Abstract
Purpose
Data on the optimal treatment strategy for patients undergoing neoadjuvant therapy (NAT) who initially presented with metastatic nodes and convert to node-negative disease (cN+ → ycN0) are limited. Since NAT leads to axillary downstaging in 20–60% of patients, the question arises whether these patients might be offered less-invasive procedures than axillary dissection, such as sentinel node biopsy or targeted removal of lymph nodes marked before therapy.
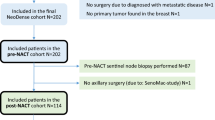
Methods
We performed a systematic review of clinical studies on the use of axillary ultrasound for prediction of response to NAT and ultrasound-guided marking of metastatic nodes for targeted axillary dissection.
Results
The sensitivity of ultrasound for prediction of residual node metastasis was higher than that of clinical examination and MRI/PET in most studies; specificity ranged in large trials from 37 to 92%. The diagnostic performance of ultrasound after NAT seems to be associated with tumor subtype: the positive predictive value was highest in luminal, the negative in triple-negative tumors. Several trials evaluated the usefulness of ultrasound for targeted axillary dissection. Before NAT, nodes were most commonly marked using ultrasound-guided clip placement, followed by ultrasound-guided placement of a radioactive seed. After chemotherapy, the clip was detected on ultrasound in 72–83% of patients; a comparison of sonographic visibility of different clips is lacking. Detection rate after radioactive seed placement was ca. 97%.
Conclusion
In conclusion, ultrasound improves prediction of axillary response to treatment in comparison to physical examination and serves as a reliable guiding tool for marking of target lymph nodes before the start of treatment. High quality and standardization of the examination is crucial for selection of patients for less-invasive surgery.
Similar content being viewed by others
References
de Bellefon M, Lemanski C, Ducteil A, Fenoglietto P, Azria D, Bourgier C (2018) Management of the axilla in the era of breast cancer heterogeneity. Front Oncol 8:84. https://doi.org/10.3389/fonc.2018.00084
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, Ollila DW, Hansen NM, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Morrow M (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318:918–926. https://doi.org/10.1001/jama.2017.11470
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, Cataliotti L, Westenberg AH, Klinkenbijl JH, Orzalesi L, Bouma WH, van der Mijle HC, Nieuwenhuijzen GA, Veltkamp SC, Slaets L, Duez NJ, de Graaf PW, van Dalen T, Marinelli A, Rijna H, Snoj M, Bundred NJ, Merkus JW, Belkacemi Y, Petignat P, Schinagl DA, Coens C, Messina CG, Bogaerts J, Rutgers EJ (2014) Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol 15:1303–1310. https://doi.org/10.1016/S1470-2045(14)70460-7
Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE (2017) Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 35:561–564. https://doi.org/10.1200/JCO.2016.71.0947
AGO Breast Committee (2019) Diagnosis and treatment of patients with primary and metastatic breast cancer. Recommendations 2019. www.ago-online.de. Accessed 1 Oct 2019
(2019) National Comprehensive Cancer Network clinical practice guidelines in oncology: breast cancer, version 3.2019
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, Wolmark N, Rastogi P, Schneeweiss A, Redondo A, Fischer HH, Jacot W, Conlin AK, Arce-Salinas C, Wapnir IL, Jackisch C, DiGiovanna MP, Fasching PA, Crown JP, Wulfing P, Shao Z, Rota Caremoli E, Wu H, Lam LH, Tesarowski D, Smitt M, Douthwaite H, Singel SM, Geyer CE Jr, Investigators K (2019) Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med 380:617–628. https://doi.org/10.1056/NEJMoa1814017
