Abstract
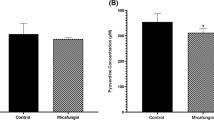
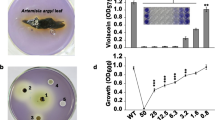
Gallium-based drugs have been repurposed as antibacterial therapeutic candidates and have shown significant potential as an alternative treatment option against drug resistant pathogens. The activity of gallium (Ga3+) is a result of its chemical similarity to ferric iron (Fe3+) and substitution into iron-dependent pathways. Ga3+ is redox inactive in typical physiological environments and therefore perturbs iron metabolism vital for bacterial growth. Gallium maltolate (GaM) is a well-known water-soluble formulation of gallium, consisting of a central gallium cation coordinated to three maltolate ligands, [Ga(Maltol-1H)3]. This study implemented a label-free quantitative proteomic approach to observe the effect of GaM on the bacterial pathogen, Pseudomonas aeruginosa. The replacement of iron for gallium mimics an iron-limitation response, as shown by increased abundance of proteins associated with iron acquisition and storage. A decreased abundance of proteins associated with quorum-sensing and swarming motility was also identified. These processes are a fundamental component of bacterial virulence and dissemination and hence suggest a potential role for GaM in the treatment of P. aeruginosa infection.
Graphic abstract







Similar content being viewed by others
Abbreviations
- AMR:
-
Antimicrobial resistance
- GaM:
-
Gallium maltolate
- PBS:
-
Phosphate buffered saline
- QS:
-
Quorum sensing
- PQS:
-
Pseudomonas Quinolone signal
- SSDA:
-
Statistically significant and differentially abundant
References
Exner M, Bhattacharya S, Christiansen B, Gebel J, Goroncy-Bermes P, Hartemann P, Heeg P, Ilschner C, Kramer A, Larson E, Merkens W, Mielke M, Oltmanns P, Ross B, Rotter M, Schmithausen RM, Sonntag HG, Trautmann M (2017) Antibiotic resistance: what is so special about multidrug-resistant Gram-negative bacteria? GMS Hygiene Infect Control. https://doi.org/10.3205/dgkh000290
Ghai I, Ghai S (2018) Understanding antibiotic resistance via outer membrane permeability. Infect Drug Resist 11:523–530. https://doi.org/10.2147/IDR.S156995
Breijyeh Z, Jubeh B, Karaman R (2020) Resistance of gram-negative bacteria to current antibacterial agents and approaches to resolve it. Molecules (Basel, Switzerland) 25(6):1340. https://doi.org/10.3390/molecules25061340
El Zowalaty ME, Al Thani AA, Webster TJ, El Zowalaty AE, Schweizer HP, Nasrallah GK, Marei HE, Ashour HM (2015) Pseudomonas aeruginosa: arsenal of resistance mechanisms, decades of changing resistance profiles, and future antimicrobial therapies. Future Microbiol 10(10):1683–1706. https://doi.org/10.2217/fmb.15.48
Wang T, Hou Y, Wang R (2019) A case report of community-acquired Pseudomonas aeruginosa pneumonia complicated with MODS in a previously healthy patient and related literature review. BMC Infect Dis 19(1):130. https://doi.org/10.1186/s12879-019-3765-1
Bassetti M, Vena A, Croxatto A, Righi E, Guery B (2018) How to manage Pseudomonas aeruginosa infections. Drugs Context 7:212527. https://doi.org/10.7573/dic.212527
Faure E, Kwong K, Nguyen D (2018) Pseudomonas aeruginosa in Chronic lung infections: How to adapt within the host? Front Immunol 9:2416. https://doi.org/10.3389/fimmu.2018.02416
Sordé R, Pahissa A, Rello J (2011) Management of refractory Pseudomonas aeruginosa infection in cystic fibrosis. Infect Drug Resist 4:31–41. https://doi.org/10.2147/IDR.S16263
Moradali MF, Ghods S, Rehm BH (2017) Pseudomonas aeruginosa lifestyle: a paradigm for adaptation, survival, and persistence. Front Cell Infect Microbiol 7:39. https://doi.org/10.3389/fcimb.2017.00039
Frimmersdorf E, Horatzek S, Pelnikevich A, Wiehlmann L, Schomburg D (2010) How Pseudomonas aeruginosa adapts to various environments: a metabolomic approach. Environ Microbiol 12(6):1734–1747. https://doi.org/10.1111/j.1462-2920.2010.02253.x
