Abstract
Purpose
Preeclampsia is known to be a leading cause of mortality and morbidity among mothers and their infants. Approximately 3–8% of all pregnancies in the US are complicated by preeclampsia and another 5–7% by hypertensive symptoms. However, less is known about its long-term influence on infant neurobehavioral development. The current review attempts to demonstrate new evidence for imprinting gene dysregulation caused by hypertension, which may explain the link between maternal preeclampsia and neurocognitive dysregulation in offspring.
Method
Pub Med and Web of Science databases were searched using the terms “preeclampsia,” “gestational hypertension,” “imprinting genes,” “imprinting dysregulation,” and “epigenetic modification,” in order to review the evidence demonstrating associations between preeclampsia and suboptimal child neurodevelopment, and suggest dysregulation of placental genomic imprinting as a potential underlying mechanism.
Results
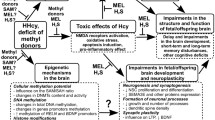
The high mortality and morbidity among mothers and fetuses due to preeclampsia is well known, but there is little research on the long-term biological consequences of preeclampsia and resulting hypoxia on the fetal/child neurodevelopment. In the past decade, accumulating evidence from studies that transcend disciplinary boundaries have begun to show that imprinted genes expressed in the placenta might hold clues for a link between preeclampsia and impaired cognitive neurodevelopment. A sudden onset of maternal hypertension detected by the placenta may result in misguided biological programming of the fetus via changes in the epigenome, resulting in suboptimal infant development.
Conclusion
Furthering our understanding of the molecular and cellular mechanisms through which neurodevelopmental trajectories of the fetus/infant are affected by preeclampsia and hypertension will represent an important first step toward preventing adverse neurodevelopment in infants.
Similar content being viewed by others
References
McCalla CO, Nacharaju VL, Muneyyirci-Delale O, Glasgow S, Feldman JG (1998) Placental 11β-hydroxysteroid dehydrogenase activity in normotensive and pre-eclamptic pregnancies. Steroids 63:511–515
Williams MA, Miller RS, Qiu C, Cripe SM, Gelaye B, Enquobahrie D (2010) Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. Sleep 33:1363–1371
Osterman, MJ, Martin JA, Mathews TJ, Hamilton BE (2011) Expanded data from the new birth certificate, 2008. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 59:1–28
Podymow T, August P (2007) Hypertension in pregnancy. Adv Chronic Kidney Dis 14:178–190
Chang J, Elam-Evans LD, Berg CJ, Herndon J, Flowers L, Seed KA, Syverson CJ (2003) Pregnancy-related mortality surveillance–united states, 1991–1999. Morbidity and mortality weekly report. Surveill Summ 52:1–8
Saadat M, Nejad SM, Habibi G, Sheikhvatan M (2007) Maternal and neonatal outcomes in women with preeclampsia. Taiwan J Obstetr Gynecol 46:255–259
Getahun, D, Rhoads, GG, Demissie, K, Lu, SE, Quinn, VP, Fassett, MJ, Wing, DA, Jacobsen, SJ (2012) In utero exposure to ischemic-hypoxic conditions and attention-deficit/hyperactivity disorder. Pediatrics 131:e53–e61
Mann JR, McDermott S (2010) Are maternal genitourinary infection and pre-eclampsia associated with adhd in school-aged children? J Atten Disord 15:667–673
Silva D, Colvin L, Hagemann E, Bower C (2013) Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics 133:e14–e22
Whitehouse, AJO, Robinson M, Newnham, JP P en nell CE (2012) Do hypertensive diseases of pregnancy disrupt neurocognitive development in offspring? Paediatr Perinat Epidemiol 26:101–108
