Abstract
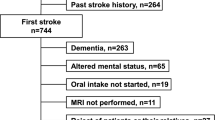
Aim of this study was to investigate the effect of post-stroke oral apraxia on dysphagia in patients with subacute stroke. We retrospectively analyzed the clinical data of 130 supratentorial stroke patients from January 2015 to February 2021 who underwent a formal limb and oral apraxia test and videofluoroscopic swallowing study (VFSS), and we compared the patients in two groups: the apraxia and non-apraxia (oral apraxia score > 45 and ≤ 45 points, respectively). All the patients participated in the standardized testing battery. The test variables were videofluoroscopic dysphagia scale (VDS), oral transit time (OTT), pharyngeal delay time (PDT), pharyngeal transit time, and penetration-aspiration scale (PAS); we conducted multivariable regression analysis with those parameters to confirm the significance of oral apraxia as a clinical determinant of post-stroke dysphagia. The mean oral apraxia scores were 38.4 and 47.6 points in the apraxia and non-apraxia groups, respectively (p < 0.001). The apraxia group had a higher proportion of delayed OTT for the 2-mL-thick liquid than the non-apraxia group (17.6% and 4.2%, respectively; p = 0.011). Oral apraxia was a significant determinant of VDS (p < 0.001), delayed OTT of 2-mL-thick liquids (p = 0.028), delayed PDT of cup drinking for thin liquid (p = 0.044), and PAS scores (p = 0.003). The presence of oral apraxia was significantly associated with dysphagia, especially with the VFSS parameters of the oral phase (thick liquid), pharyngeal phase (cup drinking for thin liquid) of swallowing, and increased risk of aspiration in subacute stroke patients. Thus, a formal assessment of oral apraxia is needed for stroke patients with dysphagia.

Similar content being viewed by others
References
Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS. Recovery of walking function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil. 1995;76:27–32.
Lee SY, Kim BR, Han EY. Association between evoked potentials and balance recovery in subacute hemiparetic stroke patients. Ann Rehabil Med. 2015;39:451–61.
Abdel Jalil AA, Katzka DA, Castell DO. Approach to the patient with dysphagia. Am J Med. 2015;128:1138.e17-23.
Broadley S, Croser D, Cottrell J, Creevy M, Teo E, Yiu D, et al. Predictors of prolonged dysphagia following acute stroke. J Clin Neurosci. 2003;10:300–5.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Smithard DG, O’Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. does dysphagia matter? Stroke. 1996;27:1200–4.
González-Fernández M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after stroke: an overview. Curr Phys Med Rehabil Rep. 2013;1:187–96.
Martin-Harris B, Michel Y, Castell DO. Physiologic model of oropharyngeal swallowing revisited. Otolaryngol Head Neck Surg. 2005;133:234–40.
Han H, Shin G, Jun A, Park T, Ko D, Choi E, et al. The relation between the presence of aspiration or penetration and the clinical indicators of dysphagia in poststroke survivors. Ann Rehabil Med. 2016;40:88–94.
Moon HI, Yoon SY, Yi TI, Jeong YJ, Cho TH. Lesions responsible for delayed oral transit time in post-stroke dysphagia. Dysphagia. 2018;33:321–8.
Ja L. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-ED; 1998.
Logemann JA, Shanahan T, Rademaker AW, Kahrilas PJ, Lazar R, Halper A. Oropharyngeal swallowing after stroke in the left basal ganglion/internal capsule. Dysphagia. 1993;8:230–4.
Rothi LJ, Heilman KM, Watson RT. Pantomime comprehension and ideomotor apraxia. J Neurol Neurosurg Psychiatry. 1985;48:207–10.
Gonzalez Rothi LJG, Ochipa C, Heilman KM. A cognitive neuropsychological model of limb praxis. Cogn Neuropsychol. 1991;8:443–4.
Foundas AL, Henchey R, Gilmore RL, Fennell EB, Heilman KM. Apraxia during Wada testing. Neurology. 1995;45:1379–83.
Foundas AL, Macauley BL, Raymer AM, Maher LM, Heilman KM, Gonzalez Rothi LJ. Ecological implications of limb apraxia: evidence from mealtime behavior. J Int Neuropsychol Soc. 1995;1:62–6.
Pyun SB, Hwang YM, Jo SY, Ha JW. Reliability and validity of the comprehensive limb and oral apraxia test: standardization and clinical application in Korean patients with stroke. Ann Rehabil Med. 2019;43:544–54.
Brust JCM. Aphasia, apraxia, and agnosia. In: The physiological basis of Rehabiliation medicine. 2nd ed. Oxford: Butterworth-Heinemann; 1995. p. 647–58.
Yun YJ, Na YJ, Han SH. Swallowing apraxia in a patient with recurrent ischemic strokes: a case report. Medicine. 2019;98: e17056.
Daniels SK, Brailey K, Foundas AL. Lingual discoordination and dysphagia following acute stroke: analyses of lesion localization. Dysphagia. 1999;14:85–92.
Mann G, Hankey GJ. Initial clinical and demographic predictors of swallowing impairment following acute stroke. Dysphagia. 2001;16:208–15.
