Abstract
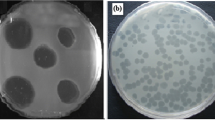
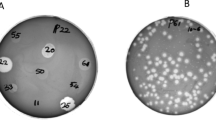
Proteus mirabilis is one of the most frequent causes of catheter-associated urinary tract infections (CAUTIs) owing to its capability to colonize and develop crystalline multidrug-resistant (MDR) biofilms. Here, we report the isolation and partial characterization of three novel bacteriophages, vB_PmiM-ES1a, vB_PmiM-ES1b, and vB_PmiM-ES1c, which were active against the planktonic form and biofilms of the MDR P. mirabilis strain ES01, isolated from CAUTIs in Egypt. The antibiotic susceptibility profile of the P. mirabilis isolates showed resistance to most of the antibiotics tested. The isolated phages were identified morphologically using TEM, and each appeared to have myovirus-like morphology. The three phages displayed strong lytic activity and a narrow host range, and they were stable at different ranges of temperatures and pH values. One-step growth kinetics showed a lysis time of 180 min with a burst size of 99.6, 95, and 86 PFU/cell for phage vB_PmiM-ES1a, vB_PmiM-ES1b, and vB_PmiM-ES1c, respectively. The three phages exhibited different digestion patterns using different restriction enzymes. The genome size was estimated to be 59.39 kb, 62.19 kb, and 52.07 kb for phage vB_PmiM-ES1a, vB_PmiM-ES1b, and vB_PmiM-ES1c, respectively. A phage cocktail including the three phages showed a potential ability to reduce and eradicate a biofilm formed by the MDR Proteus mirabilis EG-ES1. Accordingly, a phage cocktail of vB_PmiM-ES1a, vB_PmiM-ES1b, and vB_PmiM-ES1c is considered a promising candidate for use as a biocontrol agent against MDR Proteus mirabilis bacteria.





Similar content being viewed by others
References
Girlich D, Bonnin RA, Dortet L, Naas T (2020) Genetics of acquired antibiotic resistance genes in Proteus spp. Front Microbiol 11:1–21
Rózalski A, Sidorczyk Z, Kotełko K (1997) Potential virulence factors of Proteus bacilli. Microbiol Mol Biol Rev 61:65–89. https://doi.org/10.1128/.61.1.65-89.1997
Shanmugam P, Jeya M, Linda SS (2013) The bacteriology of diabetic foot ulcers, with a special reference to multidrug resistant strains. J Clin Diagnostic Res 7:441–445. https://doi.org/10.7860/JCDR/2013/5091.2794
Schaffer JN, Pearson MM (2016) Proteus mirabilis and urinary tract infections. In: Urinary tract infections: molecular pathogenesis and clinical management. Taylor & Francis, pp 383–433
O’Hara CM, Brenner FW, Miller JM (2000) Classification, identification, and clinical significance of Proteus, Providencia, and Morganella. Clin Microbiol Rev 13:534–546
Mobley HLT, Belas R, Lockatell V et al (1996) Construction of a flagellum-negative mutant of Proteus mirabilis: effect on internalization by human renal epithelial cells and virulence in a mouse model of ascending urinary tract infection. Infect Immun 64:5332–5340. https://doi.org/10.1128/iai.64.12.5332-5340.1996
Stickler DJ (2008) Bacterial biofilms in patients with indwelling urinary catheters. Nat Clin Pract Urol 5:598–608
Stickler DJ (2014) Clinical complications of urinary catheters caused by crystalline biofilms: something needs to be done. J Intern Med 276:120–129
Armbruster CE, Mobley HLT (2012) Merging mythology and morphology: the multifaceted lifestyle of Proteus mirabilis. Nat Rev Microbiol 10:743–754
Broomfield RJ, Morgan SD, Khan A, Stickler DJ (2009) Crystalline bacterial biofilm formation on urinary catheters by urease-producing urinary tract pathogens: a simple method of control. J Med Microbiol 58:1367–1375. https://doi.org/10.1099/jmm.0.012419-0
Stickler D, Morris N, Moreno MC, Sabbuba N (1998) Studies on the formation of crystalline bacterial biofilms on urethral catheters. Eur J Clin Microbiol Infect Dis 17:649–652. https://doi.org/10.1007/s100960050150
