Abstract
Purpose
Three-dimensional printing (3DP), or additive manufacturing, is an emergent fabrication technology for surgical devices. As a production method, 3DP enables physical realisation of surgical implants from geometrically complex digital-models in computer-aided design. Spine surgery has been an innovative adopter of 3DP technology for both patient-specific (PS) and market-available ‘Off-The-Shelf’ (OTS) implants. The present study assessed clinical evidence for efficacy and safety of both PS and OTS 3DP spinal implants through review of the published literature. The aim was to evaluate the clinical utility of 3DP devices for spinal surgery.
Methods
A systematic literature review of peer-reviewed papers featured on online medical databases evidencing the application of 3DP (PS and OTS) surgical spine implants was conducted in accordance with PRISMA guidelines.
Results
Twenty-two peer-reviewed articles and one book-chapter were eligible for systematic review. The published literature was limited to case reports and case series, with a predominant focus on PS designs fabricated from titanium alloys for surgical reconstruction in cases where neoplasia, infection, trauma or degenerative processes of the spine have precipitated significant anatomical complexity.
Conclusion
PS and 3DP OTS surgical implants have demonstrated considerable utility for the surgical management of complex spine pathology. The reviewed literature indicated that 3DP spinal implants have also been used safely, with positive surgeon- and patient-reported outcomes. However, these conclusions are tentative as the follow-up periods are still relatively short and the number of high-powered studies was limited. Single case and small case series reporting would benefit greatly from more standardised reporting of clinical, radiographic and biomechanical outcomes.
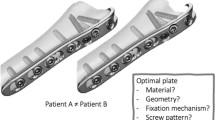
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Change history
26 May 2020
Unfortunately, 3rd author’s first name was incorrectly published in the original publication. The complete correct name is given below,
References
Ventola CL (2014) Medical applications for 3D printing: current and projected uses. Pharm Ther 39:704
Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM (2014) Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. In: ACS Publications
Hull CW (1986) Apparatus for production of three-dimensional objects by stereolithography. In: UVP Inc, San Gabriel, California, USA
Martelli N, Serrano C, van den Brink H, Pineau J, Prognon P, Borget I, El Batti S (2016) Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery 159:1485–1500. https://doi.org/10.1016/j.surg.2015.12.017
Tack P, Victor J, Gemmel P, Annemans L (2016) 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online 15:115. https://doi.org/10.1186/s12938-016-0236-4
Malik HH, Darwood ARJ, Shaunak S, Kulatilake P, El-Hilly AA, Mulki O, Baskaradas A (2015) Three-dimensional printing in surgery: a review of current surgical applications. J Surg Res 199:512–522. https://doi.org/10.1016/j.jss.2015.06.051
Wilcox B, Mobbs RJ, Wu AM, Phan K (2017) Systematic review of 3D printing in spinal surgery: the current state of play. J Spine Surg 3:433–443. https://doi.org/10.21037/jss.2017.09.01
Carette S, Fehlings MG (2005) Cervical radiculopathy. N Engl J Med 353:392–399. https://doi.org/10.1056/NEJMcp043887
Tetreault L, Goldstein CL, Arnold P, Harrop J, Hilibrand A, Nouri A, Fehlings MG (2015) Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery 77:S51–S67
Karadimas KS, Erwin MW, Ely GC, Dettori RJ, Fehlings GM (2013) Pathophysiology and natural history of cervical spondylotic myelopathy. Spine 38:S21–S36. https://doi.org/10.1097/BRS.0b013e3182a7f2c3
Baptiste DC, Fehlings MG (2006) Pathophysiology of cervical myelopathy. Spine J 6:190S. https://doi.org/10.1016/j.spinee.2006.04.024
Roh JS, Teng AL, Yoo JU, Davis J, Furey C, Bohlman HH (2005) Degenerative disorders of the lumbar and cervical spine. Orthop Clin 36:255–262
Mobbs RJ, Loganathan A, Yeung V, Rao PJ (2013) Indications for anterior lumbar interbody fusion. Orthop Surg 5:153–163
Tracy JA, Bartleson JD (2010) Cervical spondylotic myelopathy: the neurologist 16:176–187
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1:2
