Abstract
Purpose
This study compared the short-term outcomes of the non-mesh (Desarda) and mesh (Lichtenstein) methods of hernia repair among Black African patients, with regard to acute postoperative pain, day of return to normal gait, operative time and complications.
Methods
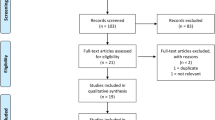
A total of 101 participants (51 in the Lichtenstein arm and 50 in the Desarda arm) were enrolled into this single centre double-blind randomised controlled trial. The outcome measures were evaluated at 1–2 h, 3, 7 and 14 days. The power of the study was set at 80%, CI at 95% and a two-sided P < 0.05 was considered statistically significant.
Results
There was no significant difference in the mean pain score (based on Visual Analogue Scale 0–10) between the study arms [3rd postoperative day (POD): 3.33 ± 1.75 for Lichtenstein and 2.73 ± 1.64 for Desarda, Effect size (CI): 0.59 (−0.088–1.272) and the scores on the 7th POD were 1.31 ± 1.19 for Lichtenstein and 1.31 ± 1.34 for Desarda, effect size (CI): 0.00 (−0.509–0.509)]. No difference was observed in regard to mean day of resumption of normal gait [2.44 ± 1.62 for Lichtenstein and 2.06 ± 1.13 for Desarda, effect size (CI): 0.08 (−0.030–0.193)]. A significant difference was recorded in regard to operative time, with the Desarda repair markedly shorter in duration [15.9 ± 3.52 min for Lichtenstein repair and 10.02 ± 2.93 min for Desarda’s repair, effect size (CI): 5.92 (4.62–7.20), P = 0.0001]. Complication rates were similar in the two study arms.
Conclusions
The results of the study showed that the effectiveness of the Desarda technique with respect to influencing the early clinical outcomes of hernia repair is similar to that of the Lichtenstein method. However, the operator in this study showed that the Desarda repair requires significantly shorter operative time.







Similar content being viewed by others
References
Odula PO, Kakande I (2004) Groin hernia in Mulago Hospital, Kampala. East Central Afr J Surg 9(1):48–52
Ostrow B (2005) What is the most appropriate repair for groin hernias in Africa? Surgery in Africa—Monthly Review. August issue
Desarda MP (2006) Physiological repair of inguinal hernia: a new technique (study of 860 patients). Hernia 10:143–146
Desarda M, Ghosh A (2006) Comparative study of open mesh repair and Desarda’s non-mesh repair in a district hospital in India. East Central Afr J Surg 11(2):28–34
Desarda MP (2003) Surgical physiology of inguinal hernia repair—a study of 200 cases. BMC Surgery 3: 2. doi:10.1186/1471-2482-3-2
Situma SM, Kaggwa S, Masiira NM, Katumba SK (2009) Comparison of Desarda versus modified Bassini inguinal hernia repair: a randomized controlled trial. East Central Afr J Surg 14(2):70–76
Newcombe RG (2001) Reporting of clinical trials in the JO—the consort guidelines. Br J Orthod 27(1):69–70
Lau H, Lee F (2001) Determinant factors of pain after ambulatory inguinal herniorrhaphy: a multi-variate analysis. Hernia 5:17–20
Kehlet H (2008) Chronic pain after groin hernia repair. Br J Surg 95(2):135–136
Bringman S, Wollert S, Sterberg JÖ, Smedberg S, Granlund H, Heikkinen TJ (2006) Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 93:1056–1059
Samir SA, Sasi Yallalampalli BA, Ahmad MS, Charles FB, Albo D, Berger DH (2007) Improved outcomes with the prolene hernia system mesh compared with the time-honored Lichtenstein onlay mesh for inguinal hernia repair. The Am J Surg 193:697–701
Funding
Funds were received from the following organisations: Makerere University and Mulago National Referral and Teaching Hospital.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The study was duly approved by the Research and Ethics Committee of Makerere University College of Health Sciences. The study was also registered at http://register.clinicaltrials.gov with identifier, NCT00941941.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manyilirah, W., Kijjambu, S., Upoki, A. et al. Comparison of non-mesh (Desarda) and mesh (Lichtenstein) methods for inguinal hernia repair among black African patients: a short-term double-blind RCT. Hernia 16, 133–144 (2012). https://doi.org/10.1007/s10029-011-0883-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-011-0883-0