Melander RJ, Zurawski DV, Melander C (2018) Narrow-spectrum antibacterial agents. Med Chem Commun 9(1):12–21. https://doi.org/10.1039/C7MD00528H
Pachori P, Gothalwal R, Gandhi P (2019) Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes Dis 6(2):109–119. https://doi.org/10.1016/j.gendis.2019.04.001
Beceiro A, Tomás M, Bou G (2013) Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world? Clin Microbiol Rev 26(2):185–230. https://doi.org/10.1128/CMR.00059-12
Goss CH, Kaneko Y, Khuu L, Anderson GD, Ravishankar S, Aitken ML, Lechtzin N, Zhou G, Czyz DM, McLean K, Olakanmi O, Shuman HA, Teresi M, Wilhelm E, Caldwell E, Salipante SJ, Hornick DB, Siehnel RJ, Becker L, Britigan BE et al (2018) Gallium disrupts bacterial iron metabolism and has therapeutic effects in mice and humans with lung infections. Sci Trans Med 10(460):eaat7520. https://doi.org/10.1126/scitranslmed.aat7520
Chitambar CR (2017) The therapeutic potential of iron-targeting gallium compounds in human disease: from basic research to clinical application. Pharmacol Res 115:56–64. https://doi.org/10.1016/j.phrs.2016.11.009
Kaneko Y, Thoendel M, Olakanmi O, Britigan BE, Singh PK (2007) The transition metal gallium disrupts Pseudomonas aeruginosa iron metabolism and has antimicrobial and antibiofilm activity. J Clin Investig 117(4):877–888. https://doi.org/10.1172/JCI30783
Cherayil BJ (2011) The role of iron in the immune response to bacterial infection. Immunol Res 50(1):1–9. https://doi.org/10.1007/s12026-010-8199-1
Ganz T, Nemeth E (2006) Regulation of iron acquisition and iron distribution in mammals. Biochem Biophys Acta 1763(7):690–699. https://doi.org/10.1016/j.bbamcr.2006.03.014
Puig S, Ramos-Alonso L, Romero AM, Martínez-Pastor MT (2017) The elemental role of iron in DNA synthesis and repair. Metallomics 9(11):1483–1500. https://doi.org/10.1039/c7mt00116a
Caza M, Kronstad JW (2013) Shared and distinct mechanisms of iron acquisition by bacterial and fungal pathogens of humans. Front Cell Infect Microbiol 3:80. https://doi.org/10.3389/fcimb.2013.00080
Cornelis P, Dingemans J (2013) Pseudomonas aeruginosa adapts its iron uptake strategies in function of the type of infections. Front Cell Infect Microbiol 3:75. https://doi.org/10.3389/fcimb.2013.00075
Lau CK, Krewulak KD, Vogel HJ (2016) Bacterial ferrous iron transport: the Feo system. FEMS Microbiol Rev 40(2):273–298. https://doi.org/10.1093/femsre/fuv049
Dumas Z, Ross-Gillespie A, Kümmerli R (2013) Switching between apparently redundant iron-uptake mechanisms benefits bacteria in changeable environments. Proc Biol Sci 280(1764):20131055. https://doi.org/10.1098/rspb.2013.1055
Chitambar CR, Zivkovic-Gilgenbach Z (1990) Role of the acidic receptosome in the uptake and retention of 67Ga by human leukemic HL60 cells. Can Res 50(5):1484–1487
Chikh Z, Ha-Duong NT, Miquel G, El Hage Chahine JM (2007) Gallium uptake by transferrin and interaction with receptor 1. J Biol Inorg Chem 12(1):90–100. https://doi.org/10.1007/s00775-006-0169-7
Chitambar CR (2016) Gallium and its competing roles with iron in biological systems. Biochem Biophys Acta 1863(8):2044–2053. https://doi.org/10.1016/j.bbamcr.2016.04.027
Harris WR, Pecoraro VL (1983) Thermodynamic binding constants for gallium transferrin. Biochemistry 22(2):292–299. https://doi.org/10.1021/bi00271a010
van Amsterdam JA, Kluin-Nelemans JC, van Eck-Smit BL, Pauwels EK (1996) Role of 67Ga scintigraphy in localization of lymphoma. Ann Hematol 72(4):202–207. https://doi.org/10.1007/s002770050161
Chitambar CR (2012) Gallium-containing anticancer compounds. Future Med Chem 4(10):1257–1272. https://doi.org/10.4155/fmc.12.69
Hayes RL (1978) The medical use of gallium radionuclides: a brief history with some comments. Semin Nucl Med 8(3):183–191. https://doi.org/10.1016/s0001-2998(78)80027-0
