Abstract
Purpose
Several investigations have shown that the risk of childhood overweight and obesity may be associated with excessive gestational weight gain (GWG), but the study samples were limited and results were mixed; hence we conducted this meta-analysis to assess the explicit association between them and present evidence.
Methods
We searched PubMed, EMbase, Ovid, Web of knowledge and Cochrane library for relevant studies. Bibliographies from retrieved articles were also manually searched. Cohort studies that presented results by OR or RR with 95 % CI for the association of maternal excessive GWG and child overweight/obesity were included. The pooled estimates were calculated by fixed-effect model or random-effect model according to the heterogeneity.
Results
Twelve cohort studies were identified, and the combined OR of excessive GWG and childhood overweight/obesity was 1.33 (95 % CI 1.18–1.50) with evidence of heterogeneity (P = 0.000, I 2 = 71.1 %). Adjustment of maternal BMI, investigation area, age of children, research type, and omission of any single study had little effect on the pooled estimate. After eliminating the effect of publication bias by trim and fill analyses, the result still remained statistically significant (OR 1.21, 95 % CI 1.05–1.40).
Conclusions
This meta-analysis suggests that the risk of childhood overweight/obesity is significantly associated with excessive gestational weight gain.
Similar content being viewed by others
Introduction
Childhood overweight and obesity are among the most serious global health problem [1]. There are 16.9 % of children and adolescents aged 2–19 being obese in US according to the National Health and Nutrition Examination Survey, 2009–2010 [2]. It has been pointed out that obesity may increase the risk of cardiovascular diseases, childhood asthma, and lower extremity fractures [3]. Thus, it is critically important to assess the potential risk factors for childhood obesity and overweight. According to existing literature, several lines of evidence have shown that high maternal pregnancy body mass index (BMI), genes, diets, maternal smoking during pregnancy [4] and sleep duration [5] are correlated to childhood overweight and obesity.
Furthermore, maternal gestational weight gain (GWG) was thought to play a potential role in the development of childhood obesity [6]. A number of cohort studies [7–18] tried to find out the possible association between GWG and childhood obesity/overweight, however, five of them [9, 15–18] presented results of null association, and the others showed a weak positive association. A meta-analysis [19] of seven studies suggested GWG is related to 21–57 % increase in the risk of childhood overweight. However, this study was criticized that two included studies were not cohorts, instead one individual participant data meta-analyses and one cross-sectional study. In addition, there was under-power with limited study subjects, and the confounding factors were not explored through subgroup and sensitive analyses.
To quantify the precise association of excessive GWG and childhood overweight/obesity and explore the influence of confounding factor on the association, we conducted current meta-analysis of 12 cohort studies for the following purposes: (1) to summarize the evidence on excessive GWG and childhood overweight/obesity; (2) to access the risk of childhood overweight/obesity associated with the excessive GWG; (3) to exam the effect of confounding factors on the association through subgroup and sensitive analyses.
Methods
Literature search
A literature search was conducted in the databases of PubMed, EMbase, Web of knowledge, Ovid databases (Journey article) and Cochrane library. All databases were searched from the date of their inception to 31 Nov 2012, with the following terms: “offspring OR childhood OR children OR adolescent OR youth OR teenager”, “overweight OR adiposity OR obesity OR corpulent OR fleshiness”, “weight gain OR weight change OR weight increase OR weight growth” and “pregnancy OR pregnant OR pregnancies OR gestational OR gestation OR gravidity OR child bearing”. The terms were combined using the Boolean operator “AND”. The included journal articles were published only in English using human beings recruited as participants. All eligible articles were retrieved and their bibliographies were also manually checked for potential-related articles. No efforts were made to acquire the unpublished reports and the additional information of the original studies.
Study selection
Study selection was achieved by two steps of screening, the abstracts/titles and reading the full-text. Studies included in this meta-analysis must meet following criteria: (1) cohort study; (2) anthropometric data are available to justify children’s status of overweight or obesity; (3) information of their mother’s total GWG are available; (4) odd ratio (OR) or relative risk (RR) with corresponding confidence interval (CI) for the excessive GWG versus adequate GWG were reported. Exclusion criteria: (1) preterm infants; (2) multiple births such as twins; (3) mothers with severe metabolism or infection disease; (4) studies with intervention such as nutrient fortifying. Any dispute was resolved by discussion and confirmed by the third investigator.
