Abstract
Background
Diverting stomata (DS) have been shown to mitigate the clinical impact of anastomotic leakage (AL) but not without complications, and their routine use remains a matter of international debate. The objective of this study was to examine the association between stomata and the clinical consequences of AL.
Methods
This was a nationwide retrospective cohort study including all patients suffering from AL after low anterior resection from 2001 to 2010.
Results
Four thousand sixty-three patients were treated in the period of whom 581 (11.9%) developed AL. In case of AL, patients without a diverting stoma had a slightly higher 90-day mortality rate (13.5% versus 8.7%, p = 0.089). Patients suffered more complications due to AL, both surgical (52% versus 28%, p < 0.001) and non-surgical (48% versus 35%, p = 0.004) with a higher Clavien-Dindo score. Twenty percent of patients developed stoma-related complications prior to stoma reversal. Mortality related to stoma reversal was 2.4%. Factors associated with a risk of a permanent stoma were age (HR 1.04, 95% CI 1.01–1.08), blood transfusion during primary surgery (HR 2.35, 95% CI 1.16–4–78), conserved anastomosis after AL (HR 0.019, 95% CI 0.009–0.04), and a diverting stoma fashioned at the index operation (HR 0.50, 95% CI 0.26–0.97).
Conclusion
The use of diverting stomata during low anterior resection mitigates the clinical impact of AL. However, this benefit needs to be balanced against the risk of stoma-related complications, seen in 20%, and mortality with stoma reversal (2.4%). Where practical, the decision to divert should be made pre-operatively in a multidisciplinary setting.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) accounts for a substantial proportion of the global cancer burden, affecting approximately 1.8 million people and resulting in approximately 900,000 cancer-related deaths each year [1]. Surgery remains the primary treatment modality for the majority of patients with CRC, but despite recent achievements in minimally invasive cancer surgery, morbidity and mortality due to post-operative complications remains an immense challenge. Anastomotic leakage (AL) continues to be one of the most common and feared complications, with an incidence of 5 to 20% after low anterior resection for rectal cancer [2,3,4,5,6,7,8,9]. The consequences of AL can be severe, with subsequent mortality rates ranging from 6 to 22% [2,3,4,5,6,7,8,9]. Other potential sequelae include the need for re-operation, persistent stomas, and an increased risk of locoregional recurrence [10, 11]. Several risk factors for AL have been previously identified and include male gender, a low anastomosis, age, comorbidity, and peri-operative bleeding [12, 13].
The present study addresses the use of a diverting stoma in connection with low anterior resection in rectal cancer treatment. A diverting stoma may be constructed during the primary operation in order to protect the healing anastomosis, with the most common choices being a loop ileostomy or loop transverse colostomy. The use of a diverting stoma has been shown to mitigate the clinical impact, and in some studies also the incidence, of AL [14]. However, the use of diverting stoma is not without complications and their routine use remains a matter of international debate. Although initially intended as a temporary measure, such stomata are never reversed in up to 20% of patients [15]. In addition, diverting ileostomies may be complicated by high output and subsequent renal failure, whereas transverse colostomies tend to prolapse and lead to local cutaneous complications. In addition, stoma reversal has its own range of complications, with reported mortality rates as high as 3% [16].
The aim of the present study was to examine the associations between diverting stomata and the clinical consequences of AL, using the Danish colorectal cancer database.
Methods
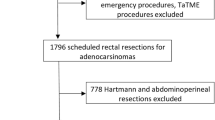
This was a nationwide cohort study including all patients suffering from AL after low anterior resection from 2001 to 2010. The data was extracted from the Danish Colorectal Cancer Group database, which contains data from 98.8% of all CRC operations performed in Denmark from 2001 to 2010. All patients included in the study were recorded in the DCCG database between May 2001 and December 2010 with a primary diagnosis of rectal adenocarcinoma. All patient files were collected and reviewed by one observer (NS). A database collecting relevant information was established, including demography; primary surgery; post-operative care; methods of diagnosis of AL; treatment of AL; data regarding stoma and reversal, short-term, and long-term complications; cancer-specific mortality; and all-cause mortality. For the present study, data related to the subject of interest were extracted from the database and analyzed. The study was approved by the Danish Data Protection Agency.
The primary outcome of the present study was a 90-day mortality; the secondary outcomes were all-cause mortality, morbidity associated with AL, length of stay, complications related to stoma, and risk of permanent stoma.
Statistics
Survival analyses were performed using the Kaplan-Meier method. T test and chi-square were used to test null hypothesis. The results of the multivariable analyses are presented as hazard ratios (HR) with 95% confidence intervals (CI). All analyses were 2-sided and considered statistically significant if p < 0.05. Data were analyzed with SPSS Statistics version 22.0 (IBM Corp, Armonk, NY).
