Abstract
Objectives
To evaluate the comparative outcomes of three-dimensional (3D) versus two-dimensional (2D) imaging during laparoscopic cholecystectomy.
Methods
We conducted a systematic search of electronic information sources and bibliographic reference lists and applied a combination of free text and controlled vocabulary search adapted to thesaurus headings, search operators and limits. Procedure time, Calot’s triangle dissection time, gallbladder removal time, gallbladder perforation, intraoperative bleeding, postoperative complications, conversion to open and intraoperative errors were the evaluated outcome parameters.
Results
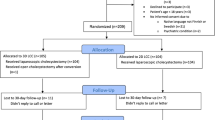
We identified 6 randomised controlled trials (RCT) reporting a total of 577 patients who underwent laparoscopic cholecystectomy using 3D (n = 282) or 2D (n = 295) imaging. The 3D imaging was associated with significantly shorter procedure time (MD − 4.23, 95% CI − 8.14 to − 0.32, p = 0.03), Calot’s triangle dissection time (MD − 4.19, 95% CI − 6.52 to − 1.86, p = 0.0004) and significantly lower risk of gallbladder perforation (RR 0.50, 95% CI 0.28–0.88, p = 0.02) compared to the 2D approach. No significant difference was found in gallbladder removal time (MD − 0.79, 95% CI − 2.24 to 0.66, p = 0.28), intraoperative bleeding (RR 1.14, 95% CI 0.68–1.90, p = 0.61), postoperative complications (RD − 0.01, 95% CI − 0.06 to 0.05, p = 0.85), conversion to open (RD 0.00, 95% CI − 0.02 to 0.03, p = 0.70) or intraoperative errors (RR 0.96, 95% CI 0.79–1.17, p = 0.70) between the two groups.
Conclusions
Although our findings suggest that the use of 3D imaging during laparoscopic cholecystectomy may be associated with significantly shorter procedure time, Calot’s triangle dissection time and gallbladder injury compared to the 2D imaging, the differences seem to be clinically insignificant. Moreover, both approaches carry s similar risk of postoperative morbidities. The impact of the surgeon’s level of experience and difficulty of the procedure on the outcomes of each imaging modality remains unknown.




Similar content being viewed by others
References
National Institute for Health and Care Excellence. (2014) Costing statement: gallstone disease – implementing the NICE guideline on gallstone disease (CG188). 2014
Gadacz T, Talamini M (1991) Traditional versus laparoscopic cholecystectomy. Am J Surg 161(3):336–338
Byrn JC, Schluender S, Divino CM, Conrad J, Gurland B, Shlasko E, Szold A (2007) Three-dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci robot system. Am J Surg 193(4):519–522
Gurusamy KS, Sahay S, Davidson BR (2011) Three dimensional versus two dimensional imaging for laparoscopic cholecystectomy. Cochrane database of systematic reviews, issue 1. Art. No.: CD006882. DOI: https://doi.org/10.1002/14651858.CD006882.pub2
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 339:b2700
Higgins JP, Altman DG, editors Chapter 8 (2018) Assessing risk of bias in included studies. In: Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.0.1[updated September 2008]. Available at: http://hiv.cochrane.org/sites/hiv. cochrane.org/files/uploads/Ch08_Bias.pdf
Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet. 351(9098):248–251
Bilgen K, Ustun M, Karakahya M et al (2013) Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23:180–183
Curro G, La Malfa G, Lazzara S (2015) Three-dimensional versus two-dimensional laparoscopic cholecystectomy: is surgeon experience relevant? J Laparoendosc Adv Surg Tech A 2015; 25:566–570
Sahu D, Mathew MJ, Reddy PK (2014) 3D laparoscopy - help or hype; initial experience of a tertiary health centre. JCDR. 8(7):NC01–NC03. https://doi.org/10.7860/JCDR/2014/8234.4543
Koppatz H, Harju J, Siren J et al (2019) Three-dimensional versus two-dimensional high-definition laparoscopy in cholecystectomy: a prospective randomized controlled study. Surg Endosc 33(11):3725–3731
