Abstract
Purpose
Hyperglycemia has been associated with postoperative morbidity in patients who undergo cardiac surgery. However, it remains unclear whether the duration of hyperglycemia is as important as its magnitude in the development of postoperative end-organ dysfunction (PEOD). This retrospective study investigated the hypothesis that the intraoperative blood glucose (BG) exposure index (GE index), calculated by the product of the magnitude and duration of BG concentration ≥ 180 mg/dL, which is an integration of the severity and duration of hyperglycemia, is associated with the incidence of PEOD in patients undergoing cardiac surgery with cardiopulmonary bypass.
Methods
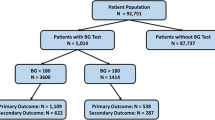
The primary outcome in this study was PEOD within 72 h of surgery, which was defined as a composite of postoperative acute kidney injury, delirium, myocardial injury, and prolonged mechanical ventilation. The GE index (the magnitude of BG concentration deviation ≥ 180 mg/dL \(\times\) duration of BG concentration ≥ 180 mg/dL) of each patient was calculated based on the intraoperative BG concentration. The relationship between the GE index and the primary outcome was examined via logistic regression model with adjustment for potential confounders.
Results
Within 72 h of surgery, 301 patients (54.5%) developed PEOD. PEOD was more common in patients with greater GE index quartiles (first versus third quartile; adjusted odds ratio, 5.65, 95% confidence interval (95% CI), 2.94–10.90; P < 0.001; first versus forth quartile, adjusted odds ratio, 20.80; 95% CI, 8.01–54.00; P < 0.001).
Conclusion
In patients undergoing cardiac surgery with cardiopulmonary bypass, the GE index was an independent predictor of PEOD.


Similar content being viewed by others
Change history
04 December 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00540-021-03029-0
References
Prondzinsky R, Knüpfer A, Lopponow H, Redling F, Lehmann DW, Stabenow I, Witthaut R, Unverzagt S, Radke J, Zerkowski HR, Werdan K. Surgical trauma affects the proinflammatory status after cardiac surgery to a higher degree than cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2005;129:760–6.
Laffey JG, Boylan JF, Cheng DC. The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiology. 2002;97:215–52.
Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Cheng DC, Crowther M, Dupuis JY, Fremes SE, Kent B, Laflamme C, Lamy A, Legare JF, Mazer CD, McCluskey SA, Rubens FD, Sawchuk C, Beattie WS. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation. 2009;119:495–502.
O’Neal JB, Shaw AD, Billings FT 4th. Acute kidney injury following cardiac surgery: current understanding and future directions. Crit Care. 2016. https://doi.org/10.1186/s13054-016-1352-z.
Goren O, Matot I. Perioperative acute kidney injury. Br J Anaesth. 2015. https://doi.org/10.1093/bja/aev380.
Kazmierski J, Kowman M, Banach M, Fendler W, Okonski P, Banys A, Jaszewski R, Rysz J, Mikhailidis DP, Sobow T, Kloszewska I. Incidence and predictors of delirium after cardiac surgery: results from The IPDACS Study. J Psychosom Res. 2010;69:179–85.
Thielmann M, Sharma V, Al-Attar N, Bulluck H, Bisleri G, Bunge J, Czerny M, Ferdinandy P, Frey UH, Heusch G, Holfeld J, Kleinbongard P, Kunst G, Lang I, Lentini S, Madonna R, Meybohm P, Muneretto C, Obadia JF, Perrino C, Prunier F, Sluijter JP, Van Laake LW, Sousa-Uva M, Hausenloy DJ. ESC Joint Working Groups on Cardiovascular Surgery and the Cellular Biology of the Heart Positin Paper: perioperative myocardial injury and infarction in patients undergoing coronary artery bypass graft surgery. Eur Heart J. 2017;38:2392–407.
LaPar DJ, Gillen JR, Crosby IK, Sawyer RG, Lau CL, Kron IL, Ailawadi G. Predictors of operative mortality in cardiac surgical patients with prolonged intensive care unit duration. J Am Coll Surg. 2013;216:1116–23.
Dardashti A, Ederoth P, Algotsson L, Brondén B, Bjursten H. Incidence, dynamics, and prognostic value of acute kidney injury for death after cardiac surgery. J Thorac Cardiovasc Surg. 2014;147:800–7.
Zakkar M, Bruno VD, Guida G, Angelini G, Chivasso P, Suleiman MS, Bryan AJ, Ascione R. Postoperative acute kidney injury defined by RIFLE criteria predicts early health outcome and long-term survival in patients undergoing redo coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2016;152:235–42.
