data extraction. Institutional review board was not sought as this study was a narrative review. Case reports were excluded, and the latest literature search was performed on the 1st of August 2018.
Eligibility criteria
Studies with human data on injectable agents were included. Inclusion criteria were studies in English with outcome data on injectable agents for ED. Primary outcome measures were to comparatively evaluate clinical efficacy, continuation rates and adverse event profiles of each injectable agent as monotherapy or in combination. The secondary outcome measurement was to discuss available guidelines that inform clinical practice for injectable agents.
Eligible studies
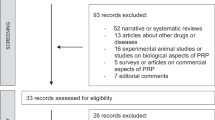
The initial search identified 415 articles and 82 full-text studies were assessed for eligibility; 33 of which were included. Studies were excluded as they did not contain outcome data assessing intracavernosal treatment. This search strategy is summarised in Fig. 1. All included studies were reflective of modern clinical practice and included data on clinical efficacy, continuation rates and adverse event profiles.
Results
Intracavernosal injectable therapy is not reliant on an intact nerve supply. Consequently, if there is adequate blood supply to the penis an improvement erectile function should occur. Outcome measures to assess the response to intracavernosal therapy include subjective patient satisfaction measurements and objective validated scoring systems [e.g. International Index of Erectile Function (IIEF) Questionnaire]. Overall, intracavernosal injections demonstrate clinical efficacy in 54–100% of patients [1]. Published data on outcomes are heterogenous and limited by small sample sizes and a dearth of recent comparative randomised controlled trials. Figure 2 demonstrates the mechanism of action of commonly used agents in intracavernosal therapy is demonstrated by identification of their major physiological target in the erection pathway.
Targets for erectile dysfunction therapies in the penile erection pathway. Modified from Porst H, Burnett A, Brock G, Ghanem H, Giuliano F, Glina S, Hellstrom W, Martin-Morales A, Salonia A, Sharlip I (2013) SOP Conservative (Medical and Mechanical) Treatment of Erectile Dysfunction. Journal of Sexual Medicine 10(1):130–171
Alprostadil
Alprostadil is a synthetic form of prostaglandin-E1 (PGE1). Its mechanism of action is by binding to intracavernosal PGE1 receptors resulting in smooth muscle relaxation and blood flow through cavernosal sinusoids to fill the penile corpora. Side effects are related to the injection site and include penile pain, priapism and penile fibrosis with long-term use.
In 1996, Linet et al. performed a landmark double-blinded randomised controlled trial by comparing the efficacy of alprostadil with a placebo at doses ranging from 2.5 to 20 μg. A dose–response relationship was demonstrated with a minimal effective dose of < 2 μg advised for neurogenic, vasculogenic, psychogenic and multifactorial causes of ED. In a subsequent open label 6-month self-injection trial, clinical efficacy was reported in 94% of patients and defined as ‘patient-reported ability to have sexual activity’. ‘Satisfaction’ with sexual activity occurred in 87% of men and in 86% of partners [4]. More recently, Rabbani et al. demonstrated 76% efficacy with flexible dosing techniques for alprostadil (range 2.5–30 μg, mean 14 μg) with only 50% of patients continuing therapy at 3 months [5]. Furthermore, Khan et al. compared office administration of the agent with ‘self-administration’ at home and noted improved efficacy when the agent was administered under office supervision (50% versus 44.4%, respectively) [6].
Papaverine
Papaverine is a non-selective PDE-5 inhibitor that results in increased intracellular cAMP, decreased intracellular calcium concentrations and subsequent smooth muscle relaxation. Notable adverse effects are penile fibrosis and priapism. Papaverine is frequently described as the original intracavernosal injectable agent as it was first reported by Virag et al. in 1984 and initial efficacy rates of 66% after 12 months were described [7]. Due to increased rates of adverse events such as priapism (6–7%) and penile fibrosis (5.7–11%), papaverine is not approved for monotherapy and is typically injected in combination formulations with phentolamine (i.e. Bimix©) or with phentolamine and alprostadil (i.e. Trimix©) or with atropine (i.e. Quadmix©) [3].
Phentolamine
Phentolamine is a non-selective alpha-adrenergic antagonist that inhibits smooth muscle contraction with a direct dilatory effect on corpus cavernosum smooth muscle and blood vessels. Phentolamine has weak efficacy as single agent and is no longer used as monotherapy; however, it can be used in combination therapy. Chlorpromazine represents an alternative option to phentolamine Trimix© and Bimix© formulations.
Vasoactive intestinal peptide
Aviptadil is a synthetic vasoactive intestinal polypeptide (VIP) that increases the activity of adenosine cyclase, leading to cavernosal smooth muscle relaxation with subsequent filling of cavernosal sinuses and erection. Adverse effects include flushing and headaches. Aviptadil has been combined with phentolamine when monotherapy is ineffective. Aviptadil (25 μg) in combination with 1–2 mg of phentolamine has demonstrated clinical efficacy in 74% compared to 13% with a placebo control [3]. A favourable side-effect profile with this combination was reported, as the incidence of priapism, pain and fibrosis was low at 0.06, 0.5 and 0%, respectively, after 12-month follow-up. Aviptadil/phentolamine combination therapy is also effective in patients that do not respond to other single monotherapy injections with efficacy rates of 67–73% described [8]. Aviptadil/phentolamine combination (Invicorp©) has been clinically approved in Denmark, the United Kingdom and in New Zealand.
