Abstract
Purpose
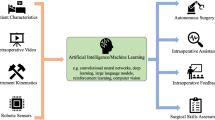
The aim of the current narrative review was to summarize the available evidence in the literature on artificial intelligence (AI) methods that have been applied during robotic surgery.
Methods
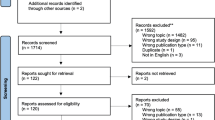
A narrative review of the literature was performed on MEDLINE/Pubmed and Scopus database on the topics of artificial intelligence, autonomous surgery, machine learning, robotic surgery, and surgical navigation, focusing on articles published between January 2015 and June 2019. All available evidences were analyzed and summarized herein after an interactive peer-review process of the panel.
Literature review
The preliminary results of the implementation of AI in clinical setting are encouraging. By providing a readout of the full telemetry and a sophisticated viewing console, robot-assisted surgery can be used to study and refine the application of AI in surgical practice. Machine learning approaches strengthen the feedback regarding surgical skills acquisition, efficiency of the surgical process, surgical guidance and prediction of postoperative outcomes. Tension-sensors on the robotic arms and the integration of augmented reality methods can help enhance the surgical experience and monitor organ movements.
Conclusions
The use of AI in robotic surgery is expected to have a significant impact on future surgical training as well as enhance the surgical experience during a procedure. Both aim to realize precision surgery and thus to increase the quality of the surgical care. Implementation of AI in master–slave robotic surgery may allow for the careful, step-by-step consideration of autonomous robotic surgery.

Similar content being viewed by others
References
Bachman AG, Parker AA, Shaw MD et al (2017) Minimally invasive versus open approach for cystectomy: trends in the utilization and demographic or clinical predictors using the National Cancer Database. Urology 103:99–105
Mazzone E, Mistretta FA, Knipper S et al (2019) Contemporary North-American assessment of robot-assisted surgery rates and total hospital charges for major surgical uro-oncological procedures. J Endourol 33(6):438–447
Autorino R, Porpiglia F, Dasgupta P et al (2017) Precision surgery and genitourinary cancers. Eur J Surg Oncol 43(5):893–908
Veronesi U, Stafyla V, Luini A, Veronesi P (2012) Breast cancer: from “maximum tolerable” to “minimum effective” treatment. Front Oncol 2:125
Gallagher AG (2018) Proficiency-based progression simulation training for more than an interesting educational experience. J Musculoskelet Surg Res 2:139–141
Satava RM, Stefanidis D, Levy JS et al (2019) Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum: a single-blinded, multispecialty, multi-institutional randomized control trial. Ann Surg. https://doi.org/10.1097/SLA.0000000000003220
Wang D, Khosla A, Gargeya R et al (2016) Deep learning for identifying metastatic breast cancer. arXiv preprint arXiv:1606.05718
Bergquist S, Brooks G, Keating N et al (2017) Classifying lung cancer severity with ensemble machine learning in health care claims data. Proc Mach Learn Res 68:25–38
Hashimoto DA, Rosman G, Rus D, Meireles OR (2018) Artificial intelligence in surgery: promises and perils. Ann Surg 268(1):70–76
Shouval R, Hadanny A, Shlomo N et al (2017) Machine learning for prediction of 30-day mortality after ST elevation myocardial infraction: an acute coronary syndrome Israeli survey data mining study. Int J Cardiol 246:7–13
Kassahun Y, Yu B, Tibebu AT et al (2016) Surgical robotics beyond enhanced dexterity instrumentation: a survey of machine learning techniques and their role in intelligent and autonomous surgical actions. Int J Comput Assist Radiol Surg 11(4):553–568
Fard MJ, Ameri S, Darin Ellis R et al (2018) Automated robot-assisted surgical skill evaluation: predictive analytics approach. Int J Med Robot 14(1):e1850
