Abstract
Purpose
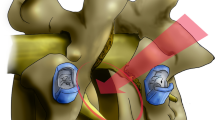
Over the past decade, alternative patient positions for the treatment of the anterior lumbar spine have been explored in an effort to maximize the benefits of direct anterior column access while minimizing the inefficiencies of single or multiple intraoperative patient repositionings. The lateral technique allows for access from L1 to L5 through a retroperitoneal, muscle-splitting, transpsoas approach with placement of a large intervertebral spacer than can reliably improve segmental lordosis, though its inability to be used at L5-S1 limits its overall adoption, as L5-S1 is one of the most common levels treated and where high levels of lordosis are optimal. Recent developments in instrumentation and techniques for lateral-position treatment of the L5-S1 level with a modified anterior lumbar interbody fusion (ALIF) approach have expanded the lateral position to L5-S1, though the positional effect on L5-S1 lordosis is heretofore unreported. The purpose of this study was to compare local and regional alignment differences between ALIFs performed with the patient in the lateral (L-ALIF) versus supine position (S-ALIF).
Methods
Retrospective, multi-center data and radiographs were collected from 476 consecutive patients who underwent L5-S1 L-ALIF (n = 316) or S-ALIF (n = 160) for degenerative lumbar conditions. Patients treated at L4-5 and above with other single-position interbody fusion and posterior fixation techniques were included in the analysis. Baseline patient characteristics were similar between the groups, though L-ALIF patients were slightly older (58 vs. 54 years), with a greater preoperative mean L5-S1 disk height (7.8 vs. 5.8 mm), and with less preoperative slip (6.6 vs. 8.5 mm), respectively. 262 patients were treated with only L-ALIF or S-ALIF at L5-S1 while the remaining 214 patients were treated with either L-ALIF or S-ALIF at L5-S1 along with fusions at other thoracolumbar levels. Lumbar lordosis (LL), L5-S1 segmental lordosis, L5-S1 disk space height, and slip reduction in L5-S1 spondylolisthesis were measured on preoperative and postoperative lateral X-ray images. LL was only compared between single-level ALIFs, given the variability of other procedures performed at the levels above L5-S1.
Results
Mean pre- to postoperative L5-S1 segmental lordosis improved 39% (6.6°) and 31% (4.9°) in the L-ALIF and S-ALIF groups, respectively (p = 0.063). Mean L5-S1 disk height increased by 6.5 mm (89%) in the L-ALIF and 6.4 mm (110%) in the S-ALIF cohorts, (p = 0.650). Spondylolisthesis, in those patients with a preoperative slip, average reduction in the L-ALIF group was 1.5 mm and 2.2 mm in the S-ALIF group (p = 0.175). In patients treated only at L5-S1 with ALIF, mean segmental alignment improved significantly more in the L-ALIF compared to the S-ALIF cohort (7.8 vs. 5.4°, p = 0.035), while lumbar lordosis increased 4.1° and 3.6° in the respective groups (p = 0.648).
Conclusion
Use of the lateral patient position for L5-S1 ALIF, compared to traditional supine L5-S1 ALIF, resulted in at least equivalent alignment and radiographic outcomes, with significantly greater improvement in segmental lordosis in patients treated only at L5-S1. These data, from the largest lateral ALIF dataset reported to date, suggest that—radiographically—the lateral patient position can be considered as an alternative to traditional ALIF positional techniques.


