Abstract
Purpose
This study aimed to clarify the association of soy intake with cardiovascular disease (CVD) and all-cause mortality.
Methods
We conducted a prospective cohort study in a Chinese population composed of 97,930 participants aged ≥ 40 years old without CVD at baseline in 2011. Habitual soy intake over a period of 12 months was evaluated using a food frequency questionnaire. All participants were classified into four groups based on their soy food consumption levels: < 15, 15–29, 30–59, and ≥ 60 g/day, with the lowest category as the reference group. Follow-up was conducted between 2014 and 2016 to assess CVD incidence and all-cause mortality since baseline, which was collected from the local mortality and disease registers of the National Disease Surveillance Point System and National Health Insurance System. The Cox proportional hazards regression models were used to analyze the relationship of soy intake with later CVD events and all-cause mortality.
Results
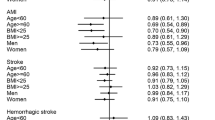
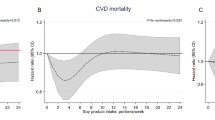
During 350,604 person-years of follow-up (median [interquartile range]: 3.16 [2.98, 4.77] years), 2523 total CVD events and 1473 all-cause mortalities were documented. After controlling for covariates, the hazard ratios (95% confidence intervals) for total CVD events across increasing soy intake levels were 1.03 (0.93–1.14); 0.96 (0.86–1.07); and 0.86 (0.75–0.98; p for trend = 0.0434), while those for all-cause mortality were 0.88 (0.77–1.02); 0.86 (0.74–1.00); and 0.83 (0.69–0.99; p for trend = 0.0084).
Conclusion
High soy intake was associated with a reduced risk of total CVD events and all-cause mortality among a Chinese population.





Similar content being viewed by others
Availability of data and material
Data underlying this article were provided by Ruijin Hospital, Shanghai Jiaotong University. Data are available upon request from the corresponding author, with permission from Ruijin Hospital, Shanghai Jiaotong University.
References
Ramdath DD, Padhi EM, Sarfaraz S, Renwick S, Duncan AM (2017) Beyond the cholesterol-lowering effect of soy protein: a review of the effects of dietary soy and its constituents on risk factors for cardiovascular disease. Nutrients 9:324. https://doi.org/10.3390/nu9040324
Reinwald S, Akabas SR, Weaver CM (2010) Whole versus the piecemeal approach to evaluating soy. J Nutr 140:2335s–2343s. https://doi.org/10.3945/jn.110.124925
Li N, Wu X, Zhuang W, Xia L, Chen Y, Zhao R, Yi M, Wan Q, Du L, Zhou Y (2020) Soy and isoflavone consumption and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomized trials in humans. Mol Nutr Food Res 64:e1900751. https://doi.org/10.1002/mnfr.201900751
Naghavi M, Abajobir AA, Abbafati C et al (2017) Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1151–1210. https://doi.org/10.1016/s0140-6736(17)32152-9
Hay SI, Abajobir AA, Abate KH et al (2017) Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1260–1344. https://doi.org/10.1016/s0140-6736(17)32130-x
Virani SS, Alonso A, Benjamin EJ et al (2020) Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 141:e139–e596. https://doi.org/10.1161/cir.0000000000000757
Gu DF, Weng JP, Lu XF (2020) Chinese guideline on healthy lifestyle to prevent cardiometabolic diseases. Zhonghua yu fang yi xue za zhi [Chinese J Prev Med] 54:256–277. https://doi.org/10.3760/cma.j.issn.0253-9624.2020.03.006
Kokubo Y, Iso H, Ishihara J, Okada K, Inoue M, Tsugane S (2007) Association of dietary intake of soy, beans, and isoflavones with risk of cerebral and myocardial infarctions in Japanese populations: the Japan Public Health Center-based (JPHC) study cohort I. Circulation 116:2553–2562. https://doi.org/10.1161/circulationaha.106.683755
