Abstract
Purpose
We aimed to compare the effects of saline with and without heparin on the catheter-occlusion rate and coagulation-related blood test results for the management of arterial catheters among patients admitted to a short-term intensive care unit postoperatively.
Methods
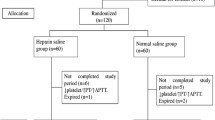
This prospective, triple-blinded, randomized controlled study recruited patients aged 20–90 years scheduled to undergo radial arterial catheter insertion and postoperative intensive care unit admission between February and August 2019. Patients were randomly allocated to two groups (1:1 ratio) depending on the use of heparin: study (normal saline with heparin, 3000 units to 500 ml of normal saline) and control (normal saline without heparin) groups with arterial catheters. The allocated management method was employed immediately after intensive care unit admission. Occlusion assessment (every 12 h), arterial blood gas tests (every 6 h), and blood sample collection (every 24 h) were performed. The occlusion of arterial catheter was assessed using occlusion rate, and blood test results were assessed using a linear mixed model.
Results
There were 147 patients in the arterial catheter groups. There were no significant differences in occlusion rates and changes in platelet counts and activated partial thromboplastin time between the groups with arterial (p = 0.98, 0.16, and 0.32, respectively) catheters during the first 6 days after intensive care unit admission.
Conclusion
Normal saline with and without heparin showed similar efficiency for both the prevention of occlusion and the results of coagulation.


Similar content being viewed by others
References
Pinsky MR. Hemodynamic monitoring in the intensive care unit. Clin Chest Med. 2003;24:549–60.
Cruzeiro PC, Camargos PA, Tatsuo ES, Piçarro C, Campos BA, Paixão RM, Pontes AK, Teixeira CR, Miranda ME. Percutaneous central venous catheterization through the external jugular vein in children: is inserting the guide wire into the superior vena cava essential for successful catheterization? J Pediatr Surg. 2012;47:1742–7.
Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M, ESPEN. ESPEN Guidelines on Parenteral Nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009;28:365–77.
Zevola DR, Dioso J, Moggio R. Comparison of heparinized and nonheparinized solutions for maintaining patency of arterial and pulmonary artery catheters. Am J Crit Care. 1997;6:52–5.
de Neef M, Heijboer H, van Woensel JB, de Haan RJ. The efficacy of heparinization in prolonging patency of arterial and central venous catheters in children: a randomized double-blind trial. Pediatr Hematol Oncol. 2002;19:553–60.
Clifton GD, Branson P, Kelly HJ, Dotson LR, Record KE, Phillips BA, Thompson JR. Comparison of normal saline and heparin solutions for maintenance of arterial catheter patency. Heart Lung. 1991;20:115–8.
Cormack GM, Kaufman LJ. Severe heparin-induced thrombocytopenia: when the obvious is not obvious, a case report. J Med Case Rep. 2007;1:13.
Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia: recognition, treatment, and prevention: the seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:311–37.
Wester JP, Haas FJ, Biesma DH, Leusink JA, Veth G. Thrombosis and hemorrhage in heparin-induced thrombocytopenia in seriously ill patients. Intensive Care Med. 2004;30:1927–34.
Bertoglio S, Solari N, Meszaros P, Vassallo F, Bonvento M, Pastorino S, Bruzzi P. Efficacy of normal saline versus heparinized saline solution for locking catheters of totally implantable long-term central vascular access devices in adult cancer patients. Cancer Nurs. 2012;35:E35-42.
Alzetani A, Vohra HA, Patel RL. Can we rely on arterial line sampling in performing activated plasma thromboplastin time after cardiac surgery? Eur J Anaesthesiol. 2004;21:384–8.
Heap MJ, Ridley SA, Hodson K, Martos FJ. Are coagulation studies on blood sampled from arterial lines valid? Anaesthesia. 1997;52:640–5.
Hook ML, Reuling J, Luettgen ML, Norris SO, Elsesser CC, Leonard MK. Comparison of the patency of arterial lines maintained with heparinized and nonheparinized infusions. The Cardiovascular Intensive Care Unit Nursing Research Committee of St. Luke’s Hospital. Heart Lung. 1987;16:693–9.
Kulkarni M, Elsner C, Ouellet D, Zeldin R. Heparinized saline versus normal saline in maintaining patency of the radial artery catheter. Can J Surg. 1994;37:37–42.
Tuncali BE, Kuvaki B, Tuncali B, Capar E. A comparison of the efficacy of heparinized and nonheparinized solutions for maintenance of perioperative radial arterial catheter patency and subsequent occlusion. Anesth Analg. 2005;100:1117–21.
Tru Wave with VAPM system. Edwards Lifesciences Corporation. 2020. https://www.edwards.com/devices/pressure-monitoring/closed-blood-sampling. Accessed 11 Dec 2020.
Medi-quick-pulse. ME-ACS223, TERUMO Co. 2020. https://www.terumo.co.jp/medical/equipment/me68.html. Accessed 11 Dec 2020.
McGhee BH, Bridges EJ. Monitoring arterial blood pressure: what you may not know. Crit Care Nurse. 2002;22:60–4 (66–70, 73 passim).
Schoenfeld D. The asymptotic properties of nonparametric tests for comparing survival distributions. Biometrika. 1981;68:316–9.
Del Cotillo M, Grané N, Llavoré M, Quintana S. Heparinized solution vs. saline solution in the maintenance of arterial catheters: a double blind randomized clinical trial. Intensive Care Med. 2008;34:339–43.
Kordzadeh A, Austin T, Panayiotopoulos Y. Efficacy of normal saline in the maintenance of the arterial lines in comparison to heparin flush: a comprehensive review of the literature. J Vasc Access. 2014;15:123–7.
Hall KF, Bennetts TM, Whitta RK, Welman L, Rawlins P. Effect of heparin in arterial line flushing solutions on platelet count: a randomised double-blind study. Crit Care Resusc. 2006;8:294–6.
Whitta RK, Hall KF, Bennetts TM, Welman L, Rawlins P. Comparison of normal or heparinised saline flushing on function of arterial lines. Crit Care Resusc. 2006;8:205–8.
Randolph AG, Cook DJ, Gonzales CA, Andrew M. Benefit of heparin in peripheral venous and arterial catheters: systematic review and meta-analysis of randomised controlled trials. BMJ. 1998;316:969–75.
Arterial catheter complications and management problems: observations from AACN’s Thunder Project. Crit Care Nurs Clin N Am. 1993;5:557–62.
Hoste EA, Roels NR, Decruyenaere JM, Colardyn FA. Significant increase of activated partial thromboplastin time by heparinization of the radial artery catheter flush solution with a closed arterial catheter system. Crit Care Med. 2002;30:1030–4.
Acknowledgements
We thank the medical staff of the Anaesthesiology Department, all nurses of the operating room, and all nurses of surgical intensive care unit at Nagoya University Hospital for their assistance.
Funding
Support was provided solely from institutional and/or departmental sources, and this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. TT, MA, TI, and YK helped with data collection, measurement, analysis, and interpretation. All authors are responsible for writing the paper and for its contents. EK, MK, YM, and AF are responsible for the treatment that the nurses carried out. YM and TI are responsible for the double-blind drug preparation performed by the pharmacists.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Tamura, T., Kobayashi, E., Kawaguchi, M. et al. Comparison between the effects of normal saline with and without heparin for the prevention and management of arterial catheter occlusion: a triple-blinded randomized trial. J Anesth 35, 536–542 (2021). https://doi.org/10.1007/s00540-021-02949-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02949-1