Results
In the 9-year period, a total of 4063 patients were operated for primary rectal cancer with the formation of an anastomosis. Five hundred eighty-one patients developed an AL (11.9%), although a total of 101 patients were lost to subsequent follow-up. As such, 480 patients were included in our analyses. The median follow-up of patients at the time of analysis was 3 years (range 2 days to 12.5 years). Patients were stratified into 2 groups, those with a diverting stoma (DS group) and those without (non-DS group). The non-DS group comprised 228 patients (47.5%). The DS group comprised 252 patients (52.5%). The overwhelming majority of patients in the DS group received a loop ileostomy (98%), with only 2% of patients receiving a diverting colostomy. Patient characteristics and surgical data are shown in Tables 1 and 2.
Patients in the non-DS group became symptomatic following AL at an earlier post-operative time point and, as such, were diagnosed significantly earlier when compared with the DS group. The median post-operative day of was day 6 in the non-diverted group compared with day 9 in patients with a diverting stoma (p < 0.001). The methods of diagnosis also differed between the two patient groups. While radiological assessment (CT scan, contrast enema, and X-ray) was predominant in the non-DS group, digital rectal exam and endoscopy were more likely to be used in the DS group (Table 3).
Significant differences in the treatment of AL were also noted between these patient groups. While more than half (133 patients, 53%) were managed non-surgically in the DS group, only 14 patients (6%) of patients in the non-DS group were managed in this fashion. Concordantly, the number of patients undergoing a Hartmann procedure was significantly higher in the non-DS group compared with those patients with the DS group (128 patients versus 60 patients, p < 0.001).
Mortality associated with AL
A total of 53 patients died within the first 90 days post-operatively, giving a 90-day mortality rate of 11.4%. The 90-day mortality rate was slightly higher in the non-DS group compared with the DS group, although this was not statistically significant (31 (13.5%) versus 22 (8.7%) patients, p = 0.085). Not surprisingly, multiorgan failure and sepsis represented the predominant etiology in early mortality in both patient groups, accounting for 12 (55%) deaths in the DS group and 26 (84%) deaths in the non-DS group. Other reasons for early mortality included pulmonary disease, heart disease, and a single case of cerebral infarction.
At the time of analysis, 133 (45%) patients in the non-DS group and 162 (55%) patients in the DS group were still alive (Fig. 1). Recurrent cancer was the most common cause of delayed mortality and was not found to differ significantly between the 2 groups (27 (11.8%) patients in the non-diverted group, 37 (14.7%) in the diverted group). All causes of death are outlined in Table 4.
Independent prognostic factors associated with a risk of 90-days mortality were investigated using multivariable Cox regression. Interestingly, the association between diverting stoma and 90-mortality was weak, while age (hazard ratio (HR) 1.07, 95% confidence interval (CI) 1.03–1.11), pre-operative morbidity (ASA) (HR 2.46, 95% CI 1.16–5.20), peri-operative complication as expressed by the need of blood transfusion (HR 3.52, 95% CI 1.56–7.97), and late-occurring leakage (HR 0.16, 95% CI 0.04–0.71) seemed to be strongly associated to the risk of 90-day mortality (Table 5).
Morbidity associated with AL
Patients in the non-DS group suffered more complications due to AL than patients in the DS group. This was true to both surgical (120 (53%) patients in the non-DS group versus 71 (28%) in the DS group, p < 0.001) and non-surgical complication (110 (48%) patients in the non-DS group versus 89 (35%) in the DS group, p = 0.004). Acute infections and wound dehiscence complications were abundant in the non-DS group along with complications related to single or multiorgan failures (respiratory 16%, renal 16%, and circulatory 29%). In contrast, post-operative fistulas (rectovaginal, rectoenteric, rectocutaneous) were more common in the DS group (8% versus 5%). The severity of complications, as measured by the Clavien-Dindo score, was significantly higher in the non-DS group (p < 0.001) (Table 6).
Length of stay
Difference in length of stay between the 2 groups was not statistically significant with a median stay of 27 days (range 1–266) in the non-DS group, compared with 22 (range 4–182) in the DS group. When looking at the subgroup that was discharged alive, the result was almost identical (Table 4).
Complications related to stoma and risk of permanent stoma
The complications related to a primary diverting stoma and a secondary stoma fashioned after the occurrence of an anastomotic leakage were similar, except for a higher incidence of high stoma output in patients with primary diversion (5% in the DS group versus 2 % in the non-DS group). Twenty percent of patients developed a stoma-related complication prior to stoma reversal. Apart from high output, these included parastomal hernias (10%), leakage from the stoma (2.7%), and stoma prolapse (2.5%). A total of 5% of patients underwent surgery for stoma-related complications during follow-up. Stoma reversal was performed in 212 patients, of whom 5 died during the operation (3 from the non-DS group, 2 from the DS group), giving a stoma reversal–related mortality rate of 2.4%.
