Abstract
Purpose
To assess the effects PCOS on live birth rates when transferring a single fresh ideal blastocyst.
Methods
A retrospective cohort study performed at the university-affiliated reproductive center. Women with PCOS and a control group of normal ovulatory women who underwent their first fresh embryo transfer with single ideal grade blastocyst were included in the study. Demographic, stimulation information and pregnancy outcomes were collected and analysed. The primary outcome was live birth rates, and secondary outcomes included pregnancy and clinical pregnancy rates.
Results
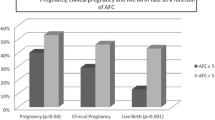
71 Women with PCOS and 272 normal ovulatory controls underwent their first embryo transfer and met the inclusion and exclusion criteria. PCOS patient were younger (31.0 ± 3.7 vs. 33.1 ± 3.2, p = 0.0001), with higher AFC (40.0 ± 9.3 vs. 13.3 ± 4.6, p = 0.0001), required lower dose of gonadotropins to stimulate (1198 ± 786 vs. 1891 ± 1224, p = 0.0001), and had higher serum testosterone levels (2.3 ± 0.7 vs. 1.1 ± 0.3, p = 0.0001). No significant difference was found between the two groups regarding the number of previous pregnancies, the number of previous full-term pregnancies, the level of basal serum FSH, estradiol level at triggering and the BMI. When compared by Chi squared testing pregnancy rates, clinical pregnancy rates and live birth rates did not differ. However, when controlling (with multivariate stepwise logistic regression) for confounders, live birth rates were lower among the women with PCOS (p = 0.035, CI: 0.18−0.92).
Conclusion
After controlling for confounders, when transferring a fresh single ideal blastocyst, live birth rates were lower among the women with PCOS than normal ovulatory controls.
Similar content being viewed by others
References
Norman RJ, Dewailly D, Legro RS, Hickey TE (2007) Polycystic ovary syndrome. Lancet (Lond Engl) 370:685–697. https://doi.org/10.1016/S0140-6736(07)61345-2
ESHRE Capri Workshop Group DT, Balen A, Escobar-Morreale HF, et al (2012) Health and fertility in World Health Organization group 2 anovulatory women. Hum Reprod Update 18:586–99. https://doi.org/10.1093/humupd/dms019
Koivunen R, Pouta A, Franks S et al (2008) Fecundability and spontaneous abortions in women with self-reported oligo-amenorrhea and/or hirsutism: Northern Finland Birth Cohort 1966 Study. Hum Reprod 23:2134–2139. https://doi.org/10.1093/humrep/den136
Tannus S, Burke YZ, Kol S (2015) Treatment Strategies for the Infertile Polycystic Ovary Syndrome Patient. Women’s Heal 11:901–912. https://doi.org/10.2217/whe.15.40
Teede HJ, Misso ML, Costello MF et al (2018) Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome†‡. Hum Reprod 33:1602–1618. https://doi.org/10.1093/humrep/dey256
Legro RS, Arslanian SA, Ehrmann DA et al (2013) Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 98:4565–4592. https://doi.org/10.1210/jc.2013-2350
Heijnen EMEW, Eijkemans MJC, Hughes EG et al (2006) A meta-analysis of outcomes of conventional IVF in women with polycystic ovary syndrome. Hum Reprod Update 12:13–21. https://doi.org/10.1093/humupd/dmi036
Brinsden PR, Wada I, Tan SL et al (1995) Diagnosis, prevention and management of ovarian hyperstimulation syndrome. Br J Obstet Gynaecol 102:767–772
MacDougall MJ, Tan SL, Jacobs HS (1992) In-vitro fertilization and the ovarian hyperstimulation syndrome. Hum Reprod 7:597–600
Kumar P, Nawani N, Malhotra N et al (2013) Assisted reproduction in polycystic ovarian disease: a multicentric trial in India. J Hum Reprod Sci 6:49–53. https://doi.org/10.4103/0974-1208.112382
