Abstract
Purpose
This meta-analysis aims to compare the complication rates of discectomy/microdiscectomy (OD/MD), microendoscopic discectomy (MED), percutaneous endoscopic lumbar discectomy (PELD), percutaneous laser disc decompression (PLDD), and tubular discectomy for symptomatic lumbar disc herniation (LDH) using general classification and modified Clavien–Dindo classification (MCDC) schemes.
Methods
We searched three online databases for randomized controlled trials (RCTs) and cohort studies. Overall complication rates and complication rates per the above-mentioned classification schemes were considered as primary outcomes. Risk ratio (RR) and their 95% confidence intervals (CI) were evaluated.
Results
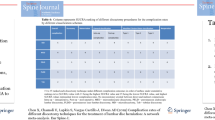
Seventeen RCTs and 20 cohort studies met the eligibility criteria. RCTs reporting OD/MD, MED, PELD, PLDD, and tubular discectomies had overall complication rates of 16.8% and 16.1%, 21.2%, 5.8%, 8.4%, and 25.8%, respectively. Compared with the OD/MD, there was moderate-quality evidence suggesting that PELD had a lower risk of overall complications (RR = 0.52, 95% CI 0.29–0.91) and high-quality evidence suggesting a lower risk of Type I complications per MCDC (RR = 0.37, 95% CI 0.16–0.81). Compared with the OD/MD data from cohort studies, there was low-quality evidence suggesting a higher risk of Type III complications per MCDC (RR = 10.83, 95% CI 1.29–91.18) for MED, higher risk of reherniations (RR = 1.67,95% CI 1.05–2.64) and reoperations (RR = 1.75, 95% CI 1.20–2.55) for PELD, lower risk of overall complication rates (RR = 0.42, 95% CI 0.25–0.70), post-operative complication rates (RR = 0.42, 95% CI 0.25–0.70), Type III complications per MCDC (RR = 0.39, 95% CI 0.22–0.69), reherniations (RR = 0.56, 95% CI 0.33–0.97) and reoperations (RR = 0.39, 95% CI 0.22–0.69) for PLDD.
Conclusions
Compared with the OD/MD, results of this meta-analysis suggest that PELD has a lower risk of overall complications and a lower risk of complications necessitating conservative treatment.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.





Similar content being viewed by others
References
Gibson JN, Cowie JG, Iprenburg M (2012) Transforaminal endoscopic spinal surgery: the future ‘gold standard’ for discectomy? A review. Surgeon 10:290–296. https://doi.org/10.1016/j.surge.2012.05.001
Postacchini F (1999) Management of herniation of the lumbar disc. J Bone Jt Surg Br 81:567–576
Luo X, Pietrobon R, Sun SX, Liu GG, Gey L (2004) Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976) 29:79–86. https://doi.org/10.1097/01.brs.0000105527.13866.0f
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL Jr, Toton JF, North American Spine S (2014) An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14:180–191. https://doi.org/10.1016/j.spinee.2013.08.003
Haines SJ, Jordan N, Boen JR, Nyman JA, Oldridge NB, Lindgren BR (2002) Discectomy strategies for lumbar disc herniation: results of the LAPDOG trial. J Clin Neurosci 9:411–417. https://doi.org/10.1054/jocn.2002.1120
Thomé C, Barth M, Scharf J, Schmiedek P (2005) Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine 2:271–278. https://doi.org/10.3171/spi.2005.2.3.0271
Barrios C, Ahmed M, Arrótegui J, Björnsson A, Gillström P (1990) Microsurgery versus standard removal of the herniated lumbar disc. A 3-year comparison in 150 cases. Acta Orthop Scand 61:399–403
Silverplats K, Lind B, Zoëga B, Halldin K, Gellerstedt M, Brisby H, Rutberg L (2010) Clinical factors of importance for outcome after lumbar disc herniation surgery: long-term follow-up. Eur Spine J 19:1459–1467. https://doi.org/10.1007/s00586-010-1433-7
Virk SS, Diwan A, Phillips FM, Sandhu H, Khan SN (2017) What is the rate of revision discectomies after primary discectomy on a national scale? Clin Orthop Relat Res 475:2752–2762. https://doi.org/10.1007/s11999-017-5467-6
Rasouli MR, Rahimi-Movaghar V, Shokraneh F, Moradi-Lakeh M, Chou R (2014) Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd010328.pub2