Timerbaev AR (2009) Advances in developing tris(8-quinolinolato)gallium(iii) as an anticancer drug: critical appraisal and prospects. Metallomics 1(3):193–198. https://doi.org/10.1039/b902861g
Hara T (1974) On the binding of gallium to transferrin. Int J Nuclear Med Biol 1(3):152–154. https://doi.org/10.1016/0047-0740(74)90021-7
Sephton RG, Harris AW (1975) Gallium-67 citrate uptake by cultured tumor cells, stimulated by serum transferrin. J Natl Cancer Inst 54(5):1263–1266. https://doi.org/10.1093/jnci/54.5.1263
Chitambar CR, Seligman PA (1986) Effects of different transferrin forms on transferrin receptor expression, iron uptake, and cellular proliferation of human leukemic HL60 cells. Mechanisms responsible for the specific cytotoxicity of transferrin-gallium. J Clin Investig 78(6):1538–1546. https://doi.org/10.1172/JCI112746
Chitambar CR, Wereley JP, Matsuyama S (2006) Gallium-induced cell death in lymphoma: role of transferrin receptor cycling, involvement of Bax and the mitochondria, and effects of proteasome inhibition. Mol Cancer Ther 5(11):2834–2843
Kubista B, Schoefl T, Mayr L, van Schoonhoven S, Heffeter P, Windhager R, Keppler BK, Berger W (2017) Distinct activity of the bone-targeted gallium compound KP46 against osteosarcoma cells—synergism with autophagy inhibition. J Exp Clin Cancer Res 36(1):52. https://doi.org/10.1186/s13046-017-0527-z
Hart MM, Smith CF, Yancey ST, Adamson RH (1971) Toxicity and antitumor activity of gallium nitrate and periodically related metal salts. J Natl Cancer Inst 47(5):1121–1127
Giacani L, Bernstein LR, Haynes AM, Godornes BC, Ciccarese G, Drago F, Parodi A, Valdevit S, Anselmi L, Tomasini CF, Baca AM (2019) Topical treatment with gallium maltolate reduces Treponema pallidum subsp. pertenue burden in primary experimental lesions in a rabbit model of yaws. PLoS Neglect Trop Dis 13(1):e0007076. https://doi.org/10.1371/journal.pntd.0007076
Finnegan M, Lutz T, Nelson W, Smith A, Orvig C (1987) Neutral water-soluble post-transition-metal chelate complexes of medical interest: aluminum and gallium tris(3-hydroxy-4-pyronates). Inorg Chem 26(13):2171–2176. https://doi.org/10.1021/ic00260a033
Bernstein LR, Tanner T, Godfrey C, Noll B (2000) Chemistry and pharmacokinetics of gallium maltolate, a compound with high oral gallium bioavailability. Met-Based Drugs 7(1):33–47. https://doi.org/10.1155/MBD.2000.33
DeLeon K, Balldin F, Watters C, Hamood A, Griswold J, Sreedharan S, Rumbaugh KP (2009) Gallium maltolate treatment eradicates Pseudomonas aeruginosa infection in thermally injured mice. Antimicrob Agents Chemother 53(4):1331–1337. https://doi.org/10.1128/AAC.01330-08
Myette MS, Elford HL, Chitambar CR (1998) Interaction of gallium nitrate with other inhibitors of ribonucleotide reductase: effects on the proliferation of human leukemic cells. Cancer Lett 129(2):199–204. https://doi.org/10.1016/s0304-3835(98)00104-9
Olakanmi O, Kesavalu B, Pasula R, Abdalla MY, Schlesinger LS, Britigan BE (2013) Gallium nitrate is efficacious in murine models of tuberculosis and inhibits key bacterial Fe-dependent enzymes. Antimicrob Agents Chemother 57(12):6074–6080. https://doi.org/10.1128/AAC.01543-13
Bernstein LR, van der Hoeven JJ, Boer RO (2011) Hepatocellular carcinoma detection by gallium scan and subsequent treatment by gallium maltolate: rationale and case study. Anticancer Agents Med Chem 11(6):585–590. https://doi.org/10.2174/187152011796011046
Jakupec MA, Keppler BK (2004) Gallium in cancer treatment. Curr Top Med Chem 4(15):1575–1583. https://doi.org/10.2174/1568026043387449
Merli D, Profumo A, Bloise N, Risi G, Momentè S, Cucca L, Visai L (2018) Indium/Gallium Maltolate effects on human breast carcinoma cells: in vitro investigation on cytotoxicity and synergism with mitoxantrone. ACS Omega 3(4):4631–4640. https://doi.org/10.1021/acsomega.7b02026
Chitambar CR, Matthaeus WG, Antholine WE, Graff K, O’Brien WJ (1988) Inhibition of leukemic HL60 cell growth by transferrin-gallium: effects on ribonucleotide reductase and demonstration of drug synergy with hydroxyurea. Blood 72(6):1930–1936