Qiao J, Feng HL (2011) Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum Reprod Update 17:17–33. https://doi.org/10.1093/humupd/dmq032
Bussen S, Sütterlin M, Steck T (1999) Endocrine abnormalities during the follicular phase in women with recurrent spontaneous abortion. Hum Reprod 14:18–20
Li HWR, Lee VCY, Lau EYL et al (2014) Cumulative live-birth rate in women with polycystic ovary syndrome or isolated polycystic ovaries undergoing in vitro fertilisation treatment. J Assist Reprod Genet 31:205–211. https://doi.org/10.1007/s10815-013-0151-6
Yu H-F, Chen H-S, Rao D-P, Gong J (2016) Association between polycystic ovary syndrome and the risk of pregnancy complications. Medicine (Baltimore) 95:e4863. https://doi.org/10.1097/MD.0000000000004863
Weghofer A, Munne S, Chen S et al (2007) Lack of association between polycystic ovary syndrome and embryonic aneuploidy. Fertil Steril 88:900–905. https://doi.org/10.1016/j.fertnstert.2006.12.018
Ashkenazi J, Farhi J, Orvieto R et al (1995) Polycystic ovary syndrome patients as oocyte donors: the effect of ovarian stimulation protocol on the implantation rate of the recipient. Fertil Steril 64:564–567
Tulppala M, Stenman UH, Cacciatore B, Ylikorkala O (1993) Polycystic ovaries and levels of gonadotrophins and androgens in recurrent miscarriage: prospective study in 50 women. Br J Obstet Gynaecol 100:348–352
Levin D, Jun SH, Dahan MH (2015) Predicting pregnancy in women undergoing in vitro fertilization with basal serum follicle stimulating hormone levels between 10.0 and 11.9 IU/L. J Turk Ger Gynecol Assoc 16:5–10. https://doi.org/10.5152/jtgga.2015.15218
Huang LN, Jun SH, Drubach N, et al (2015) Predictors of in vitro fertilization outcomes in women with highest follicle-stimulating hormone levels ≥ 12 IU/L: a prospective cohort study. https://doi.org/10.1371/journal.pone.0124789
Zakhari A, Ates S, Shaulov T, Dahan MH (2018) Does ovarian reserve affect outcomes in single ideal blastocyst transfers in women less than 40 years of age? Arch Gynecol Obstet 297:233–239. https://doi.org/10.1007/s00404-017-4571-x
Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod 19:41–47
Dahan MH, Agdi M, Shehata F et al (2014) A comparison of outcomes from in vitro fertilization cycles stimulated with either recombinant luteinizing hormone (LH) or human chorionic gonadotropin acting as an LH analogue delivered as human menopausal gonadotropins, in subjects with good or poor ovarian reserve: a retrospective analysis. Eur J Obstet Gynecol Reprod Biol 172:70–73. https://doi.org/10.1016/j.ejogrb.2013.10.027
Gardner D, Schoolcraft W (1999) In vitro culture of human blastocyst. Parthenon Press, Carnforth, pp 378–388
Sunkara SK, Rittenberg V, Raine-Fenning N et al (2011) Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Hum Reprod 26:1768–1774. https://doi.org/10.1093/humrep/der106
Maheshwari A, Pandey S, Shetty A et al (2012) Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen thawed versus fresh embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril 98(368–77):e1–e9. https://doi.org/10.1016/j.fertnstert.2012.05.019
Evans J, Hannan NJ, Edgell TA et al (2014) Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update 20:808–821. https://doi.org/10.1093/humupd/dmu027
Ferraretti AP, Gianaroli L, Magli C et al (1999) Elective cryopreservation of all pronucleate embryos in women at risk of ovarian hyperstimulation syndrome: efficiency and safety. Hum Reprod 14:1457–1460