Data extraction and quality assessment
Data were independently extracted by two investigators using a self-made data-collection form in accordance with the inclusion criteria and exclusion criteria. Information was recorded as follows: publication journal, publication year, last name of the first author, study location, characteristics of the subject including gender and age of the children, sample size, sampling method, measurement of exposure and outcome, stratification factor, RR and OR with corresponding 95 % CI from the most fully adjusted and unadjusted for the excessive GWG versus adequate GWG, and fully statistical adjustments for the main confounding factors. Any disagreement was resolved through discussion and confirmed by the third investigator. The study quality was assessed according to the Newcastle-Ottawa Quality Assessment Scale Cohort Studies [20] by two authors individually. Each article was scored judging by three main perspectives: selection of subjects (four stars), comparability of the groups (two stars), and ascertainment of the exposure and outcome (three stars). A star is given for one point mentioned with the full mark of 9. The more stars, the better validity.
Data analysis
Our main analysis was focused on the correlation of excessive GWG and childhood overweight/obesity. According to the US Centers for Disease Control and Prevention, childhood overweight is defined as a BMI at or above the 85th percentile and below the 95th percentile for children of the same age and gender, and childhood obesity is above the 95th percentile BMI for children of the same age and gender [21]. The 2009 Institute of Medicine (IOM) recommendations for GWG of singleton pregnancy were based on the maternal pre-pregnancy BMI [22] (Table 1). Although the standard existed, various definitions of the exposure (GWG) and outcome (childhood overweight/obesity) were used in the studies. As for IOM categories, the excessive GWG means above the IOM and reference means within IOM. The exposure of two studies was evaluated according to dichotomous standard of GWG, so the excessive one referred to the higher GWG, and the lower GWG was used as the reference group. The exposure divided into three groups in other two studies was calculated as IOM recommendation categories. In addition, one study divided the exposure into four parts according to the interquartile range, so we regarded GWG ≥75th percentile as excessive GWG and GWG ≤25th percentile as reference. In this procedure, we tried to use the adequate GWG as reference, unless not achieved, the reference in the original studies was used. If a study gave a range of child age, the median was used to represent the age of the selected sample. OR with corresponding 95 % CIs was used to assess the strength of association between the total excessive GWG and childhood overweight/obesity. Only two studies presented the results with RR, hence we converted it into OR according to a statistical formula [23, 24].
Heterogeneity of OR across studies was evaluated by Q statistic (at significance level of P < 0.1) and I-squared statistic (>50 % as evidence of significant inconsistency)-a better measure of the consistency between studies in a meta-analysis [25]. Either fixed-effects or random effects model [26] with the presence of inconsistency was used to combine the effect sizes.
We restricted the studies to those grouped by the 1990 or 2009 IOM recommendation categories, gained high-score, and presented crude OR to do supplementary meta-analyses separately. Subgroup analyses stratified by geographic area, offspring’s age, adjustment of maternal BMI and research type were conducted to evaluate the potential effects of these stratified factors on the pooled estimate. Besides, we also conducted a sensitivity analysis to evaluate the effect of each study on the combined OR by omitting one study in each turn.
Potential publication bias was evaluated by Begg’s funnel plots [27] and Egger’s regression test [28]. All statistical analyses were performed with Stata 12.0 software (StataCorp, College Station, TX, USA). A two-tailed P value of less than 0.05 was predetermined for statistical significance except for specified conditions, which gave a certain P value for significant level.
Results
Literature search
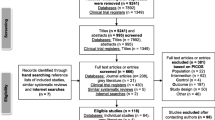
A total of 4,037 potential eligible articles were identified by electronic research with no duplications. The study selection procedure is presented by a flow chart showing in Fig. 1. Of those, 3,905 articles were excluded by title/abstract according to the inclusion and exclusion criteria. The remaining 132 texts were selected and scrutinized, 49 articles with no GWG or child anthropometric data of outcomes and 27 articles without evaluating the association of excessive GWG and childhood overweight/obesity were excluded. Two studies [29, 30] performed a perfectly suitable data were excluded owing to cross-sectional study design. Furthermore, the other two studies [31, 32] were excluded, because they were individual meta-analyses combined several original data of cohort studies. Finally, 12 eligible articles were retained for this meta-analysis.