Flu W-J, Schouten O, van Kuijk J-P, Poldermans D. Perioperative cardiac damage in vascular surgery patients. Eur J Vasc Endovasc Surg. 2010;40:1–8.
Galindo RJ, Fayfman M, Umpierrez GE. Perioperative management of hyperglycemia and diabetes in cardiac surgery patients. Endocrinol Metab Clin North Am. 2018;47:203–22.
Xiu F, Stanojcic M, Li D, Jeschke MG. Stress hyperglycemia, insulin treatment, and innate immune cells. Int J Endocrinol. 2014. https://doi.org/10.1155/2014/486403.
Tsai LL, Jensen HA, Thourani VH. Intensive Glycemic Control in Cardiac Surgery. Curr Diab Rep. 2016. https://doi.org/10.1007/s11892-016-0719-5.
Dungan KM, Braithwaite SS, Presiser JC. Stress hyperglycaemia. Lancet. 2009;373:1798–807.
Luc K, Schramm-Luc A, Guzik TJ, Mikolajczyk TP. Oxidative stress and inflammatory markers in prediabetes and diabetes. J Physiol Pharmacol. 2019. https://doi.org/10.26402/jpp.2019.6.01.
Quan XJ, Liang CL, Sun MZ, Zhang L, Li XL. Overexpression of steroid receptor coactivators alleviates hyperglycemia-induced endothelial cell injury in rats through activating the PI3K/Akt pathway. Acta Pharmacol Sin. 2019;40:648–57.
Kyle UG, Coss Bu JA, Kennedy CE, Jefferson LS. Organ dysfunction is associated with hyperglycemia in critically ill children. Intensive Care Med. 2010;36:312–20.
Lipshutz AKM, Gropper MA. Perioperative glycemic control: an evidence-based review. Anesthesiology. 2009;110(2):408–21.
Navaratnarajah M, Rea R, Evans R, Gibson F, Antoniades C, Keiralla A, Demosthenous M, Kassimis G, Krasopoulos G. Effect of glycaemic control on complications following cardiac surgery: literature review. J Cardiothorac Surg. 2018. https://doi.org/10.1186/s13019-018-0700-2.
Lazar HL, McDonnell M, Chipkin SR, Furnary AP, Engelman RM, Sadhu AR, Bridges CR, Haan CK, Svedjeholm R, Taegtmeyer H, Shemin RJ, Society of Thoracic Surgeons Blood Glucose Guideline Task Force. The Society of Thoracic Surgeons Practice Guideline Series: blood glucose management during adult cardiac surgery. Ann Thorac Surg. 2009;87(2):663–9.
Duncan AE, Abd-Elsayed A, Maheshwari A, Xu M, Soltesz E, Koch CG. Role of intraoperative and postoperative blood glucose concentration in predicting outcomes after cardiac surgery. Anesthesiology. 2010;112:860–71.
Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology. 2006;105:244–52.
Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, Devries JH. Glucose variability is associated with intensive care unit mortality. Crit Care Med. 2010;38:838–42.
Nam K, Jeon Y, Kim WH, Jung DE, Kwon SM, Kang P, Cho YJ, Kim TK. Intraoperative glucose variability, but not average glucose concentration, may be a risk factor for acute kidney injury after cardiac surgery: a retrospective study. Can J Anaesth. 2019;66:921–33.
Marsillio JE, Asaro LA, Srinivasan V, Wypij D, Sorce LR, Agus MSD, Nadkarni VM, Heart And Lung Failure-Pediatric Insulin Titration (HALF-PRINT) Study Investigators. outcomes associated with multiple organ dysfunction syndrome in critically ill children with hyperglycemia. Pediatr Crit Care Med. 2019;20:1147–56.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–84.
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–64.
Ramsay J, Shernan S, Fitch J, Finnegan P, Todaro T, Filloon T, Nussmeier NA. Increased creatine kinase MB level predicts postoperative mortality after cardiac surgery independent of new Q waves. J Thorac Cardiovasc Surg. 2005;129:300–6.
Légaré JF, Hirsch GM, Buth KJ, MacDougall C, Sullivan JA. Preoperative prediction of prolonged mechanical ventilation following coronary artery bypass grafting. Eur J Cardiothorac Surg. 2001;20:930–6.