Ma L, Liu G, Ding M, Zong G, Hu FB, Willett W, Rimm EB, Manson JE, Sun Q (2020) Isoflavone intake and the risk of coronary heart disease in US men and women: results from 3 prospective cohort studies. Circulation 141:1127–1137. https://doi.org/10.1161/circulationaha.119.041306
Nagata C, Takatsuka N, Shimizu H (2002) Soy and fish oil intake and mortality in a Japanese community. Am J Epidemiol 156:824–831. https://doi.org/10.1093/aje/kwf118
Katagiri R, Sawada N, Goto A, Yamaji T, Iwasaki M, Noda M, Iso H, Tsugane S (2020) Association of soy and fermented soy product intake with total and cause specific mortality: prospective cohort study. BMJ 368:m34. https://doi.org/10.1136/bmj.m34
Yamasaki K, Kayaba K, Ishikawa S (2015) Soy and soy products intake, all-cause mortality, and cause-specific mortality in Japan: the Jichi Medical School Cohort Study. Asia Pac J Public Health 27:531–541. https://doi.org/10.1177/1010539514539545
Nagata C, Wada K, Tamura T, Konishi K, Goto Y, Koda S, Kawachi T, Tsuji M, Nakamura K (2017) Dietary soy and natto intake and cardiovascular disease mortality in Japanese adults: the Takayama study. Am J Clin Nutr 105:426–431. https://doi.org/10.3945/ajcn.116.137281
Talaei M, Koh WP, van Dam RM, Yuan JM, Pan A (2014) Dietary soy intake is not associated with risk of cardiovascular disease mortality in Singapore Chinese adults. J Nutr 144:921–928. https://doi.org/10.3945/jn.114.190454
Zhang X, Shu XO, Gao YT, Yang G, Li Q, Li H, Jin F, Zheng W (2003) Soy food consumption is associated with lower risk of coronary heart disease in Chinese women. J Nutr 133:2874–2878. https://doi.org/10.1093/jn/133.9.2874
Yu D, Shu XO, Li H et al (2015) Dietary isoflavones, urinary isoflavonoids, and risk of ischemic stroke in women. Am J Clin Nutr 102:680–686. https://doi.org/10.3945/ajcn.115.111591
Yu D, Zhang X, Xiang YB et al (2014) Association of soy food intake with risk and biomarkers of coronary heart disease in Chinese men. Int J Cardiol 172:e285–e287. https://doi.org/10.1016/j.ijcard.2013.12.200
Gobert CP, Duncan AM (2009) Consumption, perceptions and knowledge of soy among adults with type 2 diabetes. J Am Coll Nutr 28:203–218. https://doi.org/10.1080/07315724.2009.10719772
Lu J, He J, Li M et al (2019) Predictive value of fasting glucose, postload glucose, and hemoglobin A(1c) on risk of diabetes and complications in Chinese adults. Diabetes Care 42:1539–1548. https://doi.org/10.2337/dc18-1390
Li M, Xu Y, Wan Q et al (2020) Individual and combined associations of modifiable lifestyle and metabolic health status with new-onset diabetes and major cardiovascular events: the China Cardiometabolic Disease and Cancer Cohort (4C) study. Diabetes Care 43:1929–1936. https://doi.org/10.2337/dc20-0256
Craig CL, Marshall AL, Sjöström M et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395. https://doi.org/10.1249/01.Mss.0000078924.61453.Fb
Lloyd-Jones DM, Hong Y, Labarthe D et al (2010) Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 121:586–613. https://doi.org/10.1161/CIRCULATIONAHA.109.192703
Yang Y (2005) China food composition 2004 book 2, Chinese. Peking University Medical Press, Beijing
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ (2005) Recommendations for blood pressure measurement in humans and experimental animals. Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on high blood pressure research. Circulation 111:697–716. https://doi.org/10.1161/01.Cir.0000154900.76284.F6
Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, Lernmark A, Metzger BE, Nathan DM (2011) Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care 34:e61–e99. https://doi.org/10.2337/dc11-9998
Yan LP, Chan SW, Chan AS, Chen SL, Ma XJ, Xu HX (2006) Puerarin decreases serum total cholesterol and enhances thoracic aorta endothelial nitric oxide synthase expression in diet-induced hypercholesterolemic rats. Life Sci 79:324–330. https://doi.org/10.1016/j.lfs.2006.01.016
