Abstract
Background
The epidemiology of paraneoplastic neurological syndromes (PNS) remains to be defined. We present here the first population-based incidence study and report the clinical spectrum and antibody profile of PNS in a large area in Northeastern Italy.
Methods
We performed a 9-year (2009–2017) population-based epidemiological study of PNS in the provinces of Udine, Pordenone and Gorizia, in the Friuli-Venezia Giulia region (983,190 people as of January 1, 2017). PNS diagnosis and subgroups were defined by the 2004 diagnostic criteria. Age- and sex-adjusted incidence rates were calculated.
Results
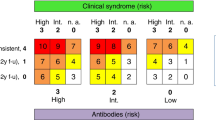
We identified 89 patients with a diagnosis of definite PNS. Median age was 68 years (range 26–90), 52% were female. The incidence of PNS was 0.89/100,000 person-years. PNS incidence rates increased over time from 0.62/100,000 person-years (2009–2011), 0.81/100,000 person-years (2012–2014) to 1.22/100,000 person-years (2015–2017). The prevalence of PNS was 4.37 per 100,000. Most common PNS were limbic encephalitis (31%), cerebellar degeneration (28%) and encephalomyelitis (20%). Among antibody (Ab)-positive cases, most frequent specificities included: Yo (30%), Hu (26%), and Ma2 (22%), while the most frequent associated tumors were lung (17%) and breast cancer (16%), followed by lymphoma (12%). PNS developed in 1 in every 334 cancers in our region. Statistically significant associations were observed between cancer type and Ab-specificity (P < 0.001), and between neurological syndrome and Ab-specificity (P < 0.001).
Conclusions
This first population-based study found an incidence of PNS that approximates 1/100,000 person-years and a prevalence of 4/100,000. Moreover, the incidence of PNS is increasing over time, probably due to increased awareness and improved detection techniques.


Similar content being viewed by others
Data access, responsibility, and analysis
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Darnell RB, Posner JB (2003) Paraneoplastic syndromes involving the nervous system. N Engl J Med 349:1543–1554. https://doi.org/10.1056/NEJMra023009
Honnorat J, Antoine J-C (2007) Paraneoplastic neurological syndromes. Orphanet J Rare Dis 2:22. https://doi.org/10.1186/1750-1172-2-22
Dalmau J, Graus F (2018) Antibody-mediated encephalitis. N Engl J Med 378:840–851. https://doi.org/10.1056/NEJMra1708712
Graus F, Titulaer MJ, Balu R et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404. https://doi.org/10.1016/S1474-4422(15)00401-9
Vogrig A, Joubert B, Ducray F et al (2018) Glioblastoma as differential diagnosis of autoimmune encephalitis. J Neurol 265:669–677. https://doi.org/10.1007/s00415-018-8767-1
Graus F, Delattre JY, Antoine JC et al (2004) Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 75:1135–1140. https://doi.org/10.1136/jnnp.2003.034447
Bettini M, Chaves M, Cristiano E et al (2017) Incidence of autoimmune myasthenia gravis in a health maintenance organization in Buenos Aires, Argentina. Neuroepidemiology 48:119–123. https://doi.org/10.1159/000477733
Breiner A, Widdifield J, Katzberg HD et al (2016) Epidemiology of myasthenia gravis in Ontario, Canada. Neuromuscul Disord 26:41–46. https://doi.org/10.1016/j.nmd.2015.10.009
Martinka I, Fulova M, Spalekova M, Spalek P (2018) Epidemiology of myasthenia gravis in Slovakia in the years 1977–2015. Neuroepidemiology 50:153–159. https://doi.org/10.1159/000487886
Popperud TH, Boldingh MI, Brunborg C et al (2017) Juvenile myasthenia gravis in Norway: a nationwide epidemiological study. Eur J Paediatr Neurol 21:312–317. https://doi.org/10.1016/j.ejpn.2016.09.001
Monaco S, Turri E, Zanusso G, Maistrello B (2004) Treatment of inflammatory and paraproteinemic neuropathies. Curr Drug Targets Immune Endocr Metabol Disord 4:141–148
Naing NN (2000) Easy way to learn standardization: direct and indirect methods. Malays J Med Sci 7:10–15
Keyfitz N (1966) Finite approximations in demography. Popul Stud (Camb) 19:281–295. https://doi.org/10.1080/00324728.1966.10406017
Vogrig A, Joubert B, André-Obadia N et al (2019) Seizure specificities in patients with antibody-mediated autoimmune encephalitis. Epilepsia 60:1508–1525. https://doi.org/10.1111/epi.16282
Kanikannan MA, Sirisha Y, Uppin MS et al (2015) Incidence and spectrum of paraneoplastic neurological syndromes: single center study. J Neurooncol 125:197–206. https://doi.org/10.1007/s11060-015-1898-7
Chan AM, Baehring JM (2019) Paraneoplastic neurological syndromes: a single institution 10-year case series. J Neurooncol 141:431–439. https://doi.org/10.1007/s11060-018-03053-3
Hayat MJ, Howlader N, Reichman ME, Edwards BK (2007) Cancer statistics, trends, and multiple primary cancer analyses from the Surveillance, Epidemiology, and End Results (SEER) Program. Oncologist 12:20–37. https://doi.org/10.1634/theoncologist.12-1-20