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I, Kuroi K, Im SA, Park BW, Kim SB, Yanagita Y, Ohno S, Takao S, Aogi K, Iwata H, Jeong J, Kim A, Park KH, Sasano H, Ohashi Y, Toi M (2017) Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 376:2147–2159. https://doi.org/10.1056/NEJMoa1612645
Chung A, Giuliano A (2010) Axillary staging in the neoadjuvant setting. Ann Surg Oncol 17:2401–2410. https://doi.org/10.1245/s10434-010-1001-8
Palmer JAV, Flippo-Morton T, Walsh KK, Gusic LH, Sarantou T, Robinson MM, White RL Jr (2018) Application of ACOSOG Z1071: effect of results on patient care and surgical decision-making. Clin Breast Cancer 18:270–275. https://doi.org/10.1016/j.clbc.2017.10.006
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, Lebeau A, Liedtke C, von Minckwitz G, Nekljudova V, Schmatloch S, Schrenk P, Staebler A, Untch M (2013) Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol 14:609–618. https://doi.org/10.1016/S1470-2045(13)70166-9
Boileau JF, Poirier B, Basik M, Holloway CM, Gaboury L, Sideris L, Meterissian S, Arnaout A, Brackstone M, McCready DR, Karp SE, Trop I, Lisbona A, Wright FC, Younan RJ, Provencher L, Patocskai E, Omeroglu A, Robidoux A (2015) Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC study. J Clin Oncol 33:258–264. https://doi.org/10.1200/JCO.2014.55.7827
Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, Leitch AM, Kuerer HM, Bowling M, Flippo-Morton TS, Byrd DR, Ollila DW, Julian TB, McLaughlin SA, McCall L, Symmans WF, Le-Petross HT, Haffty BG, Buchholz TA, Nelson H, Hunt KK, Alliance for Clinical Trials in O (2013) Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA 310:1455–1461. https://doi.org/10.1001/jama.2013.278932
Classe JM, Loaec C, Gimbergues P, Alran S, de Lara CT, Dupre PF, Rouzier R, Faure C, Paillocher N, Chauvet MP, Houvenaeghel G, Gutowski M, De Blay P, Verhaeghe JL, Barranger E, Lefebvre C, Ngo C, Ferron G, Palpacuer C, Campion L (2019) Sentinel lymph node biopsy without axillary lymphadenectomy after neoadjuvant chemotherapy is accurate and safe for selected patients: the GANEA 2 study. Breast Cancer Res Treat 173:343–352. https://doi.org/10.1007/s10549-018-5004-7
Kim HS, Shin MS, Kim CJ, Yoo SH, Yoo TK, Eom YH, Chae BJ, Song BJ (2017) Improved model for predicting axillary response to neoadjuvant chemotherapy in patients with clinically node-positive breast cancer. J Breast Cancer 20:378–385. https://doi.org/10.4048/jbc.2017.20.4.378
Hennessy BT, Hortobagyi GN, Rouzier R, Kuerer H, Sneige N, Buzdar AU, Kau SW, Fornage B, Sahin A, Broglio K, Singletary SE, Valero V (2005) Outcome after pathologic complete eradication of cytologically proven breast cancer axillary node metastases following primary chemotherapy. J Clin Oncol 23:9304–9311. https://doi.org/10.1200/jco.2005.02.5023
Caudle AS, Yang WT, Krishnamurthy S, Mittendorf EA, Black DM, Gilcrease MZ, Bedrosian I, Hobbs BP, DeSnyder SM, Hwang RF, Adrada BE, Shaitelman SF, Chavez-MacGregor M, Smith BD, Candelaria RP, Babiera GV, Dogan BE, Santiago L, Hunt KK, Kuerer HM (2016) Improved axillary evaluation following neoadjuvant therapy for patients with node-positive breast cancer using selective evaluation of clipped nodes: implementation of targeted axillary dissection. J Clin Oncol 34:1072–1078. https://doi.org/10.1200/JCO.2015.64.0094
(2019) National Comprehensive Cancer Network Clinical Practice Guidelines (NCCN Guidelines), breast cancer, Version 1.2019, NCCN.org
Mamtani A, Barrio AV, King TA, Van Zee KJ, Plitas G, Pilewskie M, El-Tamer M, Gemignani ML, Heerdt AS, Sclafani LM, Sacchini V, Cody HS 3rd, Patil S, Morrow M (2016) How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol 23:3467–3474. https://doi.org/10.1245/s10434-016-5246-8