Holling N, Dedi C, Jones CE et al (2014) Evaluation of environmental scanning electron microscopy for analysis of Proteus mirabilis crystalline biofilms in situ on urinary catheters. FEMS Microbiol Lett 355:20–27. https://doi.org/10.1111/1574-6968.12451
Holling N, Lednor D, Tsang S et al (2014) Elucidating the genetic basis of crystalline biofilm formation in Proteus mirabilis. Infect Immun 82:1616–1626. https://doi.org/10.1128/IAI.01652-13
Alves DR, Nzakizwanayo J, Dedi C et al (2019) Genomic and ecogenomic characterization of Proteus mirabilis bacteriophages. Front Microbiol 10:1–14. https://doi.org/10.3389/fmicb.2019.01783
Stickler D, Ganderton L, King J et al (1993) Proteus mirabilis biofilms and the encrustation of urethral catheters. Urol Res 21:407–411. https://doi.org/10.1007/BF00300077
Morgan SD, Rigby D, Stickler DJ (2009) A study of the structure of the crystalline bacterial biofilms that can encrust and block silver Foley catheters. Urol Res 37:89–93. https://doi.org/10.1007/s00240-009-0176-6
Kunin CM (1997) Urinary tract infections. Detection, prevention, and management. Williams & Wilkins, Philadelphia
Chenoweth CE, Gould CV, Saint S (2014) Diagnosis, management, and prevention of catheter-associated urinary tract infections. Infect Dis Clin 28:105–119
Melo LDR, Veiga P, Cerca N et al (2016) Development of a phage cocktail to control Proteus mirabilis catheter-associated urinary tract infections. Front Microbiol. https://doi.org/10.3389/fmicb.2016.01024
Wang JT, Chen PC, Chang SC et al (2014) Antimicrobial susceptibilities of Proteus mirabilis: a longitudinal nationwide study from the Taiwan surveillance of antimicrobial resistance (TSAR) program. BMC Infect Dis 14:1–10. https://doi.org/10.1186/1471-2334-14-486
Yoshikawa TT, Shibata SA, Chow AW, Guze LB (1978) Outbreak of multiply drug-resistant Proteus mirabilis originating in a surgical intensive care unit: in vitro susceptibility pattern. Antimicrob Agents Chemother 13:177–179. https://doi.org/10.1128/AAC.13.2.177
Chong Y, Shimoda S, Yakushiji H et al (2013) Community spread of extended-spectrum β-lactamase-producing Escherichia coli, Klebsiella pneumoniae and Proteus mirabilis: a long-term study in Japan. J Med Microbiol 62:1038–1043. https://doi.org/10.1099/jmm.0.059279-0
Cohen-Nahum K, Saidel-Odes L, Riesenberg K et al (2010) Urinary tract infections caused by multi-drug resistant proteus mirabilis: risk factors and clinical outcomes. Infection 38:41–46. https://doi.org/10.1007/s15010-009-8460-5
Morozova V, Kozlova Y, Shedko E et al (2018) Isolation and characterization of a group of new Proteus bacteriophages. Arch Virol 163:2189–2197. https://doi.org/10.1007/s00705-018-3853-3
Esmael A, Azab E, Gobouri AA et al (2021) Isolation and characterization of two lytic bacteriophages infecting a multi-drug resistant salmonella typhimurium and their efficacy to combat salmonellosis in ready-to-use foods. Microorganisms 9:1–19. https://doi.org/10.3390/microorganisms9020423
Moye ZD, Woolston J, Sulakvelidze A (2018) Bacteriophage applications for food production and processing. Viruses 10(4):205. https://doi.org/10.3390/v10040205
Doss J, Culbertson K, Hahn D et al (2017) A review of phage therapy against bacterial pathogens of aquatic and terrestrial organisms. Viruses 9(3):50. https://doi.org/10.3390/v9030050
Taubeneck U (1963) Demonstration of lysogeny in stable l forms of Proteus mirabilis. J Bacteriol 86:1265–1269. https://doi.org/10.1128/jb.86.6.1265-1269.1963
France DR, Markham NP (1968) Epidemiological aspects of Proteus infections with particular reference to phage typing. J Clin Pathol 21:97–102. https://doi.org/10.1136/jcp.21.1.97
Witoszka M, Strumillo B (1963) Attempted treatment of infected wounds with bacteriophage. Pol Przegl Chir 35:1054–1106