Nomura Y, Marks DJ, Grossman B, Yoon M, Loudon H, Stone J, Halperin JM (2012) Exposure to gestational diabetes mellitus and low socioeconomic status. Arch Pediatr Adolesc Med 166:337
Ornoy, A, Ratzon, N, Greenbaum, C, Wolf, A, Dulitzky, M (2001) School-age children born to diabetic mothers and to mothers with gestational diabetes exhibit a high rate of inattention and fine and gross motor impairment. J Pediatr Endocrinol Metabol 14:681–690
Bressan FF, De Bem, THC, Perecin F, Lopes FL, Ambrosio CE, Meirelles FV, Miglino MA (2009) Unearthing the roles of imprinted genes in the placenta. Placenta 30:823–834
Davies W, Isles AR, Wilkinson LS (2005) Imprinted gene expression in the brain. Neurosci Biobehav Rev 29:421–430
Roseboom T, de Rooij S, Painter R (2006) The dutch famine and its long-term consequences for adult health. Early Hum Dev 82:485–491
Susser E, Hoek HW, Brown A (1998) Neurodevelopmental disorders after prenatal famine: the story of the dutch famine study. Am J Epidemiol 147:213–216
Rasmussen S, Irgens LM (2003) Fetal growth and body proportion in preeclampsia. Obstet Gynecol 101:575–583
Henriksen T, Clausen T (2002) The fetal origins hypothesis: placental insufficiency and inheritance versus maternal malnutrition in well-nourished populations. Acta Obstet Gynecol Scand 81(2):112–114
Wu G, Imhoff-Kunsch B, Girard AW (2012) Biological mechanisms for nutritional regulation of maternal health and fetal development. Paediatr Perinat Epidemiol 26(Suppl 1):4–26. doi:10.1111/j.1365-3016.2012.01291.x
Bramham K, Briley AL, Seed P, Poston L, Shennan AH, Chappell LC (2011) Adverse maternal and perinatal outcomes in women with previous preeclampsia: A prospective study. Am J Obstet Gynecol 204(512):e1-12.e9
Habli M, Levine RJ, Qian C, Sibai B (2007) Neonatal outcomes in pregnancies with preeclampsia or gestational hypertension and in normotensive pregnancies that delivered at 35, 36, or 37 weeks of gestation. Am J Obstet Gynecol 197(406):e1-06.e7
Jelin AC, Cheng YW, Shaffer BL, Kaimal AJ, Little SE, Caughey AB (2010) Early-onset preeclampsia and neonatal outcomes. J Matern-Fetal Neonat Med 23:389–392
Liggins GC, Howie RN (1972) A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics 50:515–525
Ødegard RA, Vatten LJ, Nilsen ST, Salvesen KÅ, Austgulen R (2000) Preeclampsia and fetal growth. Obstetr Gynecol 96:950–955
Swank, M, Nageotte, M, Hatfield, T (2012) Necrotizing pancreatitis associated with severe preeclampsia. Obstetr Gynecol 120:453–455
Benediktsson R, Lindsay RS, Noble J, Seckl JR, Edwards, CRW (1993) Glucocorticoid exposure in utero: New model for adult hypertension. Lancet 341:339–341
Edwards, CRW, Benediktsson R, Lindsay RS, Seckl JR (1993) Dysfunction of placental glucocorticoid barrier: link between fetal environment and adult hypertension? Lancet 341:355–357
Kalder, M, Ulrich S, Hitschold T, Berle P (1995) [fetal development in mild and severe pre-eclampsia: Correlation with maternal laboratory parameters and doppler ultrasound]. Zeitschrift fur Geburtshilfe und Neonatologie 199:13–17
Liu C-M, Cheng P-J, Chang S-D (2008) Maternal complications and perinatal outcomes associated with gestational hypertension and severe preeclampsia in taiwanese women. Taiwan yi zhi=J Formos Med Assoc 107:129–138
Leuner B, Gould E (2010) Structural plasticity and hippocampal function. Annu Rev Psychol 61:111–140
Jones BP, Bell EA, Maroof M (1999) Epidural labor analgesia in parturient with von willebrandʼs disease type iia and severe preeclampsia. Anesthesiology 90:1219–1220