Narasimhan J, Antholine WE, Chitambar CR (1992) Effect of gallium on the tyrosyl radical of the iron-dependent M2 subunit of ribonucleotide reductase. Biochem Pharmacol 44(12):2403–2408. https://doi.org/10.1016/0006-2952(92)90686-d
Mowa MB, Warner DF, Kaplan G, Kana BD, Mizrahi V (2009) Function and regulation of class I ribonucleotide reductase-encoding genes in mycobacteria. J Bacteriol 191(3):985–995. https://doi.org/10.1128/JB.01409-08
Pfeifhofer-Obermair C, Tymoszuk P, Petzer V, Weiss G, Nairz M (2018) Iron in the tumor microenvironment-connecting the dots. Front Oncol 8:549. https://doi.org/10.3389/fonc.2018.00549
Wang Y, Yu L, Ding J, Chen Y (2018) Iron metabolism in cancer. Int J Mol Sci 20(1):95. https://doi.org/10.3390/ijms20010095
Chitambar CR (2010) Medical applications and toxicities of gallium compounds. Int J Environ Res Public Health 7(5):2337–2361. https://doi.org/10.3390/ijerph7052337
Chitambar CR (2004a) Apoptotic mechanisms of gallium nitrate: basic and clinical investigations. Oncology (Williston Park, N.Y.) 18(13 Suppl 10):39–44
Başar I, Ayhan A, Bircan K, Ergen A, Taşar C (1991) Transferrin receptor activity as a marker in transitional cell carcinoma of the bladder. Br J Urol 67(2):165–168. https://doi.org/10.1111/j.1464-410x.1991.tb15101.x
Habeshaw JA, Lister TA, Stansfeld AG, Greaves MF (1983) Correlation of transferrin receptor expression with histological class and outcome in non-Hodgkin lymphoma. Lancet (London, England) 1(8323):498–501. https://doi.org/10.1016/s0140-6736(83)92191-8
Chitambar CR (2004b) Gallium nitrate for the treatment of non-Hodgkin’s lymphoma. Expert Opin Investig Drugs 13(5):531–541. https://doi.org/10.1517/13543784.13.5.531
Malfetano JH, Blessing JA, Homesley HD, Hanjani P (1991) A phase II trial of gallium nitrate (NSC #15200) in advanced or recurrent squamous cell carcinoma of the cervix. A gynecologic oncology group study. Investig New Drugs 9(1):109–111. https://doi.org/10.1007/BF00194560
Hijazi S, Visaggio D, Pirolo M, Frangipani E, Bernstein L, Visca P (2018) Antimicrobial activity of gallium compounds on ESKAPE pathogens. Front Cell Infect Microbiol 8:316. https://doi.org/10.3389/fcimb.2018.00316
Rzhepishevska O, Ekstrand-Hammarström B, Popp M, Björn E, Bucht A, Sjöstedt A, Antti H, Ramstedt M (2011) The antibacterial activity of Ga3+ is influenced by ligand complexation as well as the bacterial carbon source. Antimicrob Agents Chemother 55(12):5568–5580. https://doi.org/10.1128/AAC.00386-11
Wang Y, Han B, Xie Y, Wang H, Wang R, Xia W, Li H, Sun H (2019) Combination of gallium(iii) with acetate for combating antibiotic resistant Pseudomonas aeruginosa. Chem Sci 10(24):6099–6106. https://doi.org/10.1039/c9sc01480b
Arnold CE, Bordin A, Lawhon SD, Libal MC, Bernstein LR, Cohen ND (2012) Antimicrobial activity of gallium maltolate against Staphylococcus aureus and methicillin-resistant S. aureus and Staphylococcus pseudintermedius: an in vitro study. Vet Microbiol 155(2–4):389–394. https://doi.org/10.1016/j.vetmic.2011.09.009
Fecteau ME, Aceto HW, Bernstein LR, Sweeney RW (2014) Comparison of the antimicrobial activities of gallium nitrate and gallium maltolate against Mycobacterium avium subsp. paratuberculosis in vitro. Vet J (London, England: 1997) 202(1):195–197
Sheehan G, Kavanagh K (2018) Analysis of the early cellular and humoral responses of Galleria mellonella larvae to infection by Candida albicans. Virulence 9(1):163–172. https://doi.org/10.1080/21505594.2017.1370174
The Uniprot Consortium (2019) A worldwide hub of protein knowledge. Nucleic Acids Res 47(D1):D506–D515. https://doi.org/10.1093/nar/gky1049
Perez-Riverol Y, Csordas A, Bai J, Bernal-Llinares M, Hewapathirana S, Kundu D et al (2018) The PRIDE database and related tools and resources in 2019: improving support for quantification data. Nucleic Acids Res 47(D1):D442–D450. https://doi.org/10.1093/nar/gky1106