Kim WH, Kim HJ, Park HY, Park JY, Chae YS, Lee SM, Cho SH, Shin KM, Lee SY (2019) Axillary pathologic complete response to neoadjuvant chemotherapy in clinically node-positive breast cancer patients: a predictive model integrating the imaging characteristics of ultrasound restaging with known clinicopathologic characteristics. Ultrasound Med Biol 45:702–709. https://doi.org/10.1016/j.ultrasmedbio.2018.10.026
Di Micco R, Zuber V, Fiacco E, Carriero F, Gattuso MI, Nazzaro L, Panizza P, Gianolli L, Canevari C, Di Muzio N, Pasetti M, Sassi I, Zambetti M, Gentilini OD (2019) Sentinel node biopsy after primary systemic therapy in node positive breast cancer patients: time trend, imaging staging power and nodal downstaging according to molecular subtype. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2019.01.219
You S, Kang DK, Jung YS, An YS, Jeon GS, Kim TH (2015) Evaluation of lymph node status after neoadjuvant chemotherapy in breast cancer patients: comparison of diagnostic performance of ultrasound, MRI and (1)(8)F-FDG PET/CT. Br J Radiol 88:20150143. https://doi.org/10.1259/bjr.20150143
Hieken TJ, Boughey JC, Jones KN, Shah SS, Glazebrook KN (2013) Imaging response and residual metastatic axillary lymph node disease after neoadjuvant chemotherapy for primary breast cancer. Ann Surg Oncol 20:3199–3204. https://doi.org/10.1245/s10434-013-3118-z
Arimappamagan A, Kadambari D, Srinivasan K, Krishnan R, Elangovan S, Reddy KS (2004) Complete axillary conversion after neoadjuvant chemotherapy in locally advanced breast cancer: a step towards conserving axilla? Indian J Cancer 41:13–17
Kuerer HM, Newman LA, Fornage BD, Dhingra K, Hunt KK, Buzdar AU, Ames FC, Ross MI, Feig BW, Hortobagyi GN, Singletary SE (1998) Role of axillary lymph node dissection after tumor downstaging with induction chemotherapy for locally advanced breast cancer. Ann Surg Oncol 5:673–680
Schwentner L, Helms G, Nekljudova V, Ataseven B, Bauerfeind I, Ditsch N, Fehm T, Fleige B, Hauschild M, Heil J, Kummel S, Lebeau A, Schmatloch S, Schrenk P, Staebler A, Loibl S, Untch M, Von Minckwitz G, Liedtke C, Kuhn T (2017) Using ultrasound and palpation for predicting axillary lymph node status following neoadjuvant chemotherapy—results from the multi-center SENTINA trial. Breast 31:202–207. https://doi.org/10.1016/j.breast.2016.11.012
Caudle AS, Kuerer HM, Krishnamurthy S, Shin K, Hobbs BP, Ma J, Mittendorf EA, Washington AC, DeSnyder SM, Black DM, Hunt KK, Yang WT (2019) Feasibility of fine-needle aspiration for assessing responses to chemotherapy in metastatic nodes marked with clips in breast cancer: a prospective registry study. Cancer 125:365–373. https://doi.org/10.1002/cncr.31825
Boughey JC, Ballman KV, Hunt KK, McCall LM, Mittendorf EA, Ahrendt GM, Wilke LG, Le-Petross HT (2015) Axillary ultrasound after neoadjuvant chemotherapy and its impact on sentinel lymph node surgery: results from the American College of Surgeons Oncology Group Z1071 Trial (alliance). J Clin Oncol 33:3386–3393. https://doi.org/10.1200/JCO.2014.57.8401
Vlastos G, Fornage BD, Mirza NQ, Bedi D, Lenert JT, Winchester DJ, Tolley SM, Ames FC, Ross MI, Feig BW, Hunt KK, Buzdar AU, Singletary SE (2000) The correlation of axillary ultrasonography with histologic breast cancer downstaging after induction chemotherapy. Am J Surg 179:446–452
Klauber-Demore N, Kuzmiak C, Rager EL, Ogunrinde OB, Ollila DW, Calvo BF, Kim HJ, Meyer A, Dees C, Graham M 2nd, Collichio FA, Sartor CI, Metzger R, Carey LA (2004) High-resolution axillary ultrasound is a poor prognostic test for determining pathologic lymph node status in patients undergoing neoadjuvant chemotherapy for locally advanced breast cancer. Am J Surg 188:386–389. https://doi.org/10.1016/j.amjsurg.2004.06.022