Masoura S, Kalogiannidis I, Margioula-Siarkou C, Diamanti E, Papouli M, Drossou-Agakidou V, Prapas N, Agorastos T (2012) Neonatal outcomes of late preterm deliveries with pre-eclampsia. Minerva Ginecol 64:109–115
Nomura Y, Lambertini L, Rialdi A, Lee M, Mystal EY, Grabie M, Manaster I, Huynh N, Finik J et al (2013) Global methylation in the placenta and umbilical cord blood from pregnancies with maternal gestational diabetes, preeclampsia, and obesity. Reprod Sci 21:131–137
Bos AF, Einspieler C, Prechtl, HFR (2001) Intrauterine growth retardation, general movements, and neurodevelopmental outcome: a review. Dev Med Child Neurol 43:61
Tolsa CB, Zimine S, Warfield SK, Freschi M, Rossignol AS, Lazeyras F, Hanquinet S, Pfizenmaier M, Hüppi PS (2004) Early alteration of structural and functional brain development in premature infants born with intrauterine growth restriction. Pediatr Res 56:132–138
Arcangeli T, Thilaganathan B, Hooper R, Khan KS, Bhide A (2012) Neurodevelopmental delay in small babies at term: a systematic review. Ultrasound Obstet Gynecol 40(3):267–275. doi:10.1002/uog.11112
Allin M, Matsumoto H, Santhouse AM, Nosarti C, AlAsady MHS, Stewart AL, Rifkin L, Murray RM (2001) Cognitive and motor function and the size of the cerebellum in adolescents born very pre-term. Brain 124:60–66
Marlow N, Wolke D, Bracewell MA, Samara M (2005) Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 352:9–19
Moster D, Lie RT, Markestad T (2008) Long-term medical and social consequences of preterm birth. N Engl J Med 359:262–273
Straub H, Adams M, Kim JJ, Silver RK (2012) Antenatal depressive symptoms increase the likelihood of preterm birth. Am J Obstet Gynecol 207(329):e1-29.e4
Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E (2003) Growth of very low birth weight infants to age 20 years. Pediatrics 112:e30–e38
Mikkola K (2005) Neurodevelopmental outcome at 5 years of age of a national cohort of extremely low birth weight infants who were born in 1996–1997. Pediatrics 116:1391–1400
Sung I-K, Vohr B, Oh W (1993) Growth and neurodevelopmental outcome of very low birth weight infants with intrauterine growth retardation: comparison with control subjects matched by birth weight and gestational age. J Pediatr 123:618–624
Davis EP, Glynn LM, Schetter CD, Hobel C, Chicz-Demet AS, Man CA (2007) Prenatal exposure to maternal depression and cortisol influences infant temperament. J Am Acad Child Adolesc Psychiatry 46:737–746
Huizink AC, Robles de Medina PG, Mulder EJH, Visser GHA, Buitelaar JK (2003) Stress during pregnancy is associated with developmental outcome in infancy. J Child Psychol Psychiat 44:810–818
Marcus S, Lopez JF, McDonough S, MacKenzie MJ, Flynn H, Neal CR, Gahagan S, Volling B, Kaciroti N et al (2011) Depressive symptoms during pregnancy: Impact on neuroendocrine and neonatal outcomes. Infant Behav Dev 34:26–34
Many A, Fattal A, Leitner Y, Kupferminc MJ, Harel S, Jaffa A (2003) Neurodevelopmental and cognitive assessment of children born growth restricted to mothers with and without preeclampsia. Hypertens Pregnancy 22:25–29
Cheng S-W, Chou H-C, Tsou K-I, Fang L-J, Tsao P-N (2004) Delivery before 32 weeks of gestation for maternal pre-eclampsia: neonatal outcome and 2-year developmental outcome. Early Hum Dev 76:39–46
Bayley N (2006) Bayley scales of infant and toddler development, third edition. In: Assessment H. (ed), PsycTESTS Dataset. Psych. Corporation, San Antonio
Posner MI, Rothbart MK, Sheese BE, Voelker P (2014) Developing attention: behavioral and brain mechanisms. Adv Neurosci 2014:1–9