Deslyper G, Colgan TJ, Cooper AJ, Holland CV, Carolan JC (2016) A proteomic investigation of hepatic resistance to ascaris in a murine model. PLoS Neglect Trop Dis 10(8):e0004837. https://doi.org/10.1371/journal.pntd.0004837
Skaar EP (2010) The battle for iron between bacterial pathogens and their vertebrate hosts. PLoS Pathog 6(8):e1000949. https://doi.org/10.1371/journal.ppat.1000949
Cohen ND, Slovis NM, Giguère S, Baker S, Chaffin MK, Bernstein LR (2015) Gallium maltolate as an alternative to macrolides for treatment of presumed Rhodococcus equi pneumonia in foals. J Vet Intern Med 29(3):932–939. https://doi.org/10.1111/jvim.12595
Browne N, Kavanagh K (2013) Developing the potential of using Galleria mellonella larvae as models for studying brain infection by Listeria monocytogenes. Virulence 4(4):271–272. https://doi.org/10.4161/viru.24174
Kavanagh K, Sheehan G (2018) The use of Galleria mellonella Larvae to identify novel antimicrobial agents against fungal species of medical interest. J Fungi (Basel, Switzerland) 4(3):113. https://doi.org/10.3390/jof4030113
Taszłow P, Vertyporokh L, Wojda I (2017) Humoral immune response of Galleria mellonella after repeated infection with Bacillus thuringiensis. J Invertebr Pathol 149:87–96. https://doi.org/10.1016/j.jip.2017.08.008
Sheehan G, Clarke G, Kavanagh K (2018) Characterisation of the cellular and proteomic response of Galleria mellonella larvae to the development of invasive aspergillosis. BMC Microbiol 18(1):63. https://doi.org/10.1186/s12866-018-1208-6
Gandra RM, McCarron P, Viganor L, Fernandes MF, Kavanagh K, McCann M, Branquinha MH, Santos A, Howe O, Devereux M (2020) In vivo Activity of copper(II), manganese(II), and silver(I) 1,10-phenanthroline chelates against Candida haemulonii using the Galleria mellonella model. Front Microbiol 11:470. https://doi.org/10.3389/fmicb.2020.00470
Fuchs BB, Li Y, Li D, Johnston T, Hendricks G, Li G, Rajamuthiah R, Mylonakis E (2016) Micafungin elicits an immunomodulatory effect in galleria mellonella and mice. Mycopathologia 181(1–2):17–25. https://doi.org/10.1007/s11046-015-9940-z
Kiley TB, Stanley-Wall NR (2010) Post-translational control of Bacillus subtilis biofilm formation mediated by tyrosine phosphorylation. Mol Microbiol 78(4):947–963. https://doi.org/10.1111/j.1365-2958.2010.07382.x
Klein G, Dartigalongue C, Raina S (2003) Phosphorylation-mediated regulation of heat shock response in Escherichia coli. Mol Microbiol 48(1):269–285. https://doi.org/10.1046/j.1365-2958.2003.03449.x
Standish AJ, Morona R (2014) The role of bacterial protein tyrosine phosphatases in the regulation of the biosynthesis of secreted polysaccharides. Antioxid Redox Signal 20(14):2274–2289. https://doi.org/10.1089/ars.2013.5726
Musumeci L, Bongiorni C, Tautz L, Edwards RA, Osterman A, Perego M, Mustelin T, Bottini N (2005) Low-molecular-weight protein tyrosine phosphatases of Bacillus subtilis. J Bacteriol 187(14):4945–4956. https://doi.org/10.1128/JB.187.14.4945-4956.2005
Yao Q, Zhang L, Wan X, Chen J, Hu L, Ding X, Li L, Karar J, Peng H, Chen S, Huang N, Rauscher FJ 3rd, Shao F (2014) Structure and specificity of the bacterial cysteine methyltransferase effector NleE suggests a novel substrate in human DNA repair pathway. PLoS Pathog 10(11):e1004522. https://doi.org/10.1371/journal.ppat.1004522
Schlagman SL, Hattman S, Marinus MG (1986) Direct role of the Escherichia coli Dam DNA methyltransferase in methylation-directed mismatch repair. J Bacteriol 165(3):896–900. https://doi.org/10.1128/jb.165.3.896-900.1986
Cohen NR, Ross CA, Jain S, Shapiro RS, Gutierrez A, Belenky P, Li H, Collins JJ (2016) A role for the bacterial GATC methylome in antibiotic stress survival. Nat Genet 48(5):581–586. https://doi.org/10.1038/ng.3530