Rousseau C, Devillers A, Campone M, Campion L, Ferrer L, Sagan C, Ricaud M, Bridji B, Kraeber-Bodere F (2011) FDG PET evaluation of early axillary lymph node response to neoadjuvant chemotherapy in stage II and III breast cancer patients. Eur J Nucl Med Mol Imaging 38:1029–1036. https://doi.org/10.1007/s00259-011-1735-y
Boughey JC, Ballman KV, Le-Petross HT, McCall LM, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, Feliberti EC, Hunt KK (2016) Identification and resection of clipped node decreases the false-negative rate of sentinel lymph node surgery in patients presenting with node-positive breast cancer (T0-T4, N1-N2) who receive neoadjuvant chemotherapy: results From ACOSOG Z1071 (Alliance). Ann Surg 263:802–807. https://doi.org/10.1097/SLA.0000000000001375
Woods RW, Camp MS, Durr NJ, Harvey SC (2018) A review of options for localization of axillary lymph nodes in the treatment of invasive breast cancer. Acad Radiol. https://doi.org/10.1016/j.acra.2018.07.002
Siso C, de Torres J, Esgueva-Colmenarejo A, Espinosa-Bravo M, Rus N, Cordoba O, Rodriguez R, Peg V, Rubio IT (2018) Intraoperative ultrasound-guided excision of axillary clip in patients with node-positive breast cancer treated with neoadjuvant therapy (ILINA Trial): a new tool to guide the excision of the clipped node after neoadjuvant treatment. Ann Surg Oncol 25:784–791. https://doi.org/10.1245/s10434-017-6270-z
Tamai K, Mitsumori M, Fujishiro S, Kokubo M, Ooya N, Nagata Y, Sasai K, Hiraoka M, Inamoto T (2001) A case of allergic reaction to surgical metal clips inserted for postoperative boost irradiation in a patient undergoing breast-conserving therapy. Breast Cancer 8:90–92
Pinkney DM, Mychajlowycz M, Shah BA (2016) A prospective comparative study to evaluate the displacement of four commercially available breast biopsy markers. Br J Radiol 89:20160149. https://doi.org/10.1259/bjr.20160149
Nguyen TT, Hieken TJ, Glazebrook KN, Boughey JC (2017) Localizing the clipped node in patients with node-positive breast cancer treated with neoadjuvant chemotherapy: early learning experience and challenges. Ann Surg Oncol 24:3011–3016. https://doi.org/10.1245/s10434-017-6023-z
Hartmann S, Reimer T, Gerber B, Stubert J, Stengel B, Stachs A (2018) Wire localization of clip-marked axillary lymph nodes in breast cancer patients treated with primary systemic therapy. Eur J Surg Oncol 44:1307–1311. https://doi.org/10.1016/j.ejso.2018.05.035
Plecha D, Bai S, Patterson H, Thompson C, Shenk R (2015) Improving the accuracy of axillary lymph node surgery in breast cancer with ultrasound-guided wire localization of biopsy proven metastatic lymph nodes. Ann Surg Oncol 22:4241–4246. https://doi.org/10.1245/s10434-015-4527-y
Ruland AM, Hagemann F, Reinisch M, Holtschmidt J, Kummel A, Dittmer-Grabowski C, Stoblen F, Rotthaus H, Dreesmann V, Blohmer JU, Kummel S (2018) Using a new marker clip system in breast cancer: tumark vision(R) clip—feasibility testing in everyday clinical practice. Breast care 13:116–120. https://doi.org/10.1159/000486388
Donker M, Straver ME, Wesseling J, Loo CE, Schot M, Drukker CA, van Tinteren H, Sonke GS, Rutgers EJ, Vrancken Peeters MJ (2015) Marking axillary lymph nodes with radioactive iodine seeds for axillary staging after neoadjuvant systemic treatment in breast cancer patients: the MARI procedure. Ann Surg 261:378–382. https://doi.org/10.1097/SLA.0000000000000558