Dougherty LR, Klein DN, Olino TM, Dyson M, Rose S (2009) Increased waking salivary cortisol and depression risk in preschoolers: the role of maternal history of melancholic depression and early child temperament. J Child Psychol Psychiatry 50:1495–1503
Madsen KS, Jernigan TL, Iversen P, Frokjaer VG, Mortensen EL, Knudsen GM, Baaré, WFC (2012) Cortisol awakening response and negative emotionality linked to asymmetry in major limbic fibre bundle architecture. Psychiatry Res: Neuroimaging 201:63–72
Whittle S, Allen NB, Lubman DI, Yücel M (2006) The neurobiological basis of temperament: Towards a better understanding of psychopathology. Neurosci Biobehav Rev 30:511–525
Putnam, SP, Gartstein, MA, Rothbart, MK (2006) Measurement of fine-grained aspects of toddler temperament: the early childhood behavior questionnaire. Infant Behav Dev 29:386–401
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 15(4):264–269
Walker CK, Krakowiak P, Baker A, Hansen RL, Ozonoff S, Hertz-Picciotto I (2015) Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr 169(2):154–162. doi:10.1001/jamapediatrics.2014.2645
Walker CK, Ashwood P, Hertz-Picciotto I (2015) Preeclampsia, placental insufficiency, autism, and antiphospholipid antibodies-reply. JAMA Pediatr 169(6):606–607. doi:10.1001/jamapediatrics.2015.0345
Schroeder DI, Schmidt RJ, Crary-Dooley FK, Walker CK, Ozonoff S, Tancredi DJ, Hertz-Picciotto I, LaSalle JM (2016) Placental methylome analysis from a prospective autism study. Mol Autism 7:51. doi:10.1186/s13229-016-0114-8
Boyle CA, Decoufle P, Yeargin-Allsopp M (1994) Prevalence and health impact of developmental disabilities in us children. Pediatrics 93:399–403
Pastor PN, Reuben CA (2002) Attention deficit disorder and learning disability: United states, 1997–98. Vital and health statistics, series 10, number 206, PsycEXTRA Dataset. American Psychological Association (APA)
Baio J (2012) Prevalence of autism spectrum disorders–autism and developmental disabilities monitoring network, 14 sites, united states, 2008. In: Prevention, C.f.D.C.a. (ed.) Morbidity and mortality weekly report. Surveillance summaries, pp. 1–19
Liu JH (2009) Endocrinology of pregnancy, creasy and resnik’s maternal-fetal medicine: principles and practice. Elsevier BV, pp. 111–124
Petraglia F, Coukos G, Volpe A, Genazzani AR, Vale W (1991) Involvement of placental neurohormones in human parturition. Ann NY Acad Sci 622:331–340
Yen SS (1994) The placenta as the third brain. J Reprod Med 39:277–280
Lambertini L, Lee TL, Chan WY, Lee MJ, Diplas A, Wetmur J, Chen J (2011) Differential methylation of imprinted genes in growth-restricted placentas. Reprod Sci 18:1111–1117
Lambertini L, Lee M-J, Marsit JC, Che J (2012) Genomic imprinting in human placenta. Recent Advances in Research on the Human Placenta. InTech
Reik W (2001) Epigenetic reprogramming in mammalian development. Science 293:1089–1093
Santos F, Dean W (2004) Epigenetic reprogramming during early development in mammals. Reproduction 127:643–651
Perera F, Herbstman J (2011) Prenatal environmental exposures, epigenetics, and disease. Reprod Toxicol 31:363–373
DUJ The genomic imprinting website. Shortitle The genomic imprinting website. http://www.geneimprint.com/site/what-is-imprinting
Garg P, Borel C, Sharp AJ (2012) Detection of parent-of-origin specific expression quantitative trait loci by cis-association analysis of gene expression in trios. PLoS One 7:e41695
Charalambous M, da Rocha ST, Ferguson-Smith AC (2007) Genomic imprinting, growth control and the allocation of nutritional resources: consequences for postnatal life. Curr Opin Endocrinol Diabetes Obes 14:3–12