Horner J, Massey EW. Silent aspiration following stroke. Neurology. 1988;38:317–9.
Smith HA, Lee SH, O’Neill PA, Connolly MJ. The combination of bedside swallowing assessment and oxygen saturation monitoring of swallowing in acute stroke: a safe and humane screening tool. Age Ageing. 2000;29:495–9.
Cichero JAY, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32:293–314.
Han TR, Park JW. The functional dysphagia scale using videofluoroscopic swallowing study in stroke patients. J Korean Acad Rehab Med. 1999;23:1118–26.
Park YW, Kim CH, Kim MO, Jeong HJ, Jung HY. Alien hand syndrome in stroke—case report & neurophysiologic study -. Ann Rehabil Med. 2012;36:556–60.
Soares TJ, Moraes DP, de Medeiros GC, Sassi FC, Zilberstein B, de Andrade CR. Oral transit time: a critical review of the literature. Arq Bras Cir Dig. 2015;28:144–7.
Jeon WH, Park GW, Lee JH, Jeong HJ, Sim YJ. Association between location of brain lesion and clinical factors and findings of videofluoroscopic swallowing study in subacute stroke patients. Brain Neurorehabil. 2014;7:54–60.
Molfenter SM, Steele CM. Temporal variability in the deglutition literature. Dysphagia. 2012;27:162–77.
Kang SH, Kim DK, Seo KM, Seo JH. Usefulness of videofluoroscopic swallow study with mixed consistency food for patients with stroke or other brain injuries. J Korean Med Sci. 2011;26:425–30.
Borders JC, Brates D. Use of the penetration-aspiration scale in dysphagia research: a systematic review. Dysphagia. 2020;35:583–97.
Daniels SK, Foundas AL, Iglesia GC, Sullivan MA. Lesion site in unilateral stroke patients with dysphagia. J Stroke Cerebrovasc Dis. 1996;6:30–3.
Daniels SK. Swallowing apraxia: a disorder of the Praxis system? Dysphagia. 2000;15:159–66.
Kent RD, Rosenbek JC. Acoustic patterns of apraxia of speech. J Speech Hear Res. 1983;26:231–49.
Cassiani RA, Santos CM, Parreira LC, Dantas RO. The relationship between the oral and pharyngeal phases of swallowing. Clinics (Sao Paulo). 2011;66:1385–8.
Loret C. Using sensory properties of food to trigger swallowing: a review. Crit Rev Food Sci Nutr. 2015;55:140–5.
Power ML, Hamdy S, Goulermas JY, Tyrrell PJ, Turnbull I, Thompson DG. Predicting aspiration after hemispheric stroke from timing measures of oropharyngeal bolus flow and laryngeal closure. Dysphagia. 2009;24:257–64.
Lin CW, Chang YC, Chen WS, Chang K, Chang HY, Wang TG. Prolonged swallowing time in dysphagic Parkinsonism patients with aspiration pneumonia. Arch Phys Med Rehabil. 2012;93:2080–4.
DeMatteo C, Matovich D, Hjartarson A. Comparison of clinical and videofluoroscopic evaluation of children with feeding and swallowing difficulties. Dev Med Child Neurol. 2005;47:149–57.
Ozaki K, Kagaya H, Yokoyama M, Saitoh E, Okada S, González-Fernández M, et al. The risk of penetration or aspiration during videofluoroscopic examination of swallowing varies depending on food types. Tohoku J Exp Med. 2010;220:41–6.
Robbins J, Levin RL. Swallowing after unilateral stroke of the cerebral cortex: preliminary experience. Dysphagia. 1988;3:11–7.
Robbins JA, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993;74:1295–300.
Saito T, Hayashi K, Nakazawa H, Ota T. Clinical characteristics and lesions responsible for swallowing hesitation after acute cerebral infarction. Dysphagia. 2016;31:567–73.
Wilmskoetter J, Bonilha L, Martin-Harris B, Elm JJ, Horn J, Bonilha HS. Mapping acute lesion locations to physiological swallow impairments after stroke. NeuroImage Clin. 2019;22: 101685.
Logemann JA. Medical and rehabilitative therapy of oral, pharyngeal motor disorders. GI Motil Online. 2006.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19(691–707):vii.
Acknowledgements
We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This study was funded by the National Research Foundation of the Korean Government (NRF-2022R1A2B5B02001673).
Author information
Authors and Affiliations
Contributions
Conceptualization (S-BP), methodology (S-BP, JHM), data curation (JHM), formal analysis (JHM), investigation (S-BP, JHM), projection administration (S-BP), validation (S-BP, JHM), writing the original draft (JHM); and critical review and editing (S-BP).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Formal consent was not required for this type of study.
Informed Consent
This study was approved by the Institutional Review Board of Korea University Anam Medical Center (no. 2021AN0151) and conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was waived owing to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Myung, J.H., Pyun, SB. Effect of Oral Apraxia on Dysphagia in Patients with Subacute Stroke. Dysphagia 38, 227–235 (2023). https://doi.org/10.1007/s00455-022-10458-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10458-w