Schwab KE, Curtis NJ, Whyte MB, Smith RV, Rockall TA, Ballard K, Jourdan IC (2020) 3D laparoscopy does not reduce operative duration or errors in day-case laparoscopic cholecystectomy: a randomised controlled trial. Surg Endosc 34(4):1745–1753
Li L, Gao X, Guo Y, Luo Y, Luo Y, Yang X, Zhang W, Feng L (2019) Comparison of three-dimensional versus two-dimensional laparoscopic surgery for rectal cancer: a meta-analysis. Int J Color Dis 34:1577–1583. https://doi.org/10.1007/s00384-019-03353-8
Pantalos G, Patsouras D, Spartalis E et al (2020) Three-dimensional versus two-dimensional laparoscopic surgery for colorectal cancer: systematic review and meta-analysis. Vivo. 34(1):11–21
Liang H, Liang W, Lei Z et al (2018) Three-dimensional versus two-dimensional video-assisted endoscopic surgery: a meta-analysis of clinical data. World J Surg 42:3658–3668. https://doi.org/10.1007/s00268-018-4681-z
Peponis T, Eskesen TG, Mesar T, Saillant N, Kaafarani HMA, Yeh DD, Fagenholz PJ, de Moya MA, King DR, Velmahos GC (2018) Bile spillage as a risk factor for surgical site infection after laparoscopic cholecystectomy: a prospective study of 1,001 patients. J Am Coll Surg 226(6):1030–1035. https://doi.org/10.1016/j.jamcollsurg.2017.11.025
Misra M, Schiff J, Rendon J, et al (2015) Laparoscopic cholecystectomy after the learning curve. Surg Endosc 2005;19:1266–1271
Lukovich P, Zsirka A, Harsanyi L (2014) Changes in the operating time of laparoscopic cholecystectomy of the surgeons and novices between 1994–2012. Chirurgia. 109:639–643
Grau-Talens EJ, Motos-Micó JJ, Giraldo-Rubio R, Aparicio-Gallego JM, Salgado JF, Ibáñez CD, Mangione-Castro PG, Arribas-Jurado M, Jordán-Chaves C, Arias-Díaz J (2018) Small-incision cholecystectomy (through a cylinder retractor) under local anaesthesia and sedation: a prospective observational study of five hundred consecutive cases. Langenbeck's Arch Surg 403(6):733–740. https://doi.org/10.1007/s00423-018-1707-9
Hozo S, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Author information
Authors and Affiliations
Contributions
Conception and design: Shahin H. Literature search and study selection: SD and MG. Data collection: SD, MG, Shahab H and Shahin H. Analysis and interpretation: Shahin H and Shahab H. Writing the article: SD, MG and Shahin H. Critical revision of the article: all authors. Final approval of the article: all authors. Statistical analysis: Shahin H and Shahab H.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Considering the design of our study, ethical approval and consent were not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Table 1 Search strategy
Search no. | Search strategy* |
|---|---|
#1 | MeSH descriptor: [cholecystectomy] explode all trees |
#2 | cholecystectomy: TI,AB,KW |
#3 | MeSH descriptor: [Laparoscopic cholecystectomy] explode all trees |
#4 | Laparoscopic cholecystectomy: TI,AB,KW |
#5 | #1 OR #2 OR #3 OR #4 |
#6 | MeSH descriptor: [3 dimensional ] explode all trees |
#7 | 3 dimensional : TI,AB,KW |
#8 | MeSH descriptor: [3D ] explode all trees |
#9 | 3D : TI,AB,KW |
#10 | MeSH descriptor: [2 dimensional ] explode all trees |
#11 | 2 dimensional : TI,AB,KW |
#12 | MeSH descriptor: [2D] explode all trees |
#13 | 2D : TI,AB,KW |
#14 | MeSH descriptor: [three-dimensional] explode all trees |
#15 | three-dimensional : TI,AB,KW |
#16 | MeSH descriptor: [ two-dimensional ] explode all trees |
#17 | two-dimensional : TI,AB,KW |
#18 | #6 OR #7 OR #8 OR #9 #10 OR #11 OR #12 OR #13 #14 OR #15 OR #16 OR #17 |
#19 | #5 AND #18 |
Rights and permissions
About this article
Cite this article
Davies, S., Ghallab, M., Hajibandeh, S. et al. Three-dimensional versus two-dimensional imaging during laparoscopic cholecystectomy: a systematic review and meta-analysis of randomised controlled trials. Langenbecks Arch Surg 405, 563–572 (2020). https://doi.org/10.1007/s00423-020-01909-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01909-9