Deen HG, Fenton DS, Lamer TJ (2003) Minimally invasive procedures for disorders of the lumbar spine. Mayo Clin Proc 78:1249–1256
Patel N, Singh V (2018) Percutaneous lumbar laser discectomy: literature review and a retrospective analysis of 65 cases. Photomed Laser Surg 36:518–521. https://doi.org/10.1089/pho.2018.4460
Abrishamkar S, Kouchakzadeh M, Mirhosseini A, Tabesh H, Rezvani M, Moayednia A, Ganjeifar B, Mahabadi A, Yousefi E, Kooshki AM (2015) Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J Res Med Sci 20:1133–1137. https://doi.org/10.4103/1735-1995.172979
Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WCH, Schenk B, van den Berg-Huijsmans AA, Koes BW, Arts MA, van Buchem MA, Peul WC (2017) Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: two-year results of a randomised controlled trial. Interv Neuroradiol 23:313–324. https://doi.org/10.1177/1591019917699981
Foley KT, Smith MM, Rampersaud YR (1999) Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 7:e5
Kambin P (1992) Arthroscopic microdiscectomy. Arthroscopy 8:287–295
Alvi MA, Kerezoudis P, Wahood W, Goyal A, Bydon M (2018) Operative approaches for lumbar disc herniation: a systematic review and multiple treatment meta-analysis of conventional and minimally invasive surgeries. World Neurosurg 114(391–407):e392. https://doi.org/10.1016/j.wneu.2018.02.156
Anichini G, Landi A, Caporlingua F, Beer-Furlan A, Brogna C, Delfini R, Passacantilli E (2015) Lumbar endoscopic microdiscectomy: where are we now? An updated literature review focused on clinical outcome, complications, and rate of recurrence. Biomed Res Int 2015:417801. https://doi.org/10.1155/2015/417801
Li X, Chang H, Meng X (2018) Tubular microscopes discectomy versus conventional microdiscectomy for treating lumbar disk herniation: systematic review and meta-analysis. Medicine 97:e9807. https://doi.org/10.1097/MD.0000000000009807
Riesenburger RI, David CA (2006) Lumbar microdiscectomy and microendoscopic discectomy. Minim Invasive Ther Allied Technol 15:267–270. https://doi.org/10.1080/13645700600958432
Clark AJ, Safaee MM, Khan NR, Brown MT, Foley KT (2017) Tubular microdiscectomy: techniques, complication avoidance, and review of the literature. Neurosurg Focus 43:E7. https://doi.org/10.3171/2017.5.FOCUS17202
Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K (2001) Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine (Phila Pa 1976) 26:652–657
Shriver MF, Xie JJ, Tye EY, Rosenbaum BP, Kshettry VR, Benzel EC, Mroz TE (2015) Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurg Focus 39:E6. https://doi.org/10.3171/2015.7.FOCUS15281
Kraemer R, Wild A, Haak H, Herdmann J, Krauspe R, Kraemer J (2003) Classification and management of early complications in open lumbar microdiscectomy. Eur Spine J 12:239–246. https://doi.org/10.1007/s00586-002-0466-y
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Tan WF, Peul WC (2011) Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery 69:135–144. https://doi.org/10.1227/neu.0b013e318214a98c(discussion 144)
Ding ZM, Tao YQ (2017) Clinical outcomes of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy in patients with lumbar disc herniation. J Int Transl Med 5:29–33. https://doi.org/10.11910/2227-6394.2017.05.01.06
Garg B, Nagraja UB, Jayaswal A (2011) Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg 19:30–34
Lebude B, Yadla S, Albert T, Anderson DG, Harrop JS, Hilibrand A, Maltenfort M, Sharan A, Vaccaro AR, Ratliff JK (2010) Defining “complications” in spine surgery: neurosurgery and orthopedic spine surgeons’ survey. J Spinal Disord Tech 23:493–500. https://doi.org/10.1097/BSD.0b013e3181c11f89
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Landriel Ibanez FA, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, Tramontano R, Knezevich F, Carrizo A (2011) A new classification of complications in neurosurgery. World Neurosurg 75:709–715. https://doi.org/10.1016/j.wneu.2010.11.010(discussion 604–711)