Ducray F, Graus F, Vigliani MC et al (2010) Delayed onset of a second paraneoplastic neurological syndrome in eight patients. J Neurol Neurosurg Psychiatry 81:937–939. https://doi.org/10.1136/jnnp.2009.190199
Dubey D, Pittock SJ, Kelly CR et al (2018) Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol 83:166–177. https://doi.org/10.1002/ana.25131
Talbott EO, Malek AM, Lacomis D (2016) The epidemiology of amyotrophic lateral sclerosis. Handb Clin Neurol 138:225–238. https://doi.org/10.1016/B978-0-12-802973-2.00013-6
Zarei S, Carr K, Reiley L et al (2015) A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int. https://doi.org/10.4103/2152-7806.169561
Giometto B, Grisold W, Vitaliani R et al (2010) Paraneoplastic neurologic syndrome in the PNS Euronetwork database: a European study from 20 centers. Arch Neurol 67:330–335. https://doi.org/10.1001/archneurol.2009.341
Vogrig A, Ferrari S, Tinazzi M et al (2015) Anti-Ma-associated encephalomyeloradiculopathy in a patient with pleural mesothelioma. J Neurol Sci 350:105–106. https://doi.org/10.1016/j.jns.2015.01.028
Dalmau J (2004) Clinical analysis of anti-Ma2-associated encephalitis. Brain 127:1831–1844. https://doi.org/10.1093/brain/awh203
Vogrig A, Joubert B, Maureille A et al (2018) Motor neuron involvement in anti-Ma2-associated paraneoplastic neurological syndrome. J Neurol 266:398–410. https://doi.org/10.1007/s00415-018-9143-x
Vogrig A, Fouret M, Joubert B et al (2019) Increased frequency of anti-Ma2 encephalitis associated with immune checkpoint inhibitors. Neurol Neuroimmunol Neuroinflamm 6:e604. https://doi.org/10.1212/NXI.0000000000000604
Maureille A, Fenouil T, Joubert B et al (2018) Isolated seizures are a common early feature of paraneoplastic anti-GABAB receptor encephalitis. J Neurol. https://doi.org/10.1007/s00415-018-9132-0
Vogrig A, Pauletto G, Belgrado E et al (2018) Effect of thymectomy on refractory autoimmune status epilepticus. J Neuroimmunol 317:90–94. https://doi.org/10.1016/j.jneuroim.2018.01.009
Camdessanché J-P, Jousserand G, Ferraud K et al (2009) The pattern and diagnostic criteria of sensory neuronopathy: a case-control study. Brain 132:1723–1733. https://doi.org/10.1093/brain/awp136
Shams’ili S, Grefkens J, de Leeuw B et al (2003) Paraneoplastic cerebellar degeneration associated with antineuronal antibodies: analysis of 50 patients. Brain 126:1409–1418
McKeon A, Tracy JA, Pittock SJ et al (2011) Purkinje cell cytoplasmic autoantibody type 1 accompaniments: the cerebellum and beyond. Arch Neurol 68:1282–1289. https://doi.org/10.1001/archneurol.2011.128
Ventura L, Giorgi D, Giordano L et al (2015) Mammographic breast cancer screening in Italy: 2011–2012 survey. Epidemiol Prev 39:21–29
Vogrig A, Zanoni T, Moretto G (2016) Nystagmus and lower extremity hyperalgesia after colectomy. JAMA 316:1488–1489. https://doi.org/10.1001/jama.2016.13658
Do L-D, Chanson E, Desestret V et al (2017) Characteristics in limbic encephalitis with anti-adenylate kinase 5 autoantibodies. Neurology 88:514–524. https://doi.org/10.1212/WNL.0000000000003586
Spatola M, Petit-Pedrol M, Simabukuro MM et al (2017) Investigations in GABAA receptor antibody-associated encephalitis. Neurology 88:1012–1020. https://doi.org/10.1212/WNL.0000000000003713
Gaig C, Graus F, Compta Y et al (2017) Clinical manifestations of the anti-IgLON5 disease. Neurology 88:1736–1743. https://doi.org/10.1212/WNL.0000000000003887
Hara M, Ariño H, Petit-Pedrol M et al (2017) DPPX antibody–associated encephalitis: main syndrome and antibody effects. Neurology 88:1340–1348. https://doi.org/10.1212/WNL.0000000000003796
Mandel-Brehm C, Dubey D, Kryzer TJ et al (2019) Kelch-like protein 11 antibodies in seminoma-associated paraneoplastic encephalitis. N Engl J Med 381:47–54. https://doi.org/10.1056/NEJMoa1816721
Funding
No targeted funding reported.
Author information
Authors and Affiliations
Contributions
Study concept and design: AV. Acquisition of data: AV, SS, EC, AM, AB, MF, PP and MR. Analysis and interpretation of data: AV, GLG, SS, EC, AM, AB, FV, MF, FC, FB, DI, PP, MR, JH and MV. Drafting of the manuscript: AV. Critical revision of the manuscript for important intellectual content: AV, GLG, SS, EC, AM, AB, FV, MF, FC, FB, DI, PP, MR, JH and MV. Study supervision: GLG and MV. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures were performed in accordance with the institutional ethics committee and the Declaration of Helsinki.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vogrig, A., Gigli, G.L., Segatti, S. et al. Epidemiology of paraneoplastic neurological syndromes: a population-based study. J Neurol 267, 26–35 (2020). https://doi.org/10.1007/s00415-019-09544-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09544-1