Abstract
Goals of the work
Patients with head and neck cancer have complex needs that affect many basic functions of life and contribute to substantial psychosocial problems. The aim of this study was to evaluate the effectiveness of a problem-focused intervention for patients with psychosocial dysfunction who had completed treatment for head and neck cancer.
Patients and methods
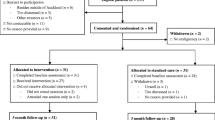
Using a quasi-experimental design, 54 participants who were above pre-determined cutoff points for psychosocial dysfunction (hospital and depression scale, work and social adjustment scale) were given the opportunity to self-select into either the experimental group for the psychosocial intervention programme which was delivered in an individualised format, with bibliotherapy as an adjunct, or the control group for usual care.
Main results
Analysis of covariance results demonstrated a reduction in psychological distress (anxiety, p = 0.001; depression, p = 0.005), improving social functioning (p = 0.048) and quality of life scores (p = <0.05) for the experimental group, all of which were sustained into the 3-month follow-up period. No such improvements were evident for the control group.
Conclusions
This study suggests that head and neck cancer patients with post-treatment psychosocial dysfunction can benefit from a problem-focused psychosocial intervention. Such evidence can inform practice, policy and future research, aimed at improving post-treatment quality of life for patients with head and neck cancer.




Similar content being viewed by others
References
Allison PJ, Nicolau B, Edgar L, Archer J, Black M, Heir M (2004) Teaching head and neck cancer patients coping strategies: results of a feasibility study. Oral Oncol 40:538–544. doi:10.1016/j.oraloncology.2003.11.008
Berglund G, Bolund C, Gustafsson UL, Sjoden PO (1994) One-year follow-up of the ‘Starting Again’ group rehabilitation programme for cancer patients. Eur J Cancer Care (Engl) 30A:1744–1751
Bouland G (1985) Suicide and cancer II: medical factors in suicide by cancer patients in Sweden, 1973–1976. J Psychol Oncol 3:31–35. doi:10.1300/J077v03n01_03
Carver CS (1997) You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med 4(1):92–100. doi:10.1207/s15327558ijbm0401_6
Carver CS, Scheier M, Weintraub J (1989) Assessing coping strategies. A theoretically based approach. J Pers Soc Psychol 56:267–283. doi:10.1037/0022-3514.56.2.267
Clarke A (2001) Resourcing and training head and neck cancer nurse specialists to deliver a social rehabilitation programme to patients. Ph.D. thesis, City University, London.
Duffy SA, Ronis DL, Valenstein M, Lambert MT, Fowler KE, Gregory L et al (2006) A tailored smoking, alcohol and depression intervention for head and neck cancer patients. Cancer Epidemiol Biomarkers Prev 15(11):2203–2208. doi:10.1158/1055-9965.EPI-05-0880
Everson DK (1999) Prediction of treatment attrition in a psychological training clinic using the personal assessment inventory, client variables and therapist abilities. Dissertation abstract. 60(2-B):826
Fiegenbaum W (1981) A social training program for clients with facial disfigurements: a contribution to the rehabilitation of cancer patients. Int J Rehabil Res 4:501–509. doi:10.1097/00004356-198112000-00003
Frampton M (2001) Psychological distress for patients with head and neck cancer. Br J Oral Maxillofac Surg 39(1):67–70, review. doi:10.1054/bjom.2000.0547
Gilbar O, Neuman R (2002) Which cancer patients completes a psychosocial intervention program? Psychooncology 11:461–471. doi:10.1002/pon.608
Greer S, Moorey S, Baruch JDR, Watson M, Robertson BM, Mason A et al (1992) Adjuvant psychological therapy for patients with cancer: a prospective randomised trial. BMJ 304:675–680
Hammerlid E, Bjordal K, Ahlner-Elmqvist M, Jannert M, Kaasa S, Sullivan M et al (1997) Prospective longitudinal quality of life study of patients with head and neck cancer: a feasibility including EORTC QLQ C30. Otolaryngol Head Neck Surg 116:666–673. doi:10.1016/S0194-5998(97)70246-8
Hammerlid E, Ahlner-Elmqvist M, Bjordal K, Biorklund A, Evensen J, Boysen M et al (1999) A prospective multicentre study in Sweden & Norway of mental distress and psychiatric morbidity in head and neck cancer patients. Br J Cancer 80(5/6):766–774. doi:10.1038/sj.bjc.6690420