Similar content being viewed by others
References
Umehara S, Zindrick MR, Patwardhan AG, Havey RM, Vrbos LA, Knight GW et al (2000) The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine 25:1617–1624
Oda I, Cunningham BW, Buckley RA et al (1999) Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? Spine 24:2139–2146
Rothenfluh DA, Mueller DA, Rothenfluh E, Min K (2015) Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 24(6):1251–1258
Sparrey CJ, Bailey JF, Safaee M, Clark AJ, Lafage V, Schwab F et al (2014) Etiology of lumbar lordosis and its pathophysiology: a review of the evolution of lumbar lordosis, and the mechanics and biology of lumbar degeneration. Neurosurg Focus 36:E1
Buckland AJ, Ashayeri K, Leon C, Manning J, Eisen L, Medley M, Protopsaltis TS, Thomas JA (2021) Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Spine J 21(5):810–820
Watkins RG 4th, Hanna R, Chang D, Watkins RG 3rd (2014) Sagittal alignment after lumbar interbody fusion: comparing anterior, lateral, and transforaminal approaches. J Spin Disord Tech 27:253–256
Ahlquist S, Park H, Gatto J et al (2018) Does approach matter? A comparative radiographic analysis of spinopelvic parameters in single-level lumbar fusion. Spine J 18(11):1999–2008. https://doi.org/10.1016/j.spinee.2018.03.014
Sembrano JN, Yson SC, Horazdovsky RD et al (2015) Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: analysis of sagittal contour change. Int J Spine Surg 9:16
Hsieh PC, Koski TR, O’Shaughnessy BA et al (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: Implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386
Kim JS, Lee KY, Lee SH, Lee HY (2010) Which lumbar interbody fusion technique is better in terms of level for the treatment of unstable isthmic spondylolisthesis? J Neurosurg Spine 12:171–7
Bassani R, Morselli C, Querenghi AM, Nuara A, Sconfienza LM, Peretti GM (2020) Functional and radiological outcome of anterior retroperitoneal versus posterior transforaminal interbody fusion in the management of single-level lumbar degenerative disease. Neurosurg 49(3):E2. https://doi.org/10.3171/2020.6.FOCUS20374
Jiang SD, Chen JW, Jiang LS (2012) Which procedure is better for lumbar interbody fusion: anterior lumbar interbody fusion or transforaminal lumbar interbody fusion? Arch Orthop Trauma Surg 132(9):1259–66. https://doi.org/10.1007/s00402-012-1546-z
Rothrock RJ, McNeill IT, Yaeger K, Oermann EK, Cho SK, Caridi JM (2018) Lumbar lordosis correction with interbody fusion: systematic literature review and analysis. World Neurosurg 118:21–31. https://doi.org/10.1016/j.wneu.2018.06.216
Nakashima H et al (2019) Changes in sagittal alignment following short-level lumbar interbody fusion: comparison between posterior and lateral lumbar interbody fusions. Asian Spine J 13(6):904–912. https://doi.org/10.31616/asj.2019.0011
Lim JK, Kim SM (2013) Radiographic results of minimally invasive (MIS) lumbar interbody fusion (LIF) compared with conventional lumbar interbody fusion. Korean J Spine 10(2):65–71. https://doi.org/10.14245/kjs.2013.10.2.65
Teng I, Han J, Phan K, Mobbs R (2017) A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci 44:11–17. https://doi.org/10.1016/j.jocn.2017.06.013
Phan K, Thayaparan GK, Mobbs RJ (2015) Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion–systematic review and meta-analysis. Br J Neurosurg 29(5):705–711
Kwee MM, Ho YH, Rozen WM (2015) The prone position during surgery and its complications: a systematic review and evidence-based guidelines. Int Surg 100:292–303
DePasse JM, Palumbo MA, Haque M et al (2015) Complications associated with prone positioning in elective spinal surgery. World J Orthop 6:351–359
Anderton JM (1991) The prone position for the surgical patient: a historical review of the principles and hazards. Br J Anaesth 67(4):452–463
Yson SC, Sembrano JN, Santos ERG et al (2014) Does prone repositioning before posterior fixation produce greater lordosis in lateral lumbar interbody fusion (LLIF)? J Spinal Disord Tech 27(7):364–369
Ziino C, Konopka JA, Ajiboye RM, Ledesma JB, Koltsov JC, Cheng I (2018) Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg 4(4):717–724. https://doi.org/10.21037/jss.2018.12.03
Pimenta L, Amaral R, Taylor W, Tohmeh A, Pokorny G, Rodrigues R, Arnoni D, Guirelli T, Batista M (2021) The prone transpsoas technique: preliminary radiographic results of a multicenter experience. Eur Spine J 30(1):108–113. https://doi.org/10.1007/s00586-020-06471-y
Lamartina C, Berjano P (2020) Prone single-position extreme lat- eral interbody fusion (Pro-XLIF): preliminary results. Eur Spine J. https://doi.org/10.1007/s00586-020-06303-z
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khajavi, K., Menezes, C.M., Braly, B.A. et al. Postoperative spinal alignment comparison of lateral versus supine patient position L5-S1 anterior lumbar interbody fusion. Eur Spine J 31, 2248–2254 (2022). https://doi.org/10.1007/s00586-022-07252-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07252-5