Lehman SM, Donlan RM (2015) Bacteriophage-mediated control of a two-species biofilm formed by microorganisms causing catheter-associated urinary tract infections in an in vitro urinary catheter model. Antimicrob Agents Chemother 59:1127–1137. https://doi.org/10.1128/AAC.03786-14
Nzakizwanayo J, Hanin A, Alves DR et al (2016) Bacteriophage can prevent encrustation and blockage of urinary catheters by Proteus mirabilis. Antimicrob Agents Chemother 60:1530–1536. https://doi.org/10.1128/AAC.02685-15
Carson L, Gorman SP, Gilmore BF (2010) The use of lytic bacteriophages in the prevention and eradication of biofilms of Proteus mirabilis and Escherichia coli. FEMS Immunol Med Microbiol 59:447–455. https://doi.org/10.1111/j.1574-695X.2010.00696.x
Gomaa S, Serry F, Abdellatif H, Abbas H (2019) Elimination of multidrug-resistant Proteus mirabilis biofilms using bacteriophages. Arch Virol 164:2265–2275. https://doi.org/10.1007/s00705-019-04305-x
Biemer JJ (1973) Antimicrobial susceptibility testing by the Kirby-Bauer disc diffusion method. Ann Clin Lab Sci 3:135–140
The Clinical and Laboratory Standards Institute (2016) Performance Standards for Antimicrobial Susceptibility Testing CLSI supplement M100S
Stepanović S, Vuković D, Hola V et al (2007) Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS 115:891–899. https://doi.org/10.1111/j.1600-0463.2007.apm_630.x
Hamed AA, Kabary H, Khedr M, Emam AN (2020) Antibiofilm, antimicrobial and cytotoxic activity of extracellular green-synthesized silver nanoparticles by two marine-derived actinomycete. RSC Adv 10:10361–10367. https://doi.org/10.1039/c9ra11021f
Clokie MRJ, Kropinski AM (2009) Bacteriophages: methods and protocols: isolation, characterization, and interactions, vol 1. Humana Press, New York, pp 971–978
Akhtar M, Viazis S, Diez-Gonzalez F (2014) Isolation, identification and characterization of lytic, wide host range bacteriophages from waste effluents against Salmonella enterica serovars. Food Control 38:67–74. https://doi.org/10.1016/j.foodcont.2013.09.064
Huang C, Shi J, Ma W et al (2018) Isolation, characterization, and application of a novel specific Salmonella bacteriophage in different food matrices. Food Res Int 111:631–641. https://doi.org/10.1016/j.foodres.2018.05.071
Kropinski AM, Mazzocco A, Waddell TE et al (2009) Enumeration of bacteriophages by double agar overlay plaque assay. Methods Mol Biol 501:69–76. https://doi.org/10.1007/978-1-60327-164-6_7
Yamamoto KR, Alberts BM, Benzinger R et al (1970) Rapid bacteriophage sedimentation in the presence of polyethylene glycol and its application to large-scale virus purification. Virology 40:734–744. https://doi.org/10.1016/0042-6822(70)90218-7
Ackermann HW (2012) Bacteriophage electron microscopy. In: Advances in virus research. Elsevier, pp 1–32
Danis-Wlodarczyk K, Olszak T, Arabski M et al (2015) Characterization of the newly isolated lytic bacteriophages KTN6 and KT28 and their efficacy against pseudomonas aeruginosa biofilm. PLoS ONE. https://doi.org/10.1371/journal.pone.0127603
Islam MS, Zhou Y, Liang L et al (2019) Application of a phage cocktail for control of Salmonella in foods and reducing biofilms. Viruses. https://doi.org/10.3390/v11090841
Kostaki M, Chorianopoulos N, Braxou E et al (2012) Differential biofilm formation and chemical disinfection resistance of sessile cells of Listeria monocytogenes strains under monospecies and dual-species (with Salmonella enterica) conditions. Appl Environ Microbiol 78:2586–2595. https://doi.org/10.1128/AEM.07099-11
Chen CY, Chen YH, Lu PL et al (2012) Proteus mirabilis urinary tract infection and bacteremia: risk factors, clinical presentation, and outcomes. J Microbiol Immunol Infect 45:228–236. https://doi.org/10.1016/j.jmii.2011.11.007