Wang Z, Majewicz Fey A (2018) Deep learning with convolutional neural network for objective skill evaluation in robot-assisted surgery. Int J Comput Assist Radiol Surg 13(12):1959–1970
Ershad M, Rege R, Majewicz Fey A (2019) Automatic and near real-time stylistic behavior assessment in robotic surgery. Int J Comput Assist Radiol Surg 14(4):635–643
Hung AJ, Chen J, Che Z et al (2018) Utilizing machine learning and automated performance metrics to evaluate robot-assisted radical prostatectomy performance and predict outcomes. J Endourol 32(5):438–444
Dai Y, Abiri A, Pensa J et al (2019) Biaxial sensing suture breakage warning system for robotic surgery. Biomed Microdevices 21(1):10
Zhao B, Waterman RS, Urman RD, Gabriel RA (2019) A machine learning approach to predicting case duration for robot-assisted surgery. J Med Syst 43(2):32
Hung AJ, Chen J, Ghodoussipour S et al (2019) A deep-learning model using automated performance metrics and clinical features to predict urinary continence recovery after robot-assisted radical prostatectomy. BJU Int. https://doi.org/10.1111/bju.14735
Collins JW, Dell'Oglio P, Hung AJ, Brook NR (2018) The importance of technical and non-technical skills in robotic surgery training. Eur Urol Focus 4(5):674–676
Lovegrove CE, Elhage O, Khan MS et al (2017) Training modalities in robot-assisted urologic surgery: a systematic review. Eur Urol Focus 3(1):102–116
Mazzone E, Dell’Oglio P, Mottrie A (2019) Outcomes report of the first ERUS robotic urology curriculum-trained surgeon in Turkey: the importance of structured and validated training programs for global outcomes improvement. Turk J Urol 45(3):189–190
Mottrie A, Novara G, van der Poel H et al (2016) The European Association of Urology robotic training curriculum: an update. Eur Urol Focus 2(1):105–108
Larcher A, De Naeyer G, Turri F et al (2019) The ERUS curriculum for robot-assisted partial nephrectomy: structure definition and pilot clinical validation. Eur Urol 75(6):1023–1031
Dell’Oglio P, Turri F, Larcher A et al (2019) Definition of a structured training curriculum for robot-assisted radical cystectomy: a Delphi-consensus study led by the ERUS Educational Board. Eur Urol Suppl 18(1):e1116–e1119
Chen J, Cheng N, Cacciamani G et al (2019) Objective assessment of robotic surgical technical skill: a systematic review. J Urol 201(3):461–469
Schout BMA, Hendrikx AJM, Scheele F, Bemelmans BLH, Scherpbier AJJA (2010) Validation and implementation of surgical simulators: a critical review of present, past, and future. Surg Endosc 24(3):536–546
Goldenberg MG, Lee JY, Kwong JCC, Grantcharov TP, Costello A (2018) Implementing assessments of robot-assisted technical skill in urological education: a systematic review and synthesis of the validity evidence. BJU Int 122(3):501–519
Ganni S, Botden SMBI, Chmarra M, Goossens RHM, Jakimowicz JJ (2018) A software-based tool for video motion tracking in the surgical skills assessment landscape. Surg Endosc 32(6):2994–2999
Hung AJ, Chen J, Gill IS (2018) Automated performance metrics and machine learning algorithms to measure surgeon performance and anticipate clinical outcomes in robotic surgery. JAMA Surg 153(8):770–771
Delto JC, Wayne G, Yanes R, Nieder AM, Bhandari A (2015) Reducing robotic prostatectomy costs by minimizing instrumentation. J Endourol 29(5):556–560
Ramirez D, Ganesan V, Nelson RJ, Haber GP (2016) Reducing costs for robotic radical prostatectomy: three-instrument technique. Urology 95:213–215
Basto M, Sathianathen N, Te Marvelde L et al (2016) Patterns-of-care and health economic analysis of robot-assisted radical prostatectomy in the Australian public health system. BJU Int 117(6):930–939
Pandit JJ, Carey A (2006) Estimating the duration of common elective operations: implications for operating list management. Anaesthesia 61:768–776
Birkmeyer J, Finks J, O'Reilly A et al (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Beulens AJW, Brinkman WM, Van der Poel HG et al (2019) Linking surgical skills to postoperative outcomes: a Delphi study on the robot-assisted radical prostatectomy. J Robot Surg. https://doi.org/10.1007/s11701-018-00916-9