Combination therapy
Combination therapies represent an attractive alternative when monotherapy has failed. The common therapeutic combinations are Trimix© which contains alprostadil papaverine and phentolamine or Bimix© which contains the latter two agents. In addition, atropine may be added to a combination of phentolamine, papaverine and alprostadil to form Quadmix© [9].
At present, there is no combination therapy that is globally approved. Therefore, these agents are formulated by compounding pharmacies with sterile laboratory facilities which can lead to variations in constituents and consistencies among such therapies. Inevitably, significant variability results in difficulties in interpreting evidence and may produce inconsistent and unreliable data for patients and prescribers [1]. One large series by Coombs et al. of 1412 patients treated with Trimix© reported a clinical efficacy rate of 89%, defined as erection adequate for penetration up to 24-month follow-up. Efficacy was reduced in patients with diabetes mellitus and with a prior history of pelvic radiation. In this prospective observational study, the discontinuation rate was higher among patients post-radical prostatectomy, as a significant proportion of this cohort recovered erectile function with PDE-5 inhibitors [10]. A smaller series by Aulitzky et al. (n = 67, of whom n = 36 had undergone radical prostatectomy) conducted a retrospective chart review to evaluate combinations of ICI in conjunction with tadalafil, measuring efficacy as achieving adequate erection for penetration. The authors reported efficacy rates of 90% overall and of 95% in the post-radical prostatectomy group [11].
Guidelines on injectable therapy for ED
Many urological bodies have produced guidelines on the management of ED and their salient features are summarised in Table 1. Intracavernosal injections are recommended as a second-line treatment option for patients who have not responded to PDE5 inhibitors in the BSSM, Canadian and EAU guidelines. However, the AUA recommend a less linear approach to treatment and advocate that male patients should be offered information on the administration method, efficacy and adverse effects of all ED therapies prior to selecting a pharmacological agent.
AUA and EAU guidelines advise combination intracavernosal therapy as an alternative to monotherapy due to its more favourable side-effect profile and comparable efficacy rates (92%) [1, 12]. EAU, BSSM and Korean guidelines emphasise important patient issues such as significant discontinuation rates, and the importance of education on administration techniques and on patient follow-up when considering ICIs. Discontinuation rates are typically greatest within 3–6 months of commencement and are usually due to factors such as pain, fibrosis, lack of sexual partner, loss of spontaneity and anxiety [12,13,14]. One comparative study by Wespes et al. demonstrated discontinuation rates of 27.5% with alprostadil compared to 37.6% with combination therapy. When patients continue with ICIs, the attrition rate is approximately 10% despite efficacy rates of 70–85% [12]. Other limiting factors associated with ICI are limited shelf-life availability and the lack of standardisation when preparing combination formulas. Alprostadil loses efficacy within 3 months of cold storage and within 1 week when stored at room temperature.
ICIs are a moderately invasive therapeutic option and require a degree of manual dexterity, from the patient or partner, with education to learn the mechanics of self-injection. All guidelines recommend counselling and education at the outset with a supervised administration consultation to facilitate patient queries, observe administration techniques and to assess response for dose titration if required [1,2,3, 12, 14, 15, 16, 17, 19]. Adverse effects of ICIs are summarised in Table 2. ICIs are also associated with significant anxiety related to the initial injection which occurs in approximately 65% and anxiety levels can remain high for 4 months [15].
It has been well established that ICIs are contraindicated in patients with a known hypersensitivity to the constituents and in patients with a predisposition to priapism (e.g. sickle cell anaemia, multiple myeloma and leukaemia). Anticoagulation medication is not an absolute contraindication; however, patients should be counselled on their increased risk of bleeding and bruising. There are also reports of broken and retained needles with ICIs and evolution into “needle-less” or auto-injection devices may eliminate this complication [18].
Beyond the delivery systems, evolution and change within the treatment of erectile dysfunction are ongoing with new agents and new combinations being tested. Stem cell therapy is being investigated as an alternative to conventional agents though this is still in the early stages [16].
Conclusion
ICIs are associated with good clinical efficacy rates, high discontinuation rates and a significant side-effect profile. They represent an important tool in the urological armamentarium for treating ED in patients that cannot tolerate or are refractory to oral therapies. Their primary role appears to be as a second-line therapy in motivated and well-counselled male patients and for penile rehabilitation in male patients after pelvic surgery. Approval of intracavernosal injection agents is mainly limited to alprostadil with the recent addition of aviptadil/phentolamine combination therapy in a select few geographical regions. Although combination therapies are attractive alternative options in patients with an adverse response to alprostadil alone, their formulations are variable and should be standardised before widespread acceptance can be achieved.