Totally there are more than 52,000 mother–child pairs analyzed in these 12 observational studies. From seven studies which presented the original data, we calculated that the prevalence of overweight/obesity was 9.6 % in the subjects included in this analysis.
Study characteristics
The characteristics of included studies were presented in Table 2. 12 studies presented 15 results because of different children ages. The studies, consisted of eight prospective studies and four retrospective studies, were published from January 2004 to September 2012. Nine studies of them were conducted in United States, one in Italy, one in Poland, and the other one in UK, respectively. Nine of the included studies were population-based, whereas two studies [13, 16] were only conducted among nurses and one [8] among schoolchildren. Of seven studies, the definition of GWG was above the IOM ranges, and other five had a particular definition showing in the table. The definition of overweight and obesity was determined by BMI for children of the same age and sex except one [10] defined by weight to height ratio. The measurements of GWG were inconsistent between studies with eight studies based on medical record and other four based on self-report by questionnaire or interview. The ages of the children ranged from 2 to 18, which are within our required age (0–18) of the children in the protocol. As for the outcome, original data were presented in seven studies and only effect sizes were presented in the other five ones. The adjustments for potential confounding factors differed across studies, and maternal BMI, maternal age, maternal smoking during pregnancy, maternal education and child birth weight were adjusted in most studies.
In the quality assessment, there are nine studies gained more than five stars, which means high-quality ones; the other two [16, 17] got less than four stars mainly because of the selection of subjects and ascertainment of the exposure and outcome.
Main analysis
The fully adjusted ORs and the pooled OR for excessive GWG versus the reference were presented in Fig. 2. Among 15 results, all but one [17] presented positive associations, furthermore, nine of which were statistically significant. The combined adjusted OR, calculated by random-effect model, was 1.33 (95 % CI 1.18–1.50), with evidence of heterogeneity (P = 0.000, I 2 = 71.1 %). But for the crude OR, fixed-effect model was used and the result was 1.26 (95 % CI 1.19–1.33) with evidence of homogeneity (P = 0.45, I 2 = 0).
Sensitivity and subgroup analyses
When the studies restricted to those using IOM recommendations and high-quality ones, the combined adjusted OR was 1.43 (95 % CI 1.24–1.65) with evidence of heterogeneity (P = 0.05, I 2 = 55.2 %) and 1.50 (95 % CI 1.33–1.69) with evidence of heterogeneity (P = 0.05, I 2 = 45.2 %), respectively. The results of subgroup analyses, stratified by geographic area, offspring age, adjustment of maternal BMI and study design, were presented in Table 3. A significant positive association was observed in all subgroup analysis.
Furthermore, to evaluate the effect of a single study on the combined OR, one study was omitted in each turn and others were used to compute meta-analysis estimates. The combined ORs, all of which had statistical significance with a narrow range of OR from 1.33 (95 % CI 1.17–1.50) to 1.42 (95 % CI 1.21–1.67).
Publication bias
Publication bias was identified by both Begg’s test and Egger’s regression test with an exactly same P value (0.047). Logarithmic ORs of the two poor-quality [16, 17] studies with large samples were beyond the pseudo 95 % confidence limits as Begg’s funnel plots showing in Fig. 3. Due to publication bias existed; we tried to evaluate the effect of publication bias by trim and fill method [33] and the random-effect model. The funnel plots became symmetric after trim and fill as shown in Fig. 4. After eliminating the effect of publication bias, the combined OR was 1.21 (95 % CI 1.05–1.40), which remained consistent with previous results.
Discussion
This current meta-analysis of 12 cohort studies, including eight prospective and four retrospective studies, indicated that excessive GWG was associated with significant increased risk of childhood overweight/obesity, which shares the same idea with the previous meta-analysis [19]. The risk of child overweight/obesity of excessive GWG compared with adequate GWG were 11.4 and 8.8 %, respectively. Furthermore, the associations remained stable both in the sensitive and subgroup analyses.