Holly LT, Schwender JD, Rouben DP, Foley KT (2006) Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus 20:1–5
Choy WJ, Parr WCH, Phan K, Walsh WR, Mobbs RJ (2018) 3-dimensional printing for anterior cervical surgery: a review. J Spine Surg 4:757–769. https://doi.org/10.21037/jss.2018.12.01
Wang T, Wang H, Liu S, An H-D, Liu H, Ding W-Y (2016) Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion in multilevel cervical spondylotic myelopathy: a meta-analysis. Medicine 95:e5437. https://doi.org/10.1097/MD.0000000000005437
Wen Z-q, Du J-y, Ling Z-h, Xu H-d, Lin X-j (2015) Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion in the treatment of multilevel cervical spondylotic myelopathy: systematic review and a meta-analysis. Ther Clin Risk Manag 11:161
Chong E, Pelletier MH, Mobbs RJ, Walsh WR (2015) The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord 16:99. https://doi.org/10.1186/s12891-015-0546-x
Phan K, Mobbs RJ (2016) Evolution of design of interbody cages for anterior lumbar interbody fusion. Orthop Surg 8:270–277
Phan K, Tian DH, Cao C, Black D, Yan TD (2015) Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg 4:112–122. https://doi.org/10.3978/j.issn.2225-319X.2015.02.04
Phan K, Mobbs RJ (2015) Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg 1:19–27. https://doi.org/10.3978/j.issn.2414-469X.2015.06.01
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Xu NMD, Wei FMD, Liu XMD, Jiang LMD, Cai HMD, Li ZMD, Yu MMD, Wu FMD, Liu ZMD (2016) Reconstruction of the upper cervical spine using a personalized 3D-printed vertebral body in an adolescent with Ewing Sarcoma. Spine 41:E50–E54
Tang HP, Zhao P, Xiang CS, Liu N, Jia L (2018) Ti-6Al-4 V orthopedic implants made by selective electron beam melting. In: Froes FH, Qian M (eds) Titanium in medical and dental applications. Woodhead Publishing, Cambridge, pp 239–249
Amelot A, Colman M, Loret JE (2018) Vertebral body replacement using patient-specific three-dimensional-printed polymer implants in cervical spondylotic myelopathy: an encouraging preliminary report. Spine J 18:892–899
Mokawem M, Katzouraki G, Harman CL, Lee R (2019) Lumbar interbody fusion rates with 3D-printed lamellar titanium cages using a silicate-substituted calcium phosphate bone graft. J Clin Neurosci. https://doi.org/10.1016/j.jocn.2019.07.011
Chung SS, Lee KJ, Kwon YB, Kang KC (2017) Characteristics and efficacy of a new 3-dimensional printed mesh structure titanium alloy spacer for posterior lumbar interbody fusion. Orthopedics 40:e880–e885
Thayaparan GK, Owbridge MG, Thompson RG, D’Urso PS (2019) Designing patient-specific solutions using biomodelling and 3D-printing for revision lumbar spine surgery. Eur Spine J 28(2):18–24
Wei R, Guo W, Yang R, Tang X, Yang Y, Ji T, Liang H (2019) Reconstruction of the pelvic ring after total en bloc sacrectomy using a 3D-printed sacral endoprosthesis with re-establishment of spinopelvic stability: a retrospective comparative study. Bone Joint J 101-B:880–888
Kim D, Lim J-Y, Shim K-W, Han JW, Yi S, Yoon DH, Kim KN, Ha Y, Ji GY, Shin DA (2017) Sacral reconstruction with a 3D-printed implant after hemisacrectomy in a patient with sacral osteosarcoma: 1-year follow-up result. Yonsei Med J 58:453–457
Wei R, Guo W, Ji T, Zhang Y, Liang H (2017) One-step reconstruction with a 3D-printed, custom-made prosthesis after total en bloc sacrectomy: a technical note. Eur Spine J 26:1902–1909. https://doi.org/10.1007/s00586-016-4871-z
Mobbs RJ, Coughlan M, Thompson R, Sutterlin CE, Phan K (2017) The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: case report. J Neurosurg: Spine 26:513–518
Girolami M, Boriani S, Bandiera S, Barbanti-Brodano G, Ghermandi R, Terzi S, Tedesco G, Evangelisti G, Pipola V, Gasbarrini A (2018) Biomimetic 3D-printed custom-made prosthesis for anterior column reconstruction in the thoracolumbar spine: a tailored option following en bloc resection for spinal tumors: preliminary results on a case-series of 13 patients. Eur Spine J 27:3073–3083
Mobbs RJ, Choy WJ, Wilson P, McEvoy A, Phan K, Parr WCH (2018) L5 en-bloc vertebrectomy with customized reconstructive implant: comparison of patient-specific versus off-the-shelf implant. World Neurosurg 112:94–100