Shapiro BS, Daneshmand ST, Garner FC et al (2011) Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfers in high responders. Fertil Steril 96:516–518. https://doi.org/10.1016/j.fertnstert.2011.02.059
Shapiro BS, Daneshmand ST, Garner FC et al (2011) Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril 96:344–348. https://doi.org/10.1016/j.fertnstert.2011.05.050
Valbuena D, Jasper M, Remohí J et al (1999) Ovarian stimulation and endometrial receptivity. Hum Reprod 14(Suppl 2):107–111
Horcajadas JA, Riesewijk A, Polman J et al (2005) Effect of controlled ovarian hyperstimulation in IVF on endometrial gene expression profiles. Mol Hum Reprod 11:195–205. https://doi.org/10.1093/molehr/gah150
Basir GS, O WS, Ng EH, Ho PC (2001) Morphometric analysis of peri-implantation endometrium in patients having excessively high oestradiol concentrations after ovarian stimulation. Hum Reprod 16:435–440
Zhu L, Li Y, Xu A (2012) Influence of controlled ovarian hyperstimulation on uterine peristalsis in infertile women. Hum Reprod 27:2684–2689. https://doi.org/10.1093/humrep/des257
Joo BS, Park SH, An BM et al (2010) Serum estradiol levels during controlled ovarian hyperstimulation influence the pregnancy outcome of in vitro fertilization in a concentration-dependent manner. Fertil Steril 93:442–446. https://doi.org/10.1016/j.fertnstert.2009.02.066
Blazar AS, Hogan JW, Frankfurter D et al (2004) Serum estradiol positively predicts outcomes in patients undergoing in vitro fertilization. Fertil Steril 81:1707–1709. https://doi.org/10.1016/j.fertnstert.2003.10.039
Chen Z-J, Shi Y, Sun Y et al (2016) Fresh versus Frozen Embryos for Infertility in the Polycystic Ovary Syndrome. N Engl J Med 375:523–533. https://doi.org/10.1056/NEJMoa1513873
Shi Y, Sun Y, Hao C et al (2018) Transfer of Fresh versus Frozen Embryos in ovulatory women. N Engl J Med 378:126–136. https://doi.org/10.1056/NEJMoa1705334
Wei D, Yu Y, Sun M et al (2018) The effect of supraphysiological estradiol on pregnancy outcomes differs between women with PCOS and ovulatory women. J Clin Endocrinol Metab 103:2735–2742. https://doi.org/10.1210/jc.2018-00613
Lebbe M, Woodruff TK (2013) Involvement of androgens in ovarian health and disease. Mol Hum Reprod 19:828–837. https://doi.org/10.1093/molehr/gat065
Frattarelli JL, Gerber MD (2006) Basal and cycle androgen levels correlate with in vitro fertilization stimulation parameters but do not predict pregnancy outcome. Fertil Steril 86:51–57. https://doi.org/10.1016/j.fertnstert.2005.12.028
Pan D, Shi J, Zhou H et al (2018) Predictive value of basal androgen levels on ongoing pregnancy rates during in vitro fertilization cycles. Gynecol Endocrinol 34:895–899. https://doi.org/10.1080/09513590.2018.1465547
De Vos M, Pareyn S, Drakopoulos P et al (2018) Cumulative live birth rates after IVF in patients with polycystic ovaries: phenotype matters. Reprod Biomed Online 37:163–171. https://doi.org/10.1016/j.rbmo.2018.05.003
Palomba S, Falbo A, Russo T et al (2010) Pregnancy in women with polycystic ovary syndrome: the effect of different phenotypes and features on obstetric and neonatal outcomes. Fertil Steril 94:1805–1811. https://doi.org/10.1016/j.fertnstert.2009.10.043
Rodrigues JK, Navarro PA, Zelinski MB et al (2015) Direct actions of androgens on the survival, growth and secretion of steroids and anti-Mullerian hormone by individual macaque follicles during three-dimensional culture. Hum Reprod 30:664–674. https://doi.org/10.1093/humrep/deu335
Tesarik J, Mendoza C Direct non-genomic effects of follicular steroids on maturing human oocytes: oestrogen versus androgen antagonism. Hum Reprod Update 3:95–100