There are several large scaled studies that share the same results with our meta-analysis. A previous study [32] of evidences for effectiveness of prevention, combined four population-based studies including 34,240 participants, found that the prevention of excessive weight gain (GWG >16) can reduce child overweight by 2.9 % (95 % CI 2.3–3.5 %). Another German study [31], combined the individual data of three German cohort studies, one cohort of which was as same as the one in the former study [32], presented that adjusted OR of excessive GWG according to IOM with children overweight/obesity aged at 5–6, was 1.28 (95 % CI 1.02–1.61) in normal-weight mother. Two cross-sectional studies [29, 30] also confirmed that excessive GWG could increase the risk of childhood overweight/obesity statistically. All the regression models in several included studies [10–12, 16] showed a significant positive association after adjustments for potential confounding factors.
We observed substantial heterogeneity among studies in this meta-analysis, and the heterogeneity still existed after sensitive analyses of quality and subgroup analysis. Therefore, the heterogeneity cannot completely be explained by study qualities, grouped methods of exposure, study location, maternal BMI, childhood age and research design. When the analysis was restricted to studies grouped by IOM recommendation, the evidence of heterogeneity still existed, which obviously demonstrated the grouped factor made little contribution to the heterogeneity. Moreover, dissimilar definitions of GWG, overweight and obesity might also contribute to the heterogeneity. Finally, the heterogeneity could also be caused by the lack of original data and limitation of studies since we only included the published studies and no effort was made to obtain additional information.
Though a substantial heterogeneity existed in subgroup analysis, the results of our subgroup analyses were consistent and robust as the sensitivity analyses, which kept significantly positive after modified by the study area, adjustment of maternal BMI, children age and study design. Maternal BMI, especially pre-pregnancy BMI, plays an important role in the increased risk of childhood overweight and obesity. Hence, the adjustment of maternal BMI can significantly attenuate the influence of excessive GWG on childhood overweight/obesity; this was in correspondence with our subgroup analysis. Since they might share the same susceptible obese gene and lifestyle, obese mother tends to have an obese child [10, 13]. Moreover, maternal obesity could contribute to the child obesity by affecting the intrauterine environment [34]. In another way, birth weight increases with increasing pre-pregnancy BMI [35], and high birth weight subsequently increases the risk of child overweight and obesity [36]. One study [18] presented stratified results by pre-pregnancy BMI categories and suggested a stronger association of excessive GWG and overweight in children among underweight women, which indicated GWG has greater impact in underweight mother. A prospective birth cohort study by Jedrychowski et al. [10] also confirmed that underweight mother tends to possess a stronger association between GWG and childhood overweight/obesity at the age of five. Whereas Beyerlein et al. [31] identified that the greater impact was in normal women, but not underweight ones. Only one included study gave the stratified data, hence no subgroup analysis was done to explore the accurate conclusion. Two studies [10, 16] pointed out that strength of association between excessive GWG and offspring overweight/obesity decreased with child age. As time goes on, the emerging postnatal predictors, including diet, physical activity, are likely to have different influence on weight change between ages. In contrast, the effect of innate predictors might attenuate. These differences could contribute to attenuate the strength of the association. However, no significant reduction of the association was found in our subgroup analysis about child age. It might be explained by limited numbers of included studies, wide age ranges of study subjects and other confounding factors. Take child age as an example, it varies from different individuals, and that the median was used to represent the age of sample. We deemed it could neutralize the effect of different age and becloud the effect of child age on the association. As for sensitive analysis, although the included studies differed from one another in various aspects, the association could be driven by none of the single studies. The combined estimate was strengthened when restricted to either high-quality studies or those grouped by IOM recommendations.
There are several mechanisms by which excessive GWG increases the risk of child overweight or obesity. (1) Child of mother with excessive GWG might share the similar genetic factor and lifestyle habits [10, 16], such as high-calorie food intake and low physical activity. (2) GWG increases birth weight [36, 37] like maternal BMI, which directly associated with child overweight and obesity [34]. The risk of overweight and obesity showed no difference between children of higher and lower birth weight, as lower birth weight is associated with higher risk of central adiposity [38], but the obesity-related morbidity of obese children with low birth weight is much higher than obese children with normal or high birth weight [39]. (3) Someone made a hypothesis that the association between excessive GWG and overweight in offspring relates to neurological weight regulation and the brain-gut interaction [10]. (4) In animal model, exposure to overnutrition in utero increases the expression of adipogenic, lipogenic, and adipokine genes in adipose tissue in early postnatal life and changes the central appetite regulatory network. Mechanism of human being may be as same as that in animal. It is no doubt that many factors are involved in childhood obesity and overweight, and much more potential mechanisms need to be explored.