Straver ME, Loo CE, Alderliesten T, Rutgers EJ, Vrancken Peeters MT (2010) Marking the axilla with radioactive iodine seeds (MARI procedure) may reduce the need for axillary dissection after neoadjuvant chemotherapy for breast cancer. Br J Surg 97:1226–1231. https://doi.org/10.1002/bjs.7073
Alderliesten T, Loo CE, Pengel KE, Rutgers EJ, Gilhuijs KG, Vrancken Peeters MJ (2011) Radioactive seed localization of breast lesions: an adequate localization method without seed migration. Breast J 17:594–601. https://doi.org/10.1111/j.1524-4741.2011.01155.x
Donker M, Drukker CA, Valdes Olmos RA, Rutgers EJ, Loo CE, Sonke GS, Wesseling J, Alderliesten T, Vrancken Peeters MJ (2013) Guiding breast-conserving surgery in patients after neoadjuvant systemic therapy for breast cancer: a comparison of radioactive seed localization with the ROLL technique. Ann Surg Oncol 20:2569–2575. https://doi.org/10.1245/s10434-013-2921-x
Hung TJ, Burrage J, Bourke A, Taylor D (2017) Intraoperative localisation of impalpable breast lesions utilising the ROLLIS technique following peritumoral < sup > 99 m </sup > Tc-colloid sentinel node lymphoscintigraphy. Curr Radiopharm 10:111–114. https://doi.org/10.2174/1874471010666170428113052
van Nijnatten TJA, Simons JM, Smidt ML, van der Pol CC, van Diest PJ, Jager A, van Klaveren D, Kam BLR, Lobbes MBI, de Boer M, Verhoef K, Koppert LB, Luiten EJT (2017) A novel less-invasive approach for axillary staging after neoadjuvant chemotherapy in patients with axillary node-positive breast cancer by combining radioactive iodine seed localization in the axilla with the sentinel node procedure (RISAS): a Dutch prospective multicenter validation study. Clin Breast Cancer 17:399–402. https://doi.org/10.1016/j.clbc.2017.04.006
Koolen BB, Donker M, Straver ME, van der Noordaa MEM, Rutgers EJT, Valdes Olmos RA, Vrancken Peeters M (2017) Combined PET-CT and axillary lymph node marking with radioactive iodine seeds (MARI procedure) for tailored axillary treatment in node-positive breast cancer after neoadjuvant therapy. Br J Surg 104:1188–1196. https://doi.org/10.1002/bjs.10555
Choy N, Lipson J, Porter C, Ozawa M, Kieryn A, Pal S, Kao J, Trinh L, Wheeler A, Ikeda D, Jensen K, Allison K, Wapnir I (2015) Initial results with preoperative tattooing of biopsied axillary lymph nodes and correlation to sentinel lymph nodes in breast cancer patients. Ann Surg Oncol 22:377–382. https://doi.org/10.1245/s10434-014-4034-6
Dauphine C, Reicher JJ, Reicher MA, Gondusky C, Khalkhali I, Kim M (2015) A prospective clinical study to evaluate the safety and performance of wireless localization of nonpalpable breast lesions using radiofrequency identification technology. Am J Roentgenol 204:W720–W723. https://doi.org/10.2214/AJR.14.13201
Natsiopoulos I, Intzes S, Liappis T, Zarampoukas K, Zarampoukas T, Zacharopoulou V, Papazisis K (2019) Axillary lymph node tattooing and targeted axillary dissection in breast cancer patients who presented as cN + before neoadjuvant chemotherapy and became cN0 after treatment. Clin Breast Cancer 19:208–215. https://doi.org/10.1016/j.clbc.2019.01.013
Diego EJ, McAuliffe PF, Soran A, McGuire KP, Johnson RR, Bonaventura M, Ahrendt GM (2016) Axillary staging after neoadjuvant chemotherapy for breast cancer: a pilot study combining sentinel lymph node biopsy with radioactive seed localization of pre-treatment positive axillary lymph nodes. Ann Surg Oncol 23:1549–1553. https://doi.org/10.1245/s10434-015-5052-8
Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Giuliano AE, American College of Surgeons Oncology G (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol 25:3657–3663. https://doi.org/10.1200/JCO.2006.07.4062