Hammerlid E, Persson L, Sullivan M, Westin T (1999) Quality-of-life effects of psychosocial intervention in patients with head and neck cancer. Otolaryngol Head Neck Surg 120:507–516. doi:10.1053/hn.1999.v120.a90352
Hassanein KA, Musgrove BT, Bradbury E (2005) Psychological outcome of patients following treatment of oral cancer and its relation with coping status and coping mechanism. J Craniomaxillofac Surg 33(6):404–409
Howe D (1993) On being a client: understanding the process of counselling and psychotherapy. Sage, London
Humphris GM, Rogers S (2004) The association of cigarette smoking and anxiety, depression and fear of recurrence in patients following treatment of oral and oropharyngeal malignancy. Eur J Cancer Care (Engl) 13(4):328–334. doi:10.1111/j.1365-2354.2004.00479.x
Humphris GM, Ozakinci G (2006) Psychological responses and support needs of patients following head and neck cancer. Int J Surg 4:37–44. doi:10.1016/j.ijsu.2005.12.004
Katz MR, Irish JC, Devins GM, Rodin GM, Gullane PJ (2000) Reliability and validity of an observer-rated disfigurement scale for head and neck cancer patients. Head Neck 22:132–141. doi:10.1002/(SICI)1097-0347(200003)22:2<132::AID-HED4>3.0.CO;2-K
Katz MR, Irish JC, Devins GM (2004) Development and pilot testing of a psychoeducational intervention for oral cancer patients. Psychooncology 13:642–653. doi:10.1002/pon.767
Maccormack T, Simonian J, Lim J, Redomd L, Roets D, Dunn S et al (2001) ‘Someone who cares:’ a qualitative investigation of cancer patients’ experiences of psychotherapy. Psychooncology 10:52–65. doi:10.1002/1099-1611(200101/02)10:1<52::AID-PON489>3.0.CO;2-V
Marks I (1986) Behavioural psychotherapy. Wright, Bristol
Moynihan C, Bliss JM, Davidson J, Burchell L, Horwich A (1998) Evaluation of adjuvant psychological therapy in patients with testicular cancer: randomised controlled trial. BMJ 316:429–435
Mundt JC, Marks IM, Shear MK, Greist JH (2002) The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry 180:461–464. doi:10.1192/bjp.180.5.461
National Institute for Clinical Excellence (2004) Guidance on cancer services: improving outcomes in head and neck cancer—the manual. National Institute for Clinical Excellence, London
Orlinsky DE, Howard KJ (1986) Process and outcome in psychotherapy. In: Handbook of psychotherapy and behavior change, 3rd edn. Wiley, New York
Rogers SN, Gwanne S, Lowe D, Humphris G, Yueh B, Welmuller EA (2002) The addition of mood and anxiety domains to the University of Washington Quality of Life Scale. Head Neck 24:521–519. doi:10.1002/hed.10106
Sarason BR, Shearin EN, Pierce GR, Sarason IG (1987) Interrelationships among social support measures: theoretical and practical implications. J Pers Soc Psychol 52:813–832. doi:10.1037/0022-3514.52.4.813
Scheier MF, Carver CS (1987) Dispositional optimism and physical well-being: the influence of generalized outcome expectancies on health. J Pers 55:169–210. doi:10.1111/j.1467-6494.1987.tb00434.x
Semple CJ, Dunnwoody L, Kernohan GW, Sullivan K (2006) Patients with head and neck cancer prefer individualized cognitive behaviour therapy. Eur J Cancer Care 15(3):220–227
Sheard T, Maguire P (1999) The effect of psychological interventions on anxiety and depression in cancer patients: results of two meta-analysis. Br J Cancer 80:1770–1780. doi:10.1038/sj.bjc.6690596
Yalmon I (1985) Theory and practice of group psychotherapy. Basic Books, London
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S (2001) The prevalence of psychological distress by cancer site. Psychooncology 10:19–28. doi:10.1002/1099-1611(200101/02)10:1<19::AID-PON5017>3.0.CO;2-6
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 63:361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
Acknowledgement
This research was funded by the Research and Development Office for the Department of Health, Social Services and Public Safety, Northern Ireland. The authors would like to express their thanks to Kelly Craig for her dedication to the project as research assistant and to Professor Kate Sullivan who provided very valuable help in the design of the project and the bibliotherapeutic texts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Semple, C.J., Dunwoody, L., Kernohan, W.G. et al. Development and evaluation of a problem-focused psychosocial intervention for patients with head and neck cancer. Support Care Cancer 17, 379–388 (2009). https://doi.org/10.1007/s00520-008-0480-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-008-0480-7