Our study has several important strengths. First, since individual studies had inadequate statistical power, the meta-analysis of 12 studies involving large amounts of cases and participants enhanced the statistical power and provided a credible estimate with narrowed confidence interval. Second, overweight and obesity were combined into one outcome in our meta-analysis, because the definitions of overweight and obesity are various, overlapped and even took place in included studies. Third, the crude and adjusted effect sizes were compared to distinguish the respective effect of GWG and confounding factors on the outcome. Finally, we have evaluated the influence of publication bias by trim and fill analyses, since the evidence of publication bias was found by both Begg’s test and Egger’s regression test.
Several limitations, however, in this meta-analysis should be considered. First, potential important confounding factors, including maternal BMI, maternal gestational age, maternal smoking during pregnancy, breast-feeding, birth weight, have only been adjusted in part of the included studies. The most important confounding of maternal BMI was not adjusted in two studies [10, 15], and no confounding factors were controlled in one study [14]. But we compared the crude and fully adjusted results, the combined estimates were similar and robust. Second, the various misclassification errors may confuse the results. Excessive GWG was based on 2009 or 1990 IOM recommendations, a certain weight gain or quartile. However, when we restricted to the studies using IOM recommendation categories, the association was still significantly positive. Moreover, in several studies, the measurement of GWG and outcome was based on self-report. Third, both prospective and retrospective studies were selected. Recall bias, interviewer bias, and selection bias are always concerned in retrospective studies. Subgroup analysis by study design suggested that the combined effects had statistical significance with each other (no overlap between 95 % CI), but both of them presented a strong positive effect. Fourth, although substantial heterogeneity across studies existed, the association of excessive GWG and childhood overweight/obesity was stable after sensitive analyses. Finally, publication bias existed in this meta-analysis, but the trim and fill analysis presented an uninfluenced result (1.21 (95 % CI 1.05–1.40), which is still significant and positive.
In conclusion, this meta-analysis provides further evidence that women with excessive GWG have higher risk of overweight or obesity of children under 18 years old. As childhood obesity/overweight has become more concern worldwide and false conception about excessive GWG holds in some underdeveloped areas, more efforts should be made to prevent excessive GWG to alleviate the tough issue about childhood overweight and obesity.
References
Gupta N, Goel K, Shah P, Misra A (2012) Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr Rev 33:48–70
Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief 82:1–8
Kessler J, Koebnick C, Smith N,Adams A (2012) Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res
Matijasevich A, Brion MJ, Menezes AM, Barros AJ, Santos IS et al (2011) Maternal smoking during pregnancy and offspring growth in childhood: 1993 and 2004 Pelotas cohort studies. Arch Dis Child 96:519–525
Meng LP, Liu AL, Hu X, Zhang Q, Du SM et al (2012) Report on childhood obesity in China (10): association of sleep duration with obesity. Biomed Environ Sci 25:133–140
Rodrigues S, Ferris AM, Perez-Escamilla R, Backstrand JR (1998) Obesity among offspring of women with type 1 diabetes. Clin Invest Med 21:258–266
Fraser A, Tilling K, Macdonald-Wallis C, Sattar N, Brion MJ et al (2010) Association of maternal weight gain in pregnancy with offspring obesity and metabolic and vascular traits in childhood. Circulation 121:2557–2564
Fuiano N, Rapa A, Monzani A, Pietrobelli A, Diddi G et al (2008) Prevalence and risk factors for overweight and obesity in a population of Italian schoolchildren: a longitudinal study. J Endocrinol Invest 31:979–984
Gillman MW, Rifas-Shiman SL, Kleinman K, Oken E, Rich-Edwards JW et al (2008) Developmental origins of childhood overweight: potential public health impact. Obesity (Silver Spring) 16:1651–1656