Chen X, Chamoli U, Lapkin S, Castillo JV, Diwan AD (2019) Complication rates of different discectomy techniques for the treatment of lumbar disc herniation: a network meta-analysis. Eur Spine J 28:2588–2601. https://doi.org/10.1007/s00586-019-06142-7
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, van Tulder MW (2015) 2015 Updated method guideline for systematic reviews in the cochrane back and neck group. Spine 40:1660–1673. https://doi.org/10.1097/brs.0000000000001061
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analysis. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF (1999) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet 354:1896–1900. https://doi.org/10.1016/s0140-6736(99)04149-5
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015
Franke J, Greiner-Perth R, Boehm H, Mahlfeld K, Grasshoff H, Allam Y, Awiszus F (2009) Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J 18:992–1000. https://doi.org/10.1007/s00586-009-0964-2
Hermantin FU, Peters T, Quartararo L, Kambin P (1999) A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am 81:958–965
Huang TJ, Hsu RW, Li YY, Cheng CC (2005) Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 23:406–411
Hussein M (2016) Minimal incision, multifidus-sparing microendoscopic diskectomy versus conventional microdiskectomy for highly migrated intracanal lumbar disk herniations. J Am Acad Orthop Surg 24:805–813. https://doi.org/10.5435/jaaos-d-15-00588
Hussein M, Abdeldayem A, Mattar MM (2014) Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J 23:1992–1999. https://doi.org/10.1007/s00586-014-3296-9
Mayer HM, Brock M (1993) Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg 78:216–225
Pan L, Zhang P, Yin Q (2014) Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg 12:534–537. https://doi.org/10.1016/j.ijsu.2014.02.015
Pan Z, Ha Y, Yi S, Cao K (2016) Efficacy of transforaminal endoscopic spine system (TESSYS) technique in treating lumbar disc herniation. Med Sci Monit 22:530–539. https://doi.org/10.12659/msm.894870
Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61:545–549. https://doi.org/10.1227/01.NEU.0000280008.72190.15
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 33:931–939. https://doi.org/10.1097/brs.0b013e31816c8af7
Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V (2008) Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery 62:174–181. https://doi.org/10.1227/01.NEU.0000296996.00030.3F
Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L (2010) Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J 19:443–450. https://doi.org/10.1007/s00586-010-1290-4
Ahn SS, Kim SH, Kim DW, Lee BH (2016) Comparison of outcomes of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for young adults: a retrospective matched cohort study. World Neurosurg 86:250–258
Choi KC, Kim JS, Park CK (2016) Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Phys 19:E291–E300
Schizas C, Tsiridis E, Saksena J (2005) Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery 57:357–360 (discussion 357–360)
Bennis S, Scarone P, Lepeintre JF, Aldea S, Gaillard S (2009) Transtubular versus microsurgical approach for single lumbar disc herniation: a prospective study. Eur J Orthop Surg Traumatol 19:535–540
Bhatia PS, Chhabra HS, Mohapatra B, Nanda A, Sangodimath G, Kaul R (2016) Microdiscectomy or tubular discectomy: is any of them a better option for management of lumbar disc prolapse. J Craniovertebral Junct Spine 7:146–152
Cahill KS, Levi AD, Cummock MD, Liao W, Wang MY (2013) A comparison of acute hospital charges after tubular versus open microdiskectomy. World Neurosurg 80:208–212. https://doi.org/10.1016/j.wneu.2012.08.015
Choi YY, Yoon SH, Ha Y, Kim EY, Park HC, Park CO (2006) Posterior microscopic lesionectomy for lumbar disc herniation with tubular retraction using METRx(TM) system. J Korean Neurosurg Soc 40:406–411
German JW, Adamo MA, Hoppenot RG, Blossom JH, Nagle HA (2008) Perioperative results following lumbar discectomy: comparison of minimally invasive discectomy and standard microdiscectomy. Neurosurg Focus 25:E20. https://doi.org/10.3171/FOC/2008/25/8/E20