Goldenberg MG, Goldenberg L, Grantcharov TP (2017) Surgeon performance predicts early continence after robot-assisted radical prostatectomy. J Endourol 31(9):858–863
Atug F, Sanli O, Duru AD (2018) Editorial comment on: utilizing machine learning and automated performance metrics to evaluate robot-assisted radical prostatectomy performance and predict outcomes by Hung et al. J Endourol 32(5):445
Chen J, Remulla D, Nguyen JH et al (2019) Current status of artificial intelligence applications in urology and their potential to influence clinical practice. BJU Int. https://doi.org/10.1111/bju.14852
Navaratnam A, Abdul-Muhsin H, Humphreys M (2018) Updates in urologic robot assisted surgery. F1000Res. https://doi.org/10.12688/f1000research.15480.1
Kong SH, Haouchine N, Soares R et al (2017) Robust augmented reality registration method for localization of solid organs’ tumors using CT-derived virtual biomechanical model and fluorescent fiducials. Surg Endosc 31(7):2863–2871
Bertolo R, Hung A, Porpiglia F et al (2019) Systematic review of augmented reality in urological interventions: the evidences of an impact on surgical outcomes are yet to come. World J Urol. https://doi.org/10.1007/s00345-019-02711-z
van Oosterom MN, van der Poel HG, Navab N, van de Velde CJ, van Leeuwen FW (2018) Computer-assisted surgery: virtual-and augmented-reality displays for navigation during urological interventions. Curr Opin Urol 28(2):205–213
Pakhomov D, Premachandran V, Allan M, Azizian M, Navab N (2017) Deep residual learning for instrument segmentation in robotic surgery. arXiv preprint arXiv:1703.08580
Zhao Y, Guo S, Wang Y et al (2019) A CNN-based prototype method of unstructured surgical state perception and navigation for an endovascular surgery robot. Med Biol Eng Comput. https://doi.org/10.1007/s11517-019-02002-0
O’Sullivan S, Nevejans N, Allen C et al (2019) Legal, regulatory, and ethical frameworks for development of standards in artificial intelligence (AI) and autonomous robotic surgery. Int J Med Robot 15(1):e1968
Fichera L, Dillon NP, Zhang D et al (2017) Through the eustachian tube and beyond: new miniature robotic endoscope to see into the middle ear. IEEE Robot Autom Lett 2(3):1488–1494
Yang S, MacLachlan RA, Martel JN, Lobes LA Jr, Riviere CN (2016) Comparative evaluation of handheld robot-aided intraocular laser surgery. IEEE Trans Robot 32(1):246–251
Fornalik H, Fornalik N, Kincy T (2015) Advanced robotics: removal of a 25 cm pelvic mass. J Minim Invasive Gynecol 22(6S):S154
Tsai TY, Dimitriou D, Li JS, Kwon YM (2016) Does haptic robot-assisted total hip arthroplasty better restore native acetabular and femoral anatomy? Int J Med Robot 12(2):288–295
O’Sullivan S, Leonard S, Holzinger A et al (2019) Anatomy 101 for AI-driven robotics: explanatory, ethical and legal frameworks for development of cadaveric *skills training standards in autonomous robotic surgery/autopsy. Int J Med e2020
Chen CH, Suehn T, Illanes A et al (2018) Proximally placed signal acquision sensoric for robotic tissue tool interactions. Curr Dir Biomed Eng 4(1):67–70
Acknowledgements
This research was conducted with the support of the European Urological Scholarship Programme and an NWO TTW VICI grant (TTW BTG 16141).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Protocol/project development: IA, EM, PDO, and AM. Data collection or management: IA, EM, and PDO. Data analysis: IA, EM, and PDO. Manuscript writing: IA, EM, and PDO. Manuscript editing: FWBL, GN, MNO, SB, TB, SOS, PJL, AB, NC, FDH, PS, HDP, and AM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andras, I., Mazzone, E., van Leeuwen, F.W.B. et al. Artificial intelligence and robotics: a combination that is changing the operating room. World J Urol 38, 2359–2366 (2020). https://doi.org/10.1007/s00345-019-03037-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-03037-6