Gonzalez D, Thackeray H, Lewis PD et al (2012) Loss of WT1 expression in the endometrium of infertile PCOS patients: a hyperandrogenic effect? J Clin Endocrinol Metab 97:957–966. https://doi.org/10.1210/jc.2011-2366
Suikkari AM, Ruutiainen K, Erkkola R, Seppälä M (1989) Low levels of low molecular weight insulin-like growth factor-binding protein in patients with polycystic ovarian disease. Hum Reprod 4:136–139
Apparao KBC, Lovely LP, Gui Y et al (2002) Elevated endometrial androgen receptor expression in women with polycystic ovarian syndrome. Biol Reprod 66:297–304
Cermik D, Selam B, Taylor HS (2003) Regulation of HOXA-10 expression by testosterone in Vitro and in the endometrium of patients with polycystic ovary syndrome. J Clin Endocrinol Metab 88:238–243. https://doi.org/10.1210/jc.2002-021072
Schulte MMB, Tsai J, Moley KH (2015) Obesity and PCOS: the effect of metabolic derangements on endometrial receptivity at the time of implantation. Reprod Sci 22:6–14. https://doi.org/10.1177/1933719114561552
Gregory CW, Wilson EM, Apparao KBC et al (2002) Steroid receptor coactivator expression throughout the menstrual cycle in normal and abnormal endometrium. J Clin Endocrinol Metab 87:2960–2966. https://doi.org/10.1210/jcem.87.6.8572
Dahan MH, Abbasi F, Reaven G (2019) Relationship between surrogate estimates and direct measurement of insulin resistance in women with polycystic ovary syndrome. J Endocrinol Invest. https://doi.org/10.1007/s40618-019-01014-9
Eppig JJ, O’Brien MJ, Pendola FL, Watanabe S (1998) Factors affecting the developmental competence of mouse oocytes grown in vitro: follicle-stimulating hormone and insulin. Biol Reprod 59:1445–1453
Katagiri S, Moon YS, Yuen BH (1996) The role for the uterine insulin-like growth factor I in early embryonic loss after superovulation in the rat. Fertil Steril 65:426–436
Katagiri S, Moon YS, Yuen BH (1997) A somatostatin analogue decreases embryonic loss following superovulation in rats by normalizing insulin-like growth factor-I action in the uterus. Hum Reprod 12:671–676
Chi MM, Schlein AL, Moley KH (2000) High insulin-like growth factor 1 (IGF-1) and insulin concentrations trigger apoptosis in the mouse blastocyst via down-regulation of the IGF-1 receptor. Endocrinology 141:4784–4792. https://doi.org/10.1210/endo.141.12.7816
Dahan MH, Abbasi F, Reaven GM (2017) Cardiovascular disease in PCOS is related to severe insulin resistance, not mild. Minerva Endocrinol 42:294–296. https://doi.org/10.23736/S0391-1977.16.02482-2
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. NS: Manuscript writing. SA: Data collection. TA: Data collection. GS: Manuscript editing. AV-P: Manuscript editing, Data analysis. SYD: Data analysis. ST: Data collection and management, Manuscript editing. W-YS:Project development. MHD:Project development, Data analysis and Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethics approval was obtained from our institution study code 5969). And with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
No informed consent given a retrospective study.
Capsule
Transferring a fresh single ideal blastocyst to women with PCOS results in lower live birth rates compared to normal controls.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Steiner, N., Ates, S., Shaulov, T. et al. A comparison of IVF outcomes transferring a single ideal blastocyst in women with polycystic ovary syndrome and normal ovulatory controls. Arch Gynecol Obstet 302, 1479–1486 (2020). https://doi.org/10.1007/s00404-020-05699-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05699-9