Siu TL, Rogers JM, Lin K, Thompson R, Owbridge M (2018) Custom-made titanium 3-dimensional printed interbody cages for treatment of osteoporotic fracture-related spinal deformity. World Neurosurg 111:1–5
Mobbs RJ, Parr WCH, Choy WJ, McEvoy A, Walsh WR, Phan K (2019) Anterior lumbar interbody fusion using a personalized approach: is custom the future of implants for anterior lumbar interbody fusion surgery? World Neurosurg. https://doi.org/10.1016/j.wneu.2018.12.144
Chung KS, Shin DA, Kim KN, Ha Y, Yoon DH, Yi S (2019) Vertebral reconstruction with customized 3-dimensional-printed spine implant replacing large vertebral defect with 3-year follow-up. World Neurosurg 126:90–95
Choy WJ, Mobbs RJ, Wilcox B, Phan S, Phan K, Sutterlin CE (2017) Reconstruction of thoracic spine using a personalized 3D-printed vertebral body in adolescent with T9 primary bone tumor. World Neurosurg 105:1032.e1013–1032.e1017. https://doi.org/10.1016/j.wneu.2017.05.133
Phan K, Sgro A, Maharaj MM, D’Urso P, Mobbs RJ (2016) Application of a 3D custom printed patient specific spinal implant for C1/2 arthrodesis. J Spine Surg 2:314–318. https://doi.org/10.21037/jss.2016.12.06
Spetzger U, Frasca M, König SA (2016) Surgical planning, manufacturing and implantation of an individualized cervical fusion titanium cage using patient-specific data. Eur Spine J 25:2239–2246. https://doi.org/10.1007/s00586-016-4473-9
Li X, Wang Y, Zhao Y, Liu J, Xiao S, Mao K (2017) Multilevel 3D printing implant for reconstructing cervical spine with metastatic papillary thyroid carcinoma. Spine 42:E1326–E1330. https://doi.org/10.1097/BRS.0000000000002229
Lu T, Liu C, Yang B, Liu J, Zhang F, Wang D, Li H, He X (2017) Single-level anterior cervical corpectomy and fusion using a new 3D-printed anatomy-adaptive titanium mesh cage for treatment of cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: a retrospective case series study. Med Sci Monit: Intern Med J Exp Clin Res 23:3105–3114
Thayaparan GK, Owbridge MG, Thompson RG, D’Urso PS (2018) Designing patient-specific 3D printed devices for posterior atlantoaxial transarticular fixation surgery. J Clin Neurosci 56:192–198. https://doi.org/10.1016/j.jocn.2018.06.038
He S, Yang X, Yang J, Ye C, Liu W, Wei H, Xiao J (2019) Customized “Whole-Cervical-Vertebral-Body” reconstruction after modified subtotal spondylectomy of C2–C7 spinal tumor via piezoelectric surgery. Oper Neurosurg. https://doi.org/10.1093/ons/opz077
Zhang Y-W, Deng L, Zhang X-X, Yu X-L, Ai Z-Z, Mei Y-X, He F, Yu H, Zhang L, Xiao X, Xiao Y, Chen X, Zhang S-L, Ge H-Y, Dong X-P (2019) Three-dimensional printing-assisted cervical anterior bilateral pedicle screw fixation of artificial vertebral body for cervical tuberculosis. World Neurosurg 127:25–30. https://doi.org/10.1016/j.wneu.2019.03.238
Rao PJ, Pelletier MH, Walsh WR, Mobbs RJ (2014) Spine interbody implants: material selection and modification, functionalization and bioactivation of surfaces to improve osseointegration. Orthop Surg 6:81–89
Tan XP, Tan YJ, Chow CSL, Tor SB, Yeong WY (2017) Metallic powder-bed based 3D printing of cellular scaffolds for orthopaedic implants: a state-of-the-art review on manufacturing, topological design, mechanical properties and biocompatibility. Mater Sci Eng, C 76:1328–1343. https://doi.org/10.1016/j.msec.2017.02.094
Sidambe A (2014) Biocompatibility of advanced manufactured titanium implants: a review. Materials 7:8168–8188
Palmquist A, Snis A, Emanuelsson L, Browne M, Thomsen P (2013) Long-term biocompatibility and osseointegration of electron beam melted, free-form–fabricated solid and porous titanium alloy: experimental studies in sheep. J Biomater Appl 27:1003–1016. https://doi.org/10.1177/0731684411431857
Lin X, Xiao X, Wang Y, Gu C, Wang C, Chen J, Liu H, Luo J, Li T, Wang D, Fan S (2018) Biocompatibility of bespoke 3D-printed titanium alloy plates for treating acetabular fractures. Biomed Res Int 2018:2053486. https://doi.org/10.1155/2018/2053486
Wang H, Zhao B, Liu C, Wang C, Tan X, Hu M (2016) A comparison of biocompatibility of a Titanium alloy fabricated by electron beam melting and selective laser melting. PLoS ONE 11:e0158513. https://doi.org/10.1371/journal.pone.0158513
Nawaz F, Wall BM (2007) Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome: suspected association with titanium bioprosthesis. Am J Med Sci 334:215–218. https://doi.org/10.1097/MAJ.0b013e318141f723
