Abstract
Purpose
Highlight risk factors for pseudarthrosis in long-segment spinal fusions, collect the approaches carried to address this complication.
Methods
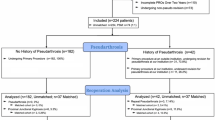
Patients with ASD and fusion of ≥ 4 levels with minimum follow-up (FU) of ≥ 2 years were included. Full-body X-rays were done preoperatively, < 3 months and ≥ 2 years. Oswestry disability index (ODI), Scoliosis Research Society-22 and SF36 assessed pre- and postoperatively. The relationship between demographic, surgical and radiological variables with the development of pseudarthrosis was evaluated.
Results
Out of 524 patients included, 65 patients (12.4%) developed pseudarthrosis and 53 underwent revision surgery. Notably, 88% of pseudarthrosis cases are associated with fusion length (OR = 1.17, 95% CI = 1.05–1.292, p = 0.004), osteotomy requirement (OR = 0.28, 95% CI = 0.09–0.85, p = 0.025), pelvic fixation (OR = 0.34, 95% CI = 0.13–0.88, p = 0.026) and combined approaches (OR = 3.29, 95% CI = 1.09–9.91, p = 0.034). Sagittal alignment is not related to the rate of pseudarthrosis. Health related and quality of life scores were comparable at last FU between patients revised for pseudarthrosis and those that didn’t require revision surgery (ODI = 28% no revision and 30% revision group).
Conclusions
Pseudarthrosis is not related to malalignment, but with the surgical techniques employed for its treatment. Anterior approaches with anterior support decrease the rate by 30%, while long fusions, osteotomies and pelvic fixation increase its rate.


Similar content being viewed by others
References
Mac-Thiong J-M, Transfeldt EE, Mehbod AA et al (2009) Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine (Phila Pa 1976) 34:E519–E527
Schwab F, Patel A, Ungar B et al (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35:2224–2231
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–8
Martin BI, Mirza SK, Comstock BA et al (2007) Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976) 32:382–7
Riouallon G, Bouyer B, Wolff S (2016) Risk of revision surgery for adult idiopathic scoliosis: a survival analysis of 517 cases over 25 years. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 25:2527–2534
How NE, Street JT, Dvorak MF et al (2019) Pseudarthrosis in adult and pediatric spinal deformity surgery: a systematic review of the literature and meta-analysis of incidence, characteristics, and risk factors. Neurosurg Rev 42:319–336
Carreon LY, Djurasovic M, Glassman SD et al (2007) Diagnostic accuracy and reliability of fine-cut CT scans with reconstructions to determine the status of an instrumented posterolateral fusion with surgical exploration as reference standard. Spine (Phila Pa 1976) 32:892–5
Peters MJM, Bastiaenen CHG, Brans BT et al (2019) The diagnostic accuracy of imaging modalities to detect pseudarthrosis after spinal fusion-a systematic review and meta-analysis of the literature. Skeletal Radiol 48:1499–1510
Barton C, Noshchenko A, Patel V et al (2015) Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: a retrospective case-series. Scoliosis 10:30
Smith JS, Shaffrey CI, Ames CP et al (2012) Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 71:862–867
Smith JS, Shaffrey E, Klineberg E et al (2014) Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 21:994–1003
Akazawa T, Kotani T, Sakuma T et al (2013) Rod fracture after long construct fusion for spinal deformity: clinical and radiographic risk factors. J Orthop Sci 18:926–931
Daniels AH, DePasse JM, Durand W et al (2018) Rod fracture after apparently solid radiographic fusion in adult spinal deformity patients. World Neurosurg 117:e530–e537
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99:1661–1672
Werle S, AbuNahleh K, Boehm H (2016) Bone morphogenetic protein 7 and autologous bone graft in revision surgery for non-union after lumbar interbody fusion. Arch Orthop Trauma Surg 136:1041–1049
Merrill RK, Kim JS, Leven DM et al (2017) Multi-rod constructs can prevent rod breakage and pseudarthrosis at the lumbosacral junction in adult spinal deformity. Glob Spine J 7:514–520
Carreon LY, Bratcher KR, Canan CE et al (2013) Differentiating minimum clinically important difference for primary and revision lumbar fusion surgeries. J Neurosurg Spine 18(1):102–106
Sherif S, Arlet V (2020) Revision surgery for non-union in adult spinal deformity. Eur Spine J 29(1):103–115
Boissière L, Bourghli A, Vital J-M et al (2013) The lumbar lordosis index: a new ratio to detect spinal malalignment with a therapeutic impact for sagittal balance correction decisions in adult scoliosis surgery. Eur spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22:1339–1345
Charosky S, Moreno P, Maxy P (2014) Instability and instrumentation failures after a PSO: a finite element analysis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 23:2340–2349
Scheer JK, Tang JA, Deviren V et al (2011) Biomechanical analysis of revision strategies for rod fracture in pedicle subtraction osteotomy. Neurosurgery 69:164–72
Hyun S-J, Lenke LG, Kim Y-C et al (2014) Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 39:1899–904
Barrey C, Perrin G, Michel F et al (2014) Pedicle subtraction osteotomy in the lumbar spine: indications, technical aspects, results and complications. Eur J Orthop Surg Traumatol 24(Suppl 1):S21-30
Enercan M, Ozturk C, Kahraman S et al (2013) Osteotomies/spinal column resections in adult deformity. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(Suppl 2):S254–S264
Richter M, Weidenfeld M, Uckmann FP (2015) Anterior lumbar interbody fusion. Indications, technique, advantages and disadvantages. Der Orthopade 44:154–161
Luca A, Lovi A, Galbusera F et al (2014) Revision surgery after PSO failure with rod breakage: a comparison of different techniques. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 23(Suppl 6):610–615
Phan K, Mobbs RJ (2015) Oblique lumbar interbody fusion for revision of non-union following prior posterior surgery: a case report. Orthop Surg 7:364–367
Hentenaar B, Spoor AB, de Waal MJ et al (2016) Clinical and radiological outcome of minimally invasive posterior lumbar interbody fusion in primary versus revision surgery. J Orthop Surg Res 11:2
Bourghli A, Boissiere L, Larrieu D et al (2017) Lack of improvement in health-related quality of life (HRQOL) scores 6 months after surgery for adult spinal deformity (ASD) predicts high revision rate in the second postoperative year. Eur Spine J 26:2160–2166
Acknowledgements
Glynny Kieser for her editorial input.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marques, M.F., Fiere, V., Obeid, I. et al. Pseudarthrosis in adult spine deformity surgery: risk factors and treatment options. Eur Spine J 30, 3225–3232 (2021). https://doi.org/10.1007/s00586-021-06861-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06861-w