Ghosh D, Veeraraghavan B, Elangovan R, Vivekanandan P (2020) Antibiotic resistance and epigenetics: more to it than meets the eye. Antimicrob Agents Chemother 64(2):e02225-e2319. https://doi.org/10.1128/AAC.02225-19
Truglio JJ, Croteau DL, Van Houten B, Kisker C (2006) Prokaryotic nucleotide excision repair: the UvrABC system. Chem Rev 106(2):233–252. https://doi.org/10.1021/cr040471u
Burby PE, Simmons LA (2019) A bacterial DNA repair pathway specific to a natural antibiotic. Mol Microbiol 111(2):338–353. https://doi.org/10.1111/mmi.14158
Crowley DJ, Hanawalt PC (1998) Induction of the SOS response increases the efficiency of global nucleotide excision repair of cyclobutane pyrimidine dimers, but not 6–4 photoproducts, in UV-irradiated Escherichia coli. J Bacteriol 180(13):3345–3352. https://doi.org/10.1128/JB.180.13.3345-3352.1998
O’Neill M, Bhakta M, Fleming K, Wilks A (2012) Induced fit on heme binding to the Pseudomonas aeruginosa cytoplasmic protein (PhuS) drives interaction with heme oxygenase (HemO). Proc Natl Acad Sci 109(15):5639–5644. https://doi.org/10.1073/pnas.1121549109
Nguyen AT, O’Neill MJ, Watts AM, Robson CL, Lamont IL, Wilks A, Oglesby-Sherrouse AG (2014) Adaptation of iron homeostasis pathways by a Pseudomonas aeruginosa pyoverdine mutant in the cystic fibrosis lung. J Bacteriol 196(12):2265–2276
Reyda MR, Fugate CJ, Jarrett JT (2009) A complex between biotin synthase and the iron-sulfur cluster assembly chaperone HscA that enhances in vivo cluster assembly. Biochemistry 48(45):10782–10792. https://doi.org/10.1021/bi901393t
Romsang A, Duang-Nkern J, Leesukon P, Saninjuk K, Vattanaviboon P, Mongkolsuk S (2014) The iron-sulphur cluster biosynthesis regulator IscR contributes to iron homeostasis and resistance to oxidants in Pseudomonas aeruginosa. PLoS ONE 9(1):e86763. https://doi.org/10.1371/journal.pone.0086763
Miller HK, Auerbuch V (2015) Bacterial iron-sulfur cluster sensors in mammalian pathogens. Metallomics 7(6):943–956. https://doi.org/10.1039/c5mt00012b
Nelson CE, Huang W, Brewer LK, Nguyen AT, Kane MA, Wilks A, Oglesby-Sherrouse AG (2019) Proteomic analysis of the Pseudomonas aeruginosa iron starvation response reveals PrrF small regulatory RNA-dependent iron regulation of twitching motility, amino acid metabolism, and zinc homeostasis proteins. J Bacteriol 201(12):e00754-e818. https://doi.org/10.1128/JB.00754-18
Choi SR, Britigan BE, Narayanasamy P (2019) Dual Inhibition of Klebsiella pneumoniae and Pseudomonas aeruginosa iron metabolism using gallium porphyrin and gallium nitrate. ACS Infect Dis 5(9):1559–1569. https://doi.org/10.1021/acsinfecdis.9b00100
Wegele R, Tasler R, Zeng Y, Rivera M, Frankenberg-Dinkel N (2004) The heme oxygenase(s)-phytochrome system of Pseudomonas aeruginosa. J Biol Chem 279(44):45791–45802. https://doi.org/10.1074/jbc.M408303200
Rutherford ST, Bassler BL (2012) Bacterial quorum sensing: its role in virulence and possibilities for its control. Cold Spring Harbor Perspect Med 2(11):a012427. https://doi.org/10.1101/cshperspect.a012427
Glessner A, Smith RS, Iglewski BH, Robinson JB (1999) Roles of Pseudomonas aeruginosa las and rhl quorum-sensing systems in control of twitching motility. J Bacteriol 181(5):1623–1629. https://doi.org/10.1128/JB.181.5.1623-1629.1999
Turkina MV, Vikström E (2019) Bacteria-host crosstalk: sensing of the quorum in the context of Pseudomonas aeruginosa infections. J Innate Immunity 11(3):263–279. https://doi.org/10.1159/000494069
Drees SL, Li C, Prasetya F, Saleem M, Dreveny I, Williams P, Hennecke U, Emsley J, Fetzner S (2016) PqsBC, a condensing enzyme in the biosynthesis of the Pseudomonas aeruginosa quinolone signal: crystal structure, inhibition, and reaction mechanism. J Biol Chem 291(13):6610–6624. https://doi.org/10.1074/jbc.M115.708453