Abbreviations
- AUA:
-
American Urology Association
- BSSM:
-
British Society of Sexual Medicine
- cAMP:
-
Cyclic adenosine monophosphate
- cGMP:
-
Cyclic guanosine monophosphate
- EAU:
-
European Association of Urology
- ED:
-
Erectile dysfunction
- FDA:
-
Food and Drug Authority, USA
- ICI:
-
Intracavernosal injection
- JSSM:
-
Japanese Society of Sexual Medicine
- KSSM:
-
Korean Society of Sexual Medicine
- PDE5:
-
Phosphodiesterase type 5
- PGE1:
-
Prostaglandin 1
- TGA:
-
Therapeutic Goods Administration, Australia
- VIP:
-
Vasoactive intestinal polypeptide
References
Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, Hakim LS et al (2018) Erectile dysfunction: AUA guideline. J Urol 07:07
Bella AJ, Lee JC, Carrier S, Benard F, Brock GB (2015) 2015 CUA Practice guidelines for erectile dysfunction. Can Urol Assoc J 9(1–2):23–29
Hatzimouratidis K, Salonia A, Adaikan G, Buvat J, Carrier S, El-Meliegy A et al (2010) Pharmacotherapy for erectile dysfunction: recommendations from the fourth international consultation for sexual medicine (ICSM 2015). J Sex Med 13(4):465–488
Linet OO, Ogrinc FG, for the Alprostadil Study Group (1996) Efficacy and safety of intracavernosal alprostadil in men with erectile dysfunction. N Engl J Med 334(14):873–877
Rabbani KJ, Tauqeer F, Rabbani R (2010) Prostaglandin E1 for the medical management of erectile dysfunction. Pak J Med Health Sci 4(4):515–519
Khan MM, Khwaja M (2005) Open label study of intracavernous injection of alpostadil alphadex in the treatment of erectile dysfunction. J Postgrad Med Inst 19(1):52–57
Virag RF, Frydman D, Legman M, Virag H (1984) Intracavernous injection of papaverine as a diagnostic and therapeutic method in erectile failure. Angiology 35(2):79–87
Dinsmore WW, Wyllie MG (2008) Vasoactive intestinal polypeptide/phentolamine for intracavernosal injection in erectile dysfunction. BJU Int 102(8):933–937
Sogari PR, Teloken C, Souto CA (1997) Atropine role in the pharmacological erection test: study of 228 patients. J Urol. 158(5):1760–1763
Coombs PG, Heck M, Guhring P, Narus J, Mulhall JP (2012) A review of outcomes of an intracavernosal injection therapy programme. BJU Int 110(11):1787–1791
Aulitzky A, Bazarnik J, Kiper J, Bolyakov A, Paduch D (2012) Safety and efficacy of intracavernosal injection therapy with concomitant daily or as needed tadalafil in men with postprostatectomy and severe erectile dysfunction. J Sex Med 1:54
Wespes E, Amar E, Hatzichristou D, Hatzimouratidis K, Montorsi F, Pryor J et al (2016) EAU guidelines on erectile dysfunction: an update. Eur Urol 49(5):806–815
Hackett G, Kell P, Ralph D, Dean J, Price D, Speakman M et al (2017) British Society for Sexual Medicine guidelines on the management of erectile dysfunction. J Sex Med 5(8):1841–1865
Ryu JK, Cho KS, Kim SJ, Oh KJ, Kam SC, Seo KK et al (2013) Korean Society for Sexual Medicine and Andrology (KSSMA) guideline on erectile dysfunction. World J Mens Health 31(2):83–102
Nelson CJ, Hsiao W, Balk E, Narus J, Tal R, Bennett NE et al (2013) Injection anxiety and pain in men using intracavernosal injection therapy after radical pelvic surgery. J Sex Med 10(10):2559–2565
Andrology Australia (2010) Erectile dysfunction: diagnosis and management. https://www.andrologyaustralia.org/wp-content/uploads/clinical-summary-guide09_May20101.pdf
Capogrosso P, Montorsi F, Salonia A (2018) Phase I and phase II clinical trials for the treatment of male sexual dysfunction—a systematic review of the literature. Expert Opin Investig Drugs 27(7):583–593
O’Kane D, Gibson L, Du Plessis J, Davidson A, Bolton D, Lawrentschuk N (2017) Delivery of intracavernosal therapies using needle-free injection devices. Int J Impot Res 29(6):225–228
Kimoto Y, Nagao K, Sasaki H, Marumo K, Takahashi Y, Nishi S et al (2008) JSSM guidelines for erectile dysfunction. Int J Urol 15(7):564–576
Funding
No funding was provided for this review.
Author information
Authors and Affiliations
Contributions
CD: Project development, data collection, data analysis, manuscript writing & revision. JGO: Project development, data collection, data analysis. JT: data analysis, manuscript writing & revision. NFD: manuscript writing and editing. DMB: Project development, manuscript editing. NL: Project development, data collection, manuscript editing
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest to disclose.
Ethical approval
Ethics approval for this project was not required as no human or animal participants were involved in this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Duncan, C., Omran, G.J., Teh, J. et al. Erectile dysfunction: a global review of intracavernosal injectables. World J Urol 37, 1007–1014 (2019). https://doi.org/10.1007/s00345-019-02727-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02727-5