FDA (2017) Technical considerations for additive manufactured medical devices. In: U.S. Food & Drug Administration (ed). U.S. Department of Health and Human Services
Shah RR, Mohammed S, Saifuddin A, Taylor BA (2003) Comparison of plain radiographs with CT scan to evaluate interbody fusion following the use of titanium interbody cages and transpedicular instrumentation. Eur Spine J 12:378–385. https://doi.org/10.1007/s00586-002-0517-4
Cook SD (2004) Comparison of methods for determining the presence and extent of anterior lumbar interbody fusion. Spine 29:1118
Williams AL, Gornet MF, Burkus JK (2005) CT evaluation of lumbar interbody fusion: current concepts. Am J Neuroradiol: AJNR 26:2057–2066
World Health Organization: International Clinical Trials Registry Platform (2018) Lumbar fusion with next spine 3D-printed titanium interbody cages. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NCT03647501
Suh PB, Puttlitz C, Lewis C, Bal BS, McGilvray K (2017) The effect of cervical interbody cage morphology, material composition, and substrate density on cage subsidence. J Am Acad Orthop Surg 25:160–168
Chatham LS, Patel VV, Yakacki CM, Dana Carpenter R (2017) Interbody spacer material properties and design conformity for reducing subsidence during lumbar interbody fusion. J Biomech Eng 139:0510051–0510058. https://doi.org/10.1115/1.4036312
de Beer N, Scheffer C (2012) Reducing subsidence risk by using rapid manufactured patient-specific intervertebral disc implants. Spine J 12:1060–1066
Fengbin Y, Jinhao M, Xinyuan L, Xinwei W, Yu C, Deyu C (2013) Evaluation of a new type of titanium mesh cage versus the traditional titanium mesh cage for single-level, anterior cervical corpectomy and fusion. Eur Spine J 22:2891–2896. https://doi.org/10.1007/s00586-013-2976-1
Arts MP, Peul WC (2008) Vertebral body replacement systems with expandable cages in the treatment of various spinal pathologies: a prospectively followed case series of 60 patients. Neurosurgery 63:537–545. https://doi.org/10.1227/01.NEU.0000325260.00628.DC
Lau D, Song Y, Guan Z, La Marca F, Park P (2013) Radiological outcomes of static vs expandable titanium cages after corpectomy. Neurosurgery 72:529–539. https://doi.org/10.1227/NEU.0b013e318282a558
Chen Y, Chen D, Guo Y, Wang X, Lu X, He Z, Yuan W (2008) Subsidence of titanium mesh cage. J Spinal Disord Tech 21:489–492. https://doi.org/10.1097/BSD.0b013e318158de22
Wang X, Xu S, Zhou S, Xu W, Leary M, Choong P, Qian M, Brandt M, Xie YM (2016) Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: a review. Biomater 83:127–141. https://doi.org/10.1016/j.biomaterials.2016.01.012
Karageorgiou V, Kaplan D (2005) Porosity of 3D biomaterial scaffolds and osteogenesis. Biomater 26:5474–5491. https://doi.org/10.1016/j.biomaterials.2005.02.002
Sing SL, An J, Yeong WY, Wiria FE (2016) Laser and electron-beam powder-bed additive manufacturing of metallic implants: a review on processes, materials and designs. J Orthop Res 34:369–385. https://doi.org/10.1002/jor.23075
Walsh WR, Pelletier MH, Wang T, Lovric V, Morberg P, Mobbs RJ (2019) Does implantation site influence bone ingrowth into 3D printed porous implants? Spine J. https://doi.org/10.1016/j.spinee.2019.06.020
Burkus JK, Foley K, Haid R, LeHuec J-C (2001) Surgical interbody research group–radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus 10:1–9. https://doi.org/10.3171/foc.2001.10.4.12
Author information
Authors and Affiliations
Contributions
(I) Study conception and design were contributed by JL Burnard, WCH Parr, RJ Mobbs; (II) Administrative Support was contributed by RJ Mobbs, WCH Parr, WJ Choy; (III) Provision of Study Materials was contributed by WCH Parr, RJ Mobbs; (IV) Data Analysis/Interpretation were contributed by JL Burnard, WCH Parr, RJ Mobbs; (V) Manuscript Writing was contributed by JL Burnard, WCH Parr; (VI) Critical Revision of Manuscript was contributed by WCH Parr, RJ Mobbs, WR Walsh.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Burnard, J.L., Parr, W.C.H., Choy, W.J. et al. 3D-printed spine surgery implants: a systematic review of the efficacy and clinical safety profile of patient-specific and off-the-shelf devices. Eur Spine J 29, 1248–1260 (2020). https://doi.org/10.1007/s00586-019-06236-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06236-2