Adamus-Bialek W, Zajac E, Parniewski P, Kaca W (2013) Comparison of antibiotic resistance patterns in collections of Escherichia coli and Proteus mirabilis uropathogenic strains. Mol Biol Rep 40:3429–3435. https://doi.org/10.1007/s11033-012-2420-3
Maszewska A, Moryl M, Wu J et al (2021) Amikacin and bacteriophage treatment modulates outer membrane proteins composition in Proteus mirabilis biofilm. Sci Rep 11:1–12. https://doi.org/10.1038/s41598-020-80907-9
Llor C, Bjerrum L (2014) Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 5:229–241
Williams PCM, Isaacs D, Berkley JA (2018) Antimicrobial resistance among children in sub-Saharan Africa. Lancet Infect Dis 18:e33–e44
Amann S, Neef K, Kohl S (2019) Antimicrobial resistance (AMR). Eur J Hosp Pharm 26:175–177. https://doi.org/10.1136/ejhpharm-2018-001820
Esmael A, Hassan MG, Amer MM et al (2020) Antimicrobial activity of certain natural-based plant oils against the antibiotic-resistant acne bacteria. Saudi J Biol Sci 27:448–455. https://doi.org/10.1016/j.sjbs.2019.11.006
Awad HA, Mohamed MH, Badran NF et al (2016) Multidrug-resistant organisms in neonatal sepsis in two tertiary neonatal ICUs, Egypt. J Egypt Public Health Assoc 91:31–38. https://doi.org/10.1097/01.EPX.0000482038.76692.3
Sabry NA, Farid SF, Dawoud DM (2014) Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Soc Adm Pharm. https://doi.org/10.1016/j.sapharm.2013.03.004
Ibrahim OHM (2012) Evaluation of drug and antibiotic utilization in an Egyptian university hospital: an interventional study. Intern Med Open Access 02:1–3. https://doi.org/10.4172/2165-8048.1000109
De J, Sosa A, Byarugaba DK, Amabile-Cuevas CF et al (2010) Antimicrobial resistance in developing countries. Springer
Abdelkader MM, Aboshanab KM, El-Ashry MA, Aboulwafa MM (2017) Prevalence of MDR pathogens of bacterial meningitis in Egypt and new synergistic antibiotic combinations. PLoS ONE 12:e0171349. https://doi.org/10.1371/journal.pone.0171349
Serry FM, Gomaa SE, Abbas HA (2018) Antimicrobial resistance of clinical Proteus mirabilis isolated from different sources. Zagazig J Pharm Sci 27:57–63. https://doi.org/10.21608/zjps.2018.38156
Azeredo J, Sutherland I (2008) The use of phages for the removal of infectious biofilms. Curr Pharm Biotechnol 9:261–266. https://doi.org/10.2174/138920108785161604
Morozova V, Kozlova Y, Shedko E et al (2016) Lytic bacteriophage PM16 specific for Proteus mirabilis: a novel member of the genus Phikmvvirus. Arch Virol 161:2457–2472. https://doi.org/10.1007/s00705-016-2944-2
Yazdi M, Bouzari M, Ghaemi EA (2018) Isolation and characterization of a lytic bacteriophage (vB-PmiS-TH) and its application in combination with ampicillin against planktonic and biofilm forms of Proteus mirabilis isolated from urinary tract infection. J Mol Microbiol Biotechnol 28:37–46. https://doi.org/10.1159/000487137
Thompson RW (2018) The isolation and characterisation of Proteus mirabilis bacteriophages and their effect on the colonisation and blockage of urinary catheters. University of the West of England
Koskella B, Meaden S (2013) Understanding bacteriophage specificity in natural microbial communities. Viruses 5:806–823
Chan BK, Abedon ST, Loc-Carrillo C (2013) Phage cocktails and the future of phage therapy. Future Microbiol 8:769–783
Liu N, Lewis C, Zheng W, Fu ZQ (2020) Phage cocktail therapy: multiple ways to suppress pathogenicity. Trends Plant Sci 25:315–317
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Handling Editor: T. K. Frey.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Esmael, A., Abo-Elmaaty, S.A., Khafaga, E.M. et al. Efficacy of three lytic bacteriophages for eradicating biofilms of multidrug-resistant Proteus mirabilis. Arch Virol 166, 3311–3322 (2021). https://doi.org/10.1007/s00705-021-05241-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-021-05241-5