Independent prognostic factors associated with a risk of a permanent stoma were investigated using multivariable Cox regression. Covariates found to be independently prognostic included age (hazard ratio (HR) 1.04, 95% confidence interval (CI) 1.01–1.08), blood transfusion during primary surgery (HR 2.35, 95% CI 1.16–4.78), an intact anastomosis after LA (HR 0.019, 95% CI 0.009–0.04), and primary diversion at the time of initial surgery (HR 0.50, 95% CI 0.26–0.97) (Table 7).
Discussion
In this nationwide study of the importance of a primary diverting stoma in rectal cancer surgery, we found, in accordance with earlier studies, that primary diversion does indeed mitigate the clinical impact of AL. Although not statistically significant, the rates of early mortality in patients with a diverting stoma were a third lower than in those patients without. Patients with a diverting stoma who suffered AL were also found to have a reduced risk of multiorgan failure, as well as lower rates of both surgical and non-surgical complications. In addition, a diverting stoma was associated with an increased likelihood of successful conservative treatment of AL and a decreased risk of a permanent stoma. This study also identified differences not only in the clinical presentation of AL in patients with or without diverting stomata but also in the diagnostic tools typically used to confirm the diagnosis of this complication. The authors acknowledge the limitations of this study, which due to its retrospective nature may be subject to both selection and confounding bias. These limitations do not affect the primary analysis, but certainly, the comparison between the various surgical techniques must be viewed in light of the selection bias.
Although these data make a strong case for the routine use of diverting stomata in surgery for rectal cancer, it should be noted that this study also identified substantial morbidity associated with such stomata, including a mortality rate of almost 3% during stoma reversal. Published rates of reversal-related mortality vary considerably, with reports ranging from 0.06 to 6.4% [17,18,19]. Although the mortality rate in this study is in keeping with published literature, it is recognized that this may be an overestimation of the risk, given that a reversal of a stoma is likely to be more technically challenging in patients who have suffered an AL after their primary surgery than those who have not. In addition to avoiding potential stoma-related morbidity, the omission of a diverting stoma may also reduce the incidence of low anterior resection syndrome (LARS) by facilitating the immediate use of the anal sphincter and avoiding disuse atrophy, resulting in a better functional outcome [20]. One may also make the economic argument for stoma omission, given that it avoids a second admission and second operation. The strongest argument may however be that, given the rate of AL in all-comers in this national cohort was less than 12%, the routine use of diverting stomata would expose almost 9 in every 10 patients to the potential complications of stoma formation and reversal for no clinical benefit.
Diverting stomata are already used selectively in Denmark. Approximately 59% of patients (14% of those undergoing partial mesorectal excision (PME) and 91% of those undergoing total mesorectal excision (TME)) undergoing restorative surgery for cancer within 15 cm from the anal verge are diverted [21]. The decision whether to divert is often made during surgery, based on objective factors such as the patient’s pre-operative performance and peri-operative factors, such as bleeding. However, it is well-recognized that this decision may also be influenced by subjective factors, with the surgeon’s own preferences often based on recent experiences and tradition or culture at their institution [22]. Peri-operatively, there may be a tendency to focus on the risk of AL at the expense of the bigger picture, a situation further compromised by the limited accuracy of the surgeon’s ability to predict AL [23].
The key issue in this complex decision-making process is to identify which patients are at greatest risk of AL and therefore stand to benefit most from a diverting stoma. Several prognostic factors of AL are known pre-operatively, including age, neoadjuvant treatment, male gender, and comorbidities and, to a certain extent, how low the anastomosis is likely to be. These factors could be used to make an evidence-based decision on whether a diverting stoma is indicated pre-operatively, a decision preferably made by a multidisciplinary team (MDT), with the use of a specific decision-making tool [24,25,26]. The use of such a selective strategy has been shown to be both feasible and effective, with a reduction in stoma formation from 90 to 8%, without increasing the rates of re-operation, re-admission, or peri-operative mortality [25]. Once made, this MDT decision should only be overturned by the occurrence of predefined peri-operative factors such as more than a certain amount of bleeding or a lower anastomosis than anticipated. This objective decision-making process should focus the use of diverting stomata to those patients likely to benefit the most.
References
Globocan. (2012). Estimated cancer incidence, mortality and prevalence worldwide in 2012. (2012) Available from: http://globocan.iarc.fr/Default.aspx. Globocan.
Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN, the Norwegian Rectal Cancer Group (2005) Anastomotic leakage following routine meosrectal excision for rectal cancer in a national cohort of patients. Color Dis 7:51–57
Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM, Tang R (2005) Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg 241:9–13
Law WI, Chu KW, Ho JW, Chan CW (2000) Risk factors for anastomotic leakage after low anterior resection with total mesorectalexcision. Am J Surg 179:92–96
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer see comment. Br J Surg 85:355–358
Peeters KC, Tollenaar RA, Marijnen CA et al (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92:211–216
Marusch F, Koch A, Schmidt U, Geiler S, Dralle H, Saeger HD, Wolff S, Nestler G, Pross M, Gastinger I, Lippert H (2002) Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum 45:1164–1171
Hallbook O, Pahlman L, Krog M et al (1996) Randomized comparison of straight and colonic J pouch anastomosis after low anterior resection. Ann Surg 224:58–65
Matthiessen P, Hallbook O, Andersson M, Rutegard J, Sjodahl R (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Color Dis 6:462–469
Branagan G, Finnis D (2005) Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum 48:1021–1026
Merkel S, Wang WY, Schmidt O, Dworak O, Wittekind CH, Hohenberger W, Hermanek P (2001) Locoregional recurrence in patients with anastomotic leakage after anterior resection for rectal carcinoma. Color Dis 3:154–160
Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Kuroyanagi H, Yamaguchi T (2011) Incidence of and risk factors for anastomotic leakage after laparoscopic anterior resection with intracorporeal rectal transection and doublestapling technique anastomosis for rectal cancer. Am J Surg 202:259–226
Law WL, Chu KW (2004) Anterior resection for rectal cancer with mesorectal excision: a prospective evaluation of 622 patients. Ann Surg 240:260–268
Matthiessen P, Hallbook O, Rutegard J et al (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246:207–214
den Dulk M, Smit M, Peeters K, Kranenbarg EM, Rutten HJ, Wiggers T, Putter H, van de Velde C, Dutch Colorectal Cancer Group (2007) A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol 8:297–303
Pokorny H, Herkner H, Jakesz R, Herbst F (2005) Mortality and complications after stoma closure. Arch Surg 140(10):956–960
Mengual-Ballester M, García-Marín JA, Pellicer-Franco E, Guillén-Paredes MP, García-García ML, Cases-Baldó MJ, Aguayo-Albasini JL (2012 Jul) Protective ileostomy: complications and mortality associated with its closure. Rev Esp Enferm Dig 104(7):350–354
Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, Fazio VW (2005) Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum 48(2):243–250
Flikier-Zelkowicz B, Codina-Cazador A, Farrés-Coll R, Olivet-Pujol F, Martín-Grillo A, Pujadas-de PM (2008) Morbidity and mortality associated with diverting ileostomy closures in rectal cancer surgery. Cir Esp 84(1):16–19
Chow A (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Color Dis 24:711–723
DCCG. DCCG Årsrapport 2017. DCCG Årsrapport 2017
Augestad KM, Lindsetmo RO, Stulberg JJ, Reynolds H, Champagne B, Senagore AJ, Delaney CP, (IRCSG)., International Rectal Cancer Study Group (2012 Oct) System-based factors influencing intraoperative decision-making in rectal cancer by surgeons: an international assessment. Color Dis 14(10):679–688
Karliczek A, Harlaar NJ, Zeebregts CJ, Wiggers T, Baas PC, van Dam GM (2009 May) Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Color Dis 24(5):569–576
Multicenter analysis of risk factors for anastomotic leakage after middle and low rectal cancer resection without diverting stoma: a retrospective study . International Journal of Colorectal Disease. 2017;32:1431–1437.
Blok RD, Stam R, Westerduin E, Borstlap WAA, Hompes R, Bemelman WA, Tanis PJ (2018 Aug) Impact of an institutional change from routine to highly selective diversion of a low anastomosis after TME for rectal cancer. Eur J Surg Oncol 44(8):1220–1225
Ihnát P, Guňková P, Peteja M, Vávra P, Pelikán A, Zonča P (2016 Nov) Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc 30(11):4809–4816
Acknowledgments
The authors extend their thanks to Claus Anders Bertelsen, M.D., PhD, for contributing to the conception of the study and acquisition of data.
Author information
Authors and Affiliations
Contributions
Nis Hallundbæk Schlesinger has contributed to the conception of the study and to the acquisition, analysis, and interpretation of the data. He has drafted, revised, and approved the work and is accountable for all aspects of the work.
Henry Smith has contributed to the analysis and interpretation of the data. He has drafted, revised, and approved the work and is accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study has received ethical approval from a local Ethics Committee prior to the study being undertaken. Regional Ethical Committee: De Videnskabsetiske Komiteer for Region, Hovedstaden, Regionsgården, Kongens Vænge 2, 3400 Hillerød.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlesinger, N.H., Smith, H. The effect of a diverting stoma on morbidity and risk of permanent stoma following anastomotic leakage after low anterior resection for rectal cancer: a nationwide cohort study. Int J Colorectal Dis 35, 1903–1910 (2020). https://doi.org/10.1007/s00384-020-03625-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03625-8