Nashef SAM, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, Lockowandt U. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–44.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Karimolla HT. The choice of methods in determining the optimal cut-off value for quantitative diagnostic test evaluation. Stat Methods Med Res. 2018;27:2374–83.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Jang MS, Nam JS, Jo JY, Kang CH, Ryu SA, Lee EH, Choi IC. The relationship of preoperative estimated glomerular filtration rate and outcomes after cardiovascular surgery in patients with normal serum creatinine: a retrospective cohort study. BMC Anesthesiol. 2019. https://doi.org/10.1186/s12871-019-0763-1.
Cywinski JB, Mascha EJ, Kurz A, Sessler DI. Estimated glomerular filtration rate better predicts 30-day mortality after non-cardiac surgery than serum creatinine: a retrospective analysis of 92,888 patients. Can J Anaesth. 2015;62:745–52.
Totonchi Z, Baazm F, Chitsazan M, Seifi S, Chitsazan M. Predictors of prolonged ventilation after open heart surgery. J Cardiovasc Thorac Res. 2014;6:211–6.
Whitten CW, Hill GE, Ivy R, Lipton JM. Does the duration of cardiopulmonary bypass or aortic cross-clamp, in the absence of blood and/or blood product administration, influence the IL-6 response to cardiac surgery? Anesth Analg. 1998;86:28–33.
Rashid N, Agarwal S, Jawed S, Yasser A, Altahmody K. Impact of cariopulmonary bypass time on postoperative duration of mechanical ventilation in patients undergoing cardiovascular surgeries: a systemic review and regression of metadata. Cureus. 2019. https://doi.org/10.7759/cureus.6088.
Girish G, Agarwal S, Satsangi DK, Tempe D, Dutta N, Pratap H. Glycemic control in cardiac surgery: rationale and current evidence. Ann Card Anaesth. 2014;17:222–8.
Wang J, Yue X, Meng C, Wang Z, Jin X, Cui X, Yang J, Shan C, Gao Z, Yang Y, Li J, Chang B, Chang B. Acute hyperglycemia may induce renal tubular injury through mitophagy inhibition. Front Endocrinol. 2020. https://doi.org/10.3389/fendo.2020.536213.
Yates AR, Dyke PCD, Taeed R, Hoffman TM, Hayes J, Feltes TF, Cua CL. Hyperglycemia is a marker for poor outcome in the postoperative pediatric cardiac patient. Pediatr Crit Care Med. 2006;7:351–5.
Falcao G, Ulate K, Kouzekanani K, Bielefeld MR, Morales JM, Rotta AT. Impact of postoperative hyperglycemia following surgical repair of congenital cardiac defects. Pediatr Cardiol. 2008;29:628–36.
van der Horst ICC, Nijsten MWN, Vogelzang M, Zijlstra F. Persistent hyperglycemia is an independent predictor of outcome in acute myocardial infarction. Cardiovasc Diabetol. 2007. https://doi.org/10.1186/1475-2840-6-2.
Wu TY, Putaala J, Sharma G, Strbian D, Tatlisumak T, Davis SM, Meretoja A. Persistent hyperglycemia is associated with increased mortality after intracerebral hemorrhage. J Am Heart Assoc. 2017. https://doi.org/10.1161/JAHA.117.005760.
Yatabe T, Yamazaki R, Kitagawa H, Okabayashi T, Yamashita K, Hanazaki K, Yokoyama M. The evaluation of the ability of closed-loop glycemic control device to maintain the blood glucose concentration in intensive care unit patients. Crit Care Med. 2011;39:575–8.
Wettstein RB, Shelledy DC, Peters JI. Delivered oxygen concentration using low-flow and high-flow nasal cannulas. Respir Care. 2005;50:604–9.
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–52.
Vincent JL, Moreno R, Takala J, Willatts S, de Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10.
Gusmao-Flores D, Salluh JIF, Chalhub RÁ, Quarantini LC. The confusion assessment method for intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. 2012. https://doi.org/10.1186/cc11407.
Acknowledgements
The authors would like to thank Dr. Satoshi Kimura (Department of Anesthesiology and Resuscitology, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan) for his support in the statistical analyses. The authors declare that we are expressing our gratitude here in pre-agreement with him.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised as affiliation 2 was not tagged to corresponding author and affiliations are correctly tagged in this version.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Matsumoto, S., Omiya, H., Fujinaka, W. et al. Association between intraoperative hyperglycemia and postoperative end-organ dysfunctions after cardiac surgery: a retrospective observational study. J Anesth 36, 174–184 (2022). https://doi.org/10.1007/s00540-021-03024-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-03024-5