Shaikh MG (2011) 2.4.1 hypothalamic dysfunction (hypothalamic syndromes), Oxford Textbook of Endocrinology and Diabetes. Oxford University Press (OUP)
John RM (2013) Epigenetic regulation of placental endocrine lineages and complications of pregnancy. Biochm Soc Trans 41:701–709
McMinn J, Wei M, Schupf N, Cusmai J, Johnson EB, Smith AC, Weksberg R, Thaker HM, Tycko B (2006) Unbalanced placental expression of imprinted genes in human intrauterine growth restriction. Placenta 27:540–549
Tycko B, Morison IM (2002) Physiological functions of imprinted genes. J Cell Physiol 192:245–258
Newman, JRS, Ghaemmaghami S, Ihmels J, Breslow DK, Noble M, DeRisi JL, Weissman JS (2006) Single-cell proteomic analysis of s. Cerevisiae reveals the architecture of biological noise. Nature 441:840–846
Zaitoun I, Downs KM, Rosa GJM, Khatib H (2010) Upregulation of imprinted genes in mice: An insight into the intensity of gene expression and the evolution of genomic imprinting. Epigenetics 5:149–158
Elowitz MB (2002) Stochastic gene expression in a single cell. Science 297:1183–1186
Ozbudak EM, Thattai M, Kurtser I, Grossman AD, van Oudenaarden A (2002) Regulation of noise in the expression of a single gene. Nat Genet 31:69–73
Blake WJ, KÆrn M, Cantor CR, Collins JJ (2003) Noise in eukaryotic gene expression. Nature 422:633–637
Fraser HB, Hirsh AE, Giaever G, Kumm J, Eisen MB (2004) Noise minimization in eukaryotic gene expression. PLoS Biol 2:e137
Batada NN, Hurst LD (2007) Evolution of chromosome organization driven by selection for reduced gene expression noise. Nat Genet 39:945–949
Guerrero-Bosagna C, Skinner MK (2012) Environmentally induced epigenetic transgenerational inheritance of phenotype and disease. Mol Cell Endocrinol 354:3–8
Dilinoy DC, Weidman JR, Jirtle RL (2007) Epigenetic gene regulation: linking early developmental environment to adult disease. Reprod Toxicol 23:297–307
Jirtle RL, Skinner MK (2007) Environmental epigenomics and disease susceptibility. Nat Rev Genet 8:253–262
Kappil M, Lambertini L, Chen J (2015) Environmental influences on genomic imprinting. Curr Environ Health Rep 2:155–162
Lambertini L (2014) Genomic imprinting. Curr Opin Pediatr 26:237–242
Lambertini L, Marsit CJ, Sharma P, Maccani M, Ma Y, Hu J, Chen J (2012) Imprinted gene expression in fetal growth and development. Placenta 33:480–486
Chen J, Li Q, Rialdi, Mystal A, EY, Ly, Finik J, Davey J, Lambertini T, Nomura LY (2014) Influences of maternal stress during pregnancy on the epi/genome: comparison of placenta and umbilical cord blood. Depress Anxiety 3:1–6
Diplas AI, Lambertini L, Lee M-J, Sperling R, Lee YL, Wetmur JG, Chen J (2009) Differential expression of imprinted genes in normal and iugr human placentas. Epigenetics 4:235–240
Green BB, Kappil M, Lambertini L, Armstrong DA, Guerin DJ, Sharp AJ, Lester BM, Chen J, Marsit CJ (2015) Expression of imprinted genes in placenta is associated with infant neurobehavioral development. Epigenetics 10:834–841
Lambertini L, Diplas AI, Lee M-J, Sperling R, Chen J, Wetmur JG (2008) A sensitive functional assay reveals frequent loss of genomic imprinting in human placenta. Epigenetics 3:261–269
Lambertini L, Diplas AL, Wetmur J, Lee MJ, Chen J (2009) Evaluation of genomic imprinting employing the analysis of loss of imprinting (loi) at the rna level: preliminary results. Eur J Oncol 14:161–169
Marsit CJ, Lambertini L, Maccani MA, Koestler DC, Houseman EA, Padbury JF, Lester BM, Chen J (2012) Placenta-imprinted gene expression association of infant neurobehavior. J Pediatr 160(854–60):e2
Mathers JC (2007) Early nutrition: Impact on epigenetics, nutrigenomics—opportunities in Asia. S. Karger AG, pp. 42–48