Choi HJ, Kim I, Alsharif E, Park S, Kim JM, Ryu JM, Nam SJ, Kim SW, Yu J, Lee SK, Lee JE (2018) Use of sentinel lymph node biopsy after neoadjuvant chemotherapy in patients with axillary node-positive breast cancer in diagnosis. J Breast Cancer 21:433–441. https://doi.org/10.4048/jbc.2018.21.e54
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14:500–515. https://doi.org/10.1016/S1470-2045(13)70076-7
Petrelli F, Lonati V, Barni S (2012) Axillary dissection compared to sentinel node biopsy for the treatment of pathologically node-negative breast cancer: a meta-analysis of four randomized trials with long-term follow up. Oncol Rev 6:e20. https://doi.org/10.4081/oncol.2012.e20
Wang Z, Wu LC, Chen JQ (2011) Sentinel lymph node biopsy compared with axillary lymph node dissection in early breast cancer: a meta-analysis. Breast Cancer Res Treat 129:675–689. https://doi.org/10.1007/s10549-011-1665-1
Yen TW, Fan X, Sparapani R, Laud PW, Walker AP, Nattinger AB (2009) A contemporary, population-based study of lymphedema risk factors in older women with breast cancer. Ann Surg Oncol 16:979–988. https://doi.org/10.1245/s10434-009-0347-2
Kuhn T, Classe JM, Gentilini OD, Tinterri C, Peintinger F, de Boniface J (2018) Current status and future perspectives of axillary management in the neoadjuvant setting. Breast care 13:337–341. https://doi.org/10.1159/000492437
Kantor O, Sipsy LM, Yao K, James TA (2018) A predictive model for axillary node pathologic complete response after neoadjuvant chemotherapy for breast cancer. Ann Surg Oncol 25:1304–1311. https://doi.org/10.1245/s10434-018-6345-5
Tadros AB, Yang WT, Krishnamurthy S, Rauch GM, Smith BD, Valero V, Black DM, Lucci A Jr, Caudle AS, DeSnyder SM, Teshome M, Barcenas CH, Miggins M, Adrada BE, Moseley T, Hwang RF, Hunt KK, Kuerer HM (2017) Identification of patients with documented pathologic complete response in the breast after neoadjuvant chemotherapy for omission of axillary surgery. JAMA Surg 152:665–670. https://doi.org/10.1001/jamasurg.2017.0562
Liedtke C, Kolberg HC, Kerschke L, Gorlich D, Bauerfeind I, Fehm T, Fleige B, Helms G, Lebeau A, Stabler A, Schmatloch S, Hausschild M, Schwentner L, von Minckwitz G, Loibl S, Untch M, Kuhn T (2018) Systematic analysis of parameters predicting pathological axillary status (ypN0 vs. ypN +) in patients with breast cancer converting from cN + to ycN0 through primary systemic therapy (PST). Clin Exp Metastasis 35:777–783. https://doi.org/10.1007/s10585-018-9938-2
Caudle AS, Yang WT, Mittendorf EA, Black DM, Hwang R, Hobbs B, Hunt KK, Krishnamurthy S, Kuerer HM (2015) Selective surgical localization of axillary lymph nodes containing metastases in patients with breast cancer: a prospective feasibility trial. JAMA Surg 150:137–143. https://doi.org/10.1001/jamasurg.2014.1086
Funding
Not applicable, no funding received.
Author information
Authors and Affiliations
Contributions
MB-P: project development, data collection, data analysis, manuscript writing. IVG: data analysis, manuscript writing. AH: manuscript editing. PP: data collection, data analysis, manuscript writing. NK: data collection, data analysis, manuscript writing. MM: manuscript editing. SB: manuscript editing. MH: project development, data analysis, manuscript writing
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Not applicable (review article), no human or animal participants involved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Banys-Paluchowski, M., Gruber, I.V., Hartkopf, A. et al. Axillary ultrasound for prediction of response to neoadjuvant therapy in the context of surgical strategies to axillary dissection in primary breast cancer: a systematic review of the current literature. Arch Gynecol Obstet 301, 341–353 (2020). https://doi.org/10.1007/s00404-019-05428-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05428-x