Abstract
Introduction
Knowledge on the learning curve for the repair of Achilles tendon rupture is limited. The aim of this study was to quantify the learning curve for the Krackow suture technique for the repair of Achilles tendon rupture and to identify the correlation between the cumulative volume of cases and clinical outcome measures.
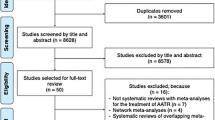
Materials and methods
A total of 226 cases of Achilles tendon repair using the Krackow suture technique were reviewed. Each surgery was independently performed by four surgeons who started a foot and ankle specialty career after fellowship training. After logarithmic transformation of the operative time and cumulative volume of cases, a linear regression analysis was performed to determine the best-fit linear equations to predict the required time for the Krackow suture technique according to the cumulative volume of cases. The correlation between the cumulative volume of cases and clinical outcome measures was analyzed using Pearson correlation coefficients. Receiver operating characteristic curves were constructed to determine the minimum number of cases with an operative time shorter than the average in the first 30 cases.
Results
In all four surgeons, significant log-linear correlations were observed between the operative time and cumulative volume of cases. The best-fit linear equations showed estimated learning rates of 90%, 87%, 92%, and 86% for each of the four surgeons, indicating that the necessary operative time decreased by 10%, 13%, 8%, and 14%, respectively, when the cumulative volume of cases had doubled. The minimum number of cases with an operative time shorter than the average was 9 (91% sensitivity and 59% specificity). The clinical outcome measures at 6 and 12 months postoperatively were available for one surgeon; however, no correlation was found with the cumulative volume of cases.
Conclusion
The learning rate for the Krackow suture technique for the repair of Achilles tendon rupture was approximately 89%, indicating that the required operative time can decrease by up to 11% when the cumulative volume of cases doubles. Therefore, it is important to rapidly accumulate surgical experience during the early phase of training.





Similar content being viewed by others
References
Clayton RA, Court-Brown CM (2008) The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 39:1338–1344. https://doi.org/10.1016/j.injury.2008.06.021
Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U (1993) Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med 21:791–799. https://doi.org/10.1177/036354659302100606
Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M (2005) Treatment of acute Achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Jt Surg Am 87:2202–2210. https://doi.org/10.2106/JBJS.D.03049
Moller M, Movin T, Granhed H, Lind K, Faxen E, Karlsson J (2001) Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Jt Surg Br 83:843–848. https://doi.org/10.1302/0301-620x.83b6.11676
Wenning M, Mauch M, Heitner A, Streicher P, Ritzmann R, Paul J (2021) Midterm functional performance following open surgical repair of acute Achilles tendon rupture. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03746-3
Fischer S, Colcuc C, Gramlich Y, Stein T, Abdulazim A, von Welck S, Hoffmann R (2021) Prospective randomized clinical trial of open operative, minimally invasive and conservative treatments of acute Achilles tendon tear. Arch Orthop Trauma Surg 141:751–760. https://doi.org/10.1007/s00402-020-03461-z
Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB (2015) Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute Achilles tendon ruptures. Foot Ankle Int 36:1279–1286. https://doi.org/10.1177/1071100715589632
Elliot RR, Calder JD (2007) Percutaneous and mini-open repair of acute Achilles tendon rupture. Foot Ankle Clin 12:573–582. https://doi.org/10.1016/j.fcl.2007.07.002
Wei S, Chen J, Kong C, Xu F, Zhi X, Cai X (2021) Endoscopic “internal splinting” repair technique for acute Achilles tendon rupture. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03818-y