Kawasaki K, Kondoh E, Chigusa Y, Ujita M, Murakami R, Mogami H, Brown JB, Okuno Y, Konishi I (2014) Reliable pre-eclampsia pathways based on multiple independent microarray data sets. Mol Hum Reprod 21:217–224
Enquobahrie DA, Meller M, Rice K, Psaty BM, Siscovick DS, Williams MA (2008) Differential placental gene expression in preeclampsia. Am J Obstet Gynecol 199(566):e1-66.e11
Unek G, Ozmen A, Mendilcioglu I, Simsek M, Korgun ET (2014) The expression of cell cycle related proteins pcna, ki67, p27 and p57 in normal and preeclamptic human placentas. Tissue Cell 46:198–205
Bourque DK, Avila L, Peñaherrera M, von Dadelszen P, Robinson WP (2010) Decreased placental methylation at the h19/igf2 imprinting control region is associated with normotensive intrauterine growth restriction but not preeclampsia. Placenta 31:197–202
Janssen AB, Tunster SJ, Savory N, Holmes A, Beasley J, Parveen, SAR, Penketh, RJA, John RM (2015) Placental expression of imprinted genes varies with sampling site and mode of delivery. Placenta 36:790–795
Romanelli V, Belinchón A, Campos-Barros A, Heath KE, García-Miñaur S, Martínez-Glez V, Palomo R, Mercado G, Gracia R et al (2009) Cdkn1c mutations in hellp/preeclamptic mothers of beckwith–wiedemann syndrome (bws) patients. Placenta 30:551–554
Kanayama N (2002) Deficiency in p57kip2 expression induces preeclampsia-like symptoms in mice. Mol Hum Reprod 8:1129–1135
Knox KS, Baker JC (2007) Genome-wide expression profiling of placentas in the p57kip2 model of pre-eclampsia. Mol Hum Reprod 13:251–263
Takahashi K (2000) P57kip2 regulates the proper development of labyrinthine and spongiotrophoblasts. Mol Hum Reprod 6:1019–1025
Tunster SJ, Van de Pette M, John RM (2011) Fetal overgrowth in the cdkn1c mouse model of beckwith-wiedemann syndrome. Dis Models Mech 4:814–821
Jin F, Qiao C, Luan N, Shang T (2015) The expression of the imprinted gene pleckstrin homology-like domain family a member 2 in placental tissues of preeclampsia and its effects on the proliferation, migration and invasion of trophoblast cells jeg-3. Clin Exp Pharmacol Physiol 42:1142–1151
Weksberg R (2010) Imprinted genes and human disease. Am J Med Genet 154C:317–320
Acknowledgements
This work was supported by the NIMH Grants K01 MH080062, ARRA supplement K01 MH080062S and R01MH102729 (to YN), and MRC Grant MR/MD013960/1 (to AJ).
Author Contributions
Y Nomura: Protocol/project development, Manuscript writing/editing, Study Design; R John: Manuscript writing/editing, Placenta Biology, and Epigenetics; AB Janssen: Manuscript writing/editing, Translational Epigenetics; C Davey: Manuscript writing/editing, Critical Review; J Finik: Manuscript writing/editing, Literature Review, Literature Search; J Buthmann: Manuscript writing/editing, Literature Review, Literature Search; V Glover: Manuscript writing/editing, Critical Review; L Lambertini: Manuscript writing/editing, Translational Epigenetics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest with any author in the study.
Ethical approval
This review article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This article does not contain any studies with human participants that required Informed consents.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nomura, Y., John, R.M., Janssen, A.B. et al. Neurodevelopmental consequences in offspring of mothers with preeclampsia during pregnancy: underlying biological mechanism via imprinting genes. Arch Gynecol Obstet 295, 1319–1329 (2017). https://doi.org/10.1007/s00404-017-4347-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4347-3