Liu YC, Hussain F, Negm O, Pavia A, Halliday N, Dubern JF, Singh S, Muntaka S, Wheldon L, Luckett J, Tighe P, Bosquillon C, Williams P, Cámara M, Martínez-Pomares L (2018) Contribution of the alkylquinolone quorum-sensing system to the interaction of Pseudomonas aeruginosa with bronchial epithelial cells. Front Microbiol 9:3018. https://doi.org/10.3389/fmicb.2018.03018
Diggle SP, Winzer K, Chhabra SR, Worrall KE, Cámara M, Williams P (2003) The Pseudomonas aeruginosa quinolone signal molecule overcomes the cell density-dependency of the quorum sensing hierarchy, regulates rhl-dependent genes at the onset of stationary phase and can be produced in the absence of LasR. Mol Microbiol 50(1):29–43. https://doi.org/10.1046/j.1365-2958.2003.03672.x
Heeb S, Fletcher MP, Chhabra SR, Diggle SP, Williams P, Cámara M (2011) Quinolones: from antibiotics to autoinducers. FEMS Microbiol Rev 35(2):247–274. https://doi.org/10.1111/j.1574-6976.2010.00247.x
Whiteley M, Lee KM, Greenberg EP (1999) Identification of genes controlled by quorum sensing in Pseudomonas aeruginosa. Proc Natl Acad Sci USA 96(24):13904–13909. https://doi.org/10.1073/pnas.96.24.13904
Stintzi A, Evans K, Meyer JM, Poole K (1998) Quorum-sensing and siderophore biosynthesis in Pseudomonas aeruginosa: lasR/lasI mutants exhibit reduced pyoverdine biosynthesis. FEMS Microbiol Lett 166(2):341–345. https://doi.org/10.1111/j.1574-6968.1998.tb13910.x
Coin D, Louis D, Bernillon J, Guinand M, Wallach J (1997) LasA, alkaline protease and elastase in clinical strains of Pseudomonas aeruginosa: quantification by immunochemical methods. FEMS Immunol Med Microbiol 18(3):175–184. https://doi.org/10.1111/j.1574-695X.1997.tb01043.x
Wen Y, Kim IH, Son JS, Lee BH, Kim KS (2012) Iron and quorum sensing coordinately regulate the expression of vulnibactin biosynthesis in Vibrio vulnificus. J Biol Chem 287(32):26727–26739. https://doi.org/10.1074/jbc.M112.374165
Zolfaghar I, Evans DJ, Fleiszig SM (2003) Twitching motility contributes to the role of pili in corneal infection caused by Pseudomonas aeruginosa. Infect Immun 71(9):5389–5393. https://doi.org/10.1128/iai.71.9.5389-5393.2003
Murray TS, Ledizet M, Kazmierczak BI (2010) Swarming motility, secretion of type 3 effectors and biofilm formation phenotypes exhibited within a large cohort of Pseudomonas aeruginosa clinical isolates. J Med Microbiol 59(Pt 5):511–520
Chuang SK, Vrla GD, Fröhlich KS, Gitai Z (2019) Surface association sensitizes Pseudomonas aeruginosa to quorum sensing. Nat Commun 10(1):4118. https://doi.org/10.1038/s41467-019-12153-1
Lakshmanan D, Harikrishnan A, Jyoti K, Idul Ali M, Jeevaratnam K (2020) A compound isolated from Alpinia officinarum Hance. inhibits swarming motility of Pseudomonas aeruginosa and down regulates virulence genes. J Appl Microbiol 128(5):1355–1365
Frisk A, Jyot J, Arora SK, Ramphal R (2002) Identification and functional characterization of flgM, a gene encoding the anti-sigma 28 factor in Pseudomonas aeruginosa. J Bacteriol 184(6):1514–1521. https://doi.org/10.1128/jb.184.6.1514-1521.2002
Burrage AM, Vanderpool E, Kearns DB (2018) Assembly order of flagellar rod subunits in Bacillus subtilis. J Bacteriol 200(23):e00425-e518. https://doi.org/10.1128/JB.00425-18
Zhu S, Schniederberend M, Zhitnitsky D, Jain R, Galán JE, Kazmierczak BI, Liu J (2019) In situ structures of polar and lateral flagella revealed by cryo-electron tomography. J Bacteriol 201(13):e00117-e119. https://doi.org/10.1128/JB.00117-19
Patriquin GM, Banin E, Gilmour C, Tuchman R, Greenberg EP, Poole K (2008) Influence of quorum sensing and iron on twitching motility and biofilm formation in Pseudomonas aeruginosa. J Bacteriol 190(2):662–671. https://doi.org/10.1128/JB.01473-07
Lim CK, Hassan KA, Tetu SG, Loper JE, Paulsen IT (2012) The effect of iron limitation on the transcriptome and proteome of Pseudomonas fluorescens Pf-5. PLoS ONE 7(6):e39139. https://doi.org/10.1371/journal.pone.0039139