Jeon S, Park YJ, Kwon YH (2014) Genistein alleviates the development of nonalcoholic steatohepatitis in ApoE(−/−) mice fed a high-fat diet. Mol Nutr Food Res 58:830–841. https://doi.org/10.1002/mnfr.201300112
Hu X, Gao J, Zhang Q, Fu Y, Li K, Zhu S, Li D (2013) Soy fiber improves weight loss and lipid profile in overweight and obese adults: a randomized controlled trial. Mol Nutr Food Res 57:2147–2154. https://doi.org/10.1002/mnfr.201300159
Mann GE, Rowlands DJ, Li FY, de Winter P, Siow RC (2007) Activation of endothelial nitric oxide synthase by dietary isoflavones: role of NO in Nrf2-mediated antioxidant gene expression. Cardiovasc Res 75:261–274. https://doi.org/10.1016/j.cardiores.2007.04.004
Schreihofer DA, Deutsch C, Lovekamp-Swan T, Sullivan JC, Dorrance AM (2010) Effect of high soy diet on the cerebrovasculature and endothelial nitric oxide synthase in the ovariectomized rat. Vasc Pharmacol 52:236–242. https://doi.org/10.1016/j.vph.2010.02.003
Irace C, Marini H, Bitto A et al (2013) Genistein and endothelial function in postmenopausal women with metabolic syndrome. Eur J Clin Invest 43:1025–1031. https://doi.org/10.1111/eci.12139
Douglas CC, Johnson SA, Arjmandi BH (2013) Soy and its isoflavones: the truth behind the science in breast cancer. Anticancer Agents Med Chem 13:1178–1187. https://doi.org/10.2174/18715206113139990320
Sirotkin AV, Harrath AH (2014) Phytoestrogens and their effects. Eur J Pharmacol 741:230–236. https://doi.org/10.1016/j.ejphar.2014.07.057
Acknowledgements
The authors thank all study participants.
Funding
This research was funded by the Ministry of Science and Technology of the People’s Republic of China (Grant Numbers: 2016YFC0901203, 2016YFC1305600, 2016YFC1305202, 2016YFC1304904, 2017YFC1310700, 2018YFC1311705, and 2018YFC1311800), the Chinese Medical Association Foundation and Chinese Endocrine Society (Grant Number: 12020240314), Chinese Academy of Medical Sciences (Grant No. 2018PT32017, 2019PT330006) Shanghai Medical and Health Development Foundation (Grant No. DMRFP_I_01), Clinical Research Plan of SHDC (Grant No. SHDC2020CR3064B), and Science and Technology Committee of Shanghai (Grant No. 19411964200 and 20Y11905100), the National Key New Drug Creation and Manufacturing Program of the Ministry of Science and Technology (Grant Number: 2012ZX09303006-001), and Startup Fund for Scientific Research of Fujian Medical University (Grant No. 2017XQ1138).
Author information
Authors and Affiliations
Contributions
GN, WW, GC, and JL designed the study; JW, QW, GQ, LY, GW, YQ, ZL, XT, YH, RH, ZY, LS, ZG, QS, YM, JZ, LuC, TZ, XY, QL, FS, LiC, YZ, YW, HD, CL, SW, TY, ML, YX, MX, TW, ZZ, JL, and YB conducted the research; JL and TX analyzed the data; TX wrote the first draft of the manuscript; GC, JW, and JL revised the manuscript; GC assumed primary responsibility for the final content; GN, WW, and JL are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All the authors have read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
All the participants provided consent to publish their data.
Consent to participate
All the participants provided written informed consent.
Ethics approval
The present study was approved by the Medical Ethics Committee of Ruijin Hospital, Shanghai Jiaotong University (approval number: 2011-14).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xue, T., Wen, J., Wan, Q. et al. Association of soy food with cardiovascular outcomes and all-cause mortality in a Chinese population: a nationwide prospective cohort study. Eur J Nutr 61, 1609–1620 (2022). https://doi.org/10.1007/s00394-021-02724-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02724-8