Gatz M, Driessen A, Eschweiler J, Tingart M, Migliorini F (2021) Open versus minimally-invasive surgery for Achilles tendon rupture: a meta-analysis study. Arch Orthop Trauma Surg 141:383–401. https://doi.org/10.1007/s00402-020-03437-z
Park SH, Lee HS, Young KW, Seo SG (2020) Treatment of acute Achilles tendon rupture. Clin Orthop Surg 12:1–8. https://doi.org/10.4055/cios.2020.12.1.1
Krackow KA, Thomas SC, Jones LC (1986) A new stitch for ligament-tendon fixation. Brief note. J Bone Jt Surg Am 68:764–766
Hapa O, Erduran M, Havitcioglu H, Cecen B, Aksahin E, Guler S, Atalay K (2013) Strength of different Krackow stitch configurations using high-strength suture. J Foot Ankle Surg 52:448–450. https://doi.org/10.1053/j.jfas.2013.03.009
Watson TW, Jurist KA, Yang KH, Shen KL (1995) The strength of Achilles tendon repair: an in vitro study of the biomechanical behavior in human cadaver tendons. Foot Ankle Int 16:191–195. https://doi.org/10.1177/107110079501600404
Tian J, Rui Y, Xu Y, Yang W, Xu T, Chen X, Zhang X (2020) A biomechanical comparison of Achilles tendon suture repair techniques: locking block modified Krackow, Kessler, and percutaneous Achilles repair system with the early rehabilitation program in vitro bovine model. Arch Orthop Trauma Surg 140:1775–1782. https://doi.org/10.1007/s00402-020-03535-y
Rosenzweig S, Azar FM (2009) Open repair of acute Achilles tendon ruptures. Foot Ankle Clin 14:699–709. https://doi.org/10.1016/j.fcl.2009.07.002
Park YH, Jeong SM, Choi GW, Kim HJ (2017) How early must an acute Achilles tendon rupture be repaired? Injury 48:776–780. https://doi.org/10.1016/j.injury.2017.01.020
Yamakado K (2015) Quantification of the learning curve for arthroscopic suprascapular nerve decompression: an evaluation of 300 cases. Arthroscopy 31:191–196. https://doi.org/10.1016/j.arthro.2014.08.029
Yamakado K (2018) Quantification of the learning curve for arthroscopic Os trigonum excision. J Foot Ankle Surg 57:505–508. https://doi.org/10.1053/j.jfas.2017.11.010
Wright TP (1936) Factors affecting the cost of airplanes. J Aeronaut Sci 3:122–128
Nilsson-Helander K, Thomee R, Silbernagel KG, Thomee P, Faxen E, Eriksson BI, Karlsson J (2007) The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med 35:421–426. https://doi.org/10.1177/0363546506294856
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11):S240-252. https://doi.org/10.1002/acr.20543
Jain NP, Jowett AJ, Clarke NM (2007) Learning curves in orthopaedic surgery: a case for super-specialisation? Ann R Coll Surg Engl 89:143–146. https://doi.org/10.1308/003588407X155798
You JS, Flores SE, Friedman JM, Lansdown DA, Zhang AL (2020) The learning curve for hip arthroscopic surgery: a prospective evaluation with 2-year outcomes in patients with femoroacetabular impingement. Orthop J Sports Med 8:2325967120959140. https://doi.org/10.1177/2325967120959140
Gofton WT, Solomon M, Gofton T, Page A, Kim PR, Netting C, Bhandari M, Beaule PE (2016) What do reported learning curves mean for orthopaedic surgeons? Instr Course Lect 65:633–643
Yelle LE (1979) The learning curve: historical review and comprehensive survey. Decis Sci 10:302–328
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the contents of this study.
Author information
Authors and Affiliations
Contributions
YHP: lead investigator and first author, performing study intervention, writing manuscript. WK: performing study intervention and data analysis. KSJ: performing study intervention and data analysis. THL: performing study intervention and data analysis. EDY: outcome assessment and data analysis. GWC: outcome assessment and manuscript review. HJK: corresponding author and study coordinator, manuscript review.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the local Ethics Committee (IRB No. 2021GR0048, 2021AS0021, and BOHUN202101036). This study was approved by the institutional review boards of three facilities.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, Y.H., Kim, W., Jang, K.S. et al. Learning curve of the Krackow suture technique for the repair of Achilles tendon rupture. Arch Orthop Trauma Surg 142, 3747–3754 (2022). https://doi.org/10.1007/s00402-021-04213-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04213-3