Sader HS, Huband MD, Castanheira M, Flamm RK (2017) Pseudomonas aeruginosa antimicrobial susceptibility results from four years (2012 to 2015) of the international network for optimal resistance monitoring program in the United States. Antimicrob Agents Chemother 61(3):e02252-e2316. https://doi.org/10.1128/AAC.02252-16
Ekkelenkamp MB, Cantón R, Díez-Aguilar M, Tunney MM, Gilpin DF, Bernardini F, Dale GE, Elborn JS, Bayjanov JR, Fluit A (2020) Susceptibility of Pseudomonas aeruginosa recovered from cystic fibrosis patients to murepavadin and 13 comparator antibiotics. Antimicrob Agents Chemother 64(2):e01541-e1619. https://doi.org/10.1128/AAC.01541-19
Mustafa MH, Chalhoub H, Denis O, Deplano A, Vergison A, Rodriguez-Villalobos H, Tunney MM, Elborn JS, Kahl BC, Traore H, Vanderbist F, Tulkens PM, Van Bambeke F (2016) Antimicrobial susceptibility of Pseudomonas aeruginosa isolated from cystic fibrosis patients in Northern Europe. Antimicrob Agents Chemother 60(11):6735–6741. https://doi.org/10.1128/AAC.01046-16
Pathmanathan SG, Samat NA, Mohamed R (2009) Antimicrobial susceptibility of clinical isolates of Pseudomonas aeruginosa from a Malaysian Hospital. Malaysian J Med Sci 16(2):27–32
Oglesby AG, Farrow JM 3rd, Lee JH, Tomaras AP, Greenberg EP, Pesci EC, Vasil ML (2008) The influence of iron on Pseudomonas aeruginosa physiology: a regulatory link between iron and quorum sensing. J Biol Chem 283(23):15558–15567
Kaur AP, Lansky IB, Wilks A (2009) The role of the cytoplasmic heme-binding protein (PhuS) of Pseudomonas aeruginosa in intracellular heme trafficking and iron homeostasis. J Biol Chem 284(1):56–66. https://doi.org/10.1074/jbc.M806068200
Bollinger N, Hassett DJ, Iglewski BH, Costerton JW, McDermott TR (2001) Gene expression in Pseudomonas aeruginosa: evidence of iron override effects on quorum sensing and biofilm-specific gene regulation. J Bacteriol 183(6):1990–1996
Juhas M, Wiehlmann L, Huber B, Jordan D, Lauber J, Salunkhe P, Limpert AS, von Götz F, Steinmetz I, Eberl L, Tümmler B (2004) Global regulation of quorum sensing and virulence by VqsR in Pseudomonas aeruginosa. Microbiology (Reading, England) 150(Pt 4):831–841
Jiang Q, Chen J, Yang C, Yin Y, Yao K (2019) Quorum sensing: a prospective therapeutic target for bacterial diseases. Biomed Res Int 2019:2015978. https://doi.org/10.1155/2019/2015978
Asif M, Acharya M (2012) Quorum sensing: a nobel target for antibacterial agents. Avicenna J Med 2(4):97–99. https://doi.org/10.4103/2231-0770.110743
Suga H, Smith KM (2003) Molecular mechanisms of bacterial quorum sensing as a new drug target. Curr Opin Chem Biol 7(5):586–591. https://doi.org/10.1016/j.cbpa.2003.08.001
Imperi F, Massai F, Ramachandran Pillai C, Longo F, Zennaro E, Rampioni G, Visca P, Leoni L (2013) New life for an old drug: the anthelmintic drug niclosamide inhibits Pseudomonas aeruginosa quorum sensing. Antimicrob Agents Chemother 57(2):996–1005. https://doi.org/10.1128/AAC.01952-12
Acknowledgements
The production of this publication was supported by funding from a research grant from Science Foundation Ireland (SFI) and is co-funded under the European Regional Development Fund under grant number 12/RC/2275_P2. Q-exactive mass spectrometer was funded under the SFI Research Infrastructure Call 2012; Grant Number: 12/RI/2346 (3).
Author information
Authors and Affiliations
Contributions
Funding: KK. Experimental design: MP, DG, KK. Experimental procedures: MP, KK. Manuscript draft: MP, KK, DG. Editing and approval of manuscript: MP, KK, DG.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
Ethical permission was not required for this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Piatek, M., Griffith, D.M. & Kavanagh, K. Quantitative proteomic reveals gallium maltolate induces an iron-limited stress response and reduced quorum-sensing in Pseudomonas aeruginosa. J Biol Inorg Chem 25, 1153–1165 (2020). https://doi.org/10.1007/s00775-020-01831-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00775-020-01831-x