Jedrychowski W, Maugeri U, Kaim I, Budzyn-Mrozek D, Flak E et al (2011) Impact of excessive gestational weight gain in non-smoking mothers on body fatness in infancy and early childhood. Prospective prebirth cohort study in Cracow. J Physiol Pharmacol 62:55–64
Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS (2007) Developmental trajectories of overweight during childhood: role of early life factors. Obesity (Silver Spring) 15:760–771
Margerison Zilko CE, Rehkopf D, Abrams B (2010) Association of maternal gestational weight gain with short- and long-term maternal and child health outcomes. Am J Obstet Gynecol 202(574):e571–e578
Oken E, Rifas-Shiman SL, Field AE, Frazier AL, Gillman MW (2008) Maternal gestational weight gain and offspring weight in adolescence. Obstet Gynecol 112:999–1006
Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW (2007) Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol 196(322):e321–e328
Rooney BL, Mathiason MA, Schauberger CW (2011) Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern Child Health J 15:1166–1175
Stuebe AM, Forman MR, Michels KB (2009) Maternal-recalled gestational weight gain, pre-pregnancy body mass index, and obesity in the daughter. Int J Obes (Lond) 33:743–752
Whitaker RC (2004) Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics 114:e29–e36
Wrotniak BH, Shults J, Butts S, Stettler N (2008) Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. Am J Clin Nutr 87:1818–1824
Nehring I, Lehmann S, von Kries R (2012) Gestational weight gain in accordance to the IOM/NRC criteria and the risk for childhood overweight: a meta-analysis. Pediatr Obes
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 3rd symposium on systematic reviews: beyond the basics, 2000
Barlow SE (2007) Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120(Suppl 4):S164–S192
Weight Gain During Pregnancy (2009) Reexamining the guidelines. National Academy of Sciences, Washington DC
Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA (2011) Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342:d671
Zhang J, Yu KF (1998) What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280:1690–1691
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Moreira P, Padez C, Mourao-Carvalhal I, Rosado V (2007) Maternal weight gain during pregnancy and overweight in Portuguese children. Int J Obes (Lond) 31:608–614
von Kries R, Ensenauer R, Beyerlein A, Amann-Gassner U, Hauner H et al (2010) Gestational weight gain and overweight in children: results from the cross-sectional German KiGGS study. Int J Pediatr Obes
Beyerlein A, Nehring I, Rzehak P, Heinrich J, Muller MJ et al (2012) Gestational weight gain and body mass index in children: results from three german cohort studies. PLoS One 7:e33205
Plachta-Danielzik S, Kehden B, Landsberg B, Schaffrath Rosario A, Kurth BM et al (2012) Attributable risks for childhood overweight: evidence for limited effectiveness of prevention. Pediatrics 130:e865–e871
Taylor S, Tweedie R (1998) Practical estimates of the effect of publication bias in meta-analysis. Australas Epidemiol 5:14–17
Whitaker RC, Dietz WH (1998) Role of the prenatal environment in the development of obesity. J Pediatr 132:768–776
Stamnes Koepp UM, Frost Andersen L, Dahl-Joergensen K, Stigum H, Nass O et al (2012) Maternal pre-pregnant body mass index, maternal weight change and offspring birth-weight. Acta Obstet Gynecol Scand 91:243–249
Oken E, Gillman MW (2003) Fetal origins of obesity. Obes Res 11:496–506
Ludwig DS, Currie J (2010) The association between pregnancy weight gain and birth-weight: a within-family comparison. Lancet 376:984–990
Okosun IS, Liao Y, Rotimi CN, Dever GE, Cooper RS (2000) Impact of birth weight on ethnic variations in subcutaneous and central adiposity in American children aged 5–11 years. A study from the Third National Health and Nutrition Examination Survey. Int J Obes Relat Metab Disord 24:479–484
Adair LS, Cole TJ (2003) Rapid child growth raises blood pressure in adolescent boys who were thin at birth. Hypertension 41:451–456
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 30901189) and China Effective Health Care Network.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tie, HT., Xia, YY., Zeng, YS. et al. Risk of childhood overweight or obesity associated with excessive weight gain during pregnancy: a meta-analysis. Arch Gynecol Obstet 289, 247–257 (2014). https://doi.org/10.1007/s00404-013-3053-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-3053-z