Hsu HT, Chang SJ, Yang SS, Chai CL (2013) Learning curve of full-endoscopic lumbar discectomy. Eur Spine J 22:727–733
Kim MJ, Lee SH, Jung ES, Son BG, Choi ES, Shin JH, Sung JK, Chi YC (2007) Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol 68:623–631. https://doi.org/10.1016/j.surneu.2006.12.051
Kim SK, Lee SC, Park SW (2018) Trans-sacral epiduroscopic laser decompression versus the microscopic open interlaminar approach for L5-S1 disc herniation. J Spinal Cord Med 43:46–52
Kleinpeter G, Markowitsch MM, Bock F (1995) Percutaneous endoscopic lumbar discectomy: minimally invasive, but perhaps only minimally useful? Surg Neurol 43:534–541
Lau D, Han SJ, Lee JG, Lu DC, Chou D (2011) Minimally invasive compared to open microdiscectomy for lumbar disc herniation. J Clin Neurosci 18:81–84
Lee P, Liu JC, Fessler RG (2011) Perioperative results following open and minimally invasive single-level lumbar discectomy. J Clin Neurosci 18:1667–1670
Liu WG, Wu XT, Guo JH, Zhuang SY, Teng GJ (2010) Long-term outcomes of patients with lumbar disc herniation treated with percutaneous discectomy: comparative study with microendoscopic discectomy. Cardiovasc Interv Radiol 33:780–786
Liu X, Yuan S, Tian Y, Wang L, Gong L, Zheng Y, Li J (2018) Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results. J Neurosurg Spine 28:317–325. https://doi.org/10.3171/2017.6.SPINE172
Nakagawa H, Kamimura M, Uchiyama S, Takahara K, Itsubo T, Miyasaka T (2003) Microendoscopic discectomy (MED) for lumbar disc prolapse. J Clin Neurosci 10:231–235
Tassi GP (2006) Comparison of results of 500 microdiscectomies and 500 percutaneous laser disc decompression procedures for lumbar disc herniation. Photomed Laser Surg 24:694–697
Wu X, Zhuang S, Mao Z, Chen H (2006) Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976) 31:2689–2694. https://doi.org/10.1097/01.brs.0000244615.43199.07
Yoon SM, Ahn SS, Kim KH, Kim YD, Cho JH, Kim DH (2012) Comparative study of the outcomes of percutaneous endoscopic lumbar discectomy and microscopic lumbar discectomy using the tubular retractor system based on the VAS, ODI, and SF-36. Korean J Spine 9:215–222. https://doi.org/10.14245/kjs.2012.9.3.215
Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A (2016) Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta-analysis. Int J Surg 31:86–92. https://doi.org/10.1016/j.ijsu.2016.05.061
Qin R, Liu B, Hao J, Zhou P, Yao Y, Zhang F, Chen X (2018) Percutaneous endoscopic lumbar discectomy versus posterior open lumbar microdiscectomy for the treatment of symptomatic lumbar disc herniation: a systemic review and meta-analysis. World Neurosurg 120:352–362. https://doi.org/10.1016/j.wneu.2018.08.236
Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ (2018) A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: a meta-analysis. Biomed Res Int 2018:9073460. https://doi.org/10.1155/2018/9073460
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW Jr, Atkins D, Meerpohl J, Schunemann HJ (2011) GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias). J Clin Epidemiol 64:407–415. https://doi.org/10.1016/j.jclinepi.2010.07.017
Acknowledgements
The authors would like to thank Mark Donoghoe (Stats Central, UNSW) for his help with developing the database search strategy.
Funding
This work was supported by a Research Training Program scholarship and a University Postgraduate Award from the Australian Government and UNSW to XLC and a Scientia scholarship from UNSW to VASR. A Clinical Travelling Fellowship from the International Society for the Study of the Lumbar Spine (ISSLS) in 2018 further supported this work. JLVC was funded by an unrestricted educational and research donation by Nuvasive Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, X., Chamoli, U., Vargas Castillo, J. et al. Complication rates of different discectomy techniques for symptomatic lumbar disc herniation: a systematic review and meta-analysis. Eur Spine J 29, 1752–1770 (2020). https://doi.org/10.1007/s00586-020-06389-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06389-5