Abstract
Patients with rheumatoid arthritis (RA) suffer from muscle loss, causing reduced muscle strength and endurance. The current study aimed to: (1) evaluate the effects of combined strength and endurance training (CT) on disease activity and functional ability in patients with RA and (2) investigate the benefits of a 6-month supervised CT program on muscle strength, cardio-respiratory fitness, and body composition of RA patients. Forty patients with RA, aged 41–73 years, were recruited for the current study. Twenty of these patients (19 females, one male) were randomly assigned to a 6-month supervised CT program; 20 patients (17 females, three males) served as controls. Within the CT program, strength training consisted of sets of weight bearing exercises for all major muscle groups. In addition to strength training, systematic endurance training was performed on a cycle ergometer two times per week. For RA patients involved in CT, disease activity (p = 0.06) and pain (p = 0.05) were reduced after the 6-month training period while general health (p = 0.04) and functional ability (p = 0.06) improved. Cardio-respiratory endurance was found to have improved significantly (by 10%) after 6 months of CT (p < 0.001). The overall strength of patients undertaking CT increased by an average of 14%. Lean body mass increased, and the percentage of body fat was found to decrease significantly (p < 0.05). A combination of strength and endurance training resulted in considerable improvements in RA patients’ muscle strength and cardio-respiratory endurance, accompanied by positive changes in body composition and functional ability. Long-term training appears to be effective in reducing disease activity and associated pain and was found to have no deleterious effects.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory auto-immune disease, causing progressive damage to the musculoskeletal system [1–4], loss of function [3, 5, 6], and increased energy expenditure [7]. Joint pains are typically caused by inflammation and in advanced cases can relate to joint destruction, further limiting the patients’ physical activities [8]. Consequently, patients with RA suffer from muscle loss and reduced muscle strength, ranging from 30% to 70% [1, 2], while endurance is reduced to 50% [2]. All of these factors contribute to the loss of physical function and quality of life [9]. The frequency of RA is twice as great in women as in men and is most prevalent among those aged 40–60 years [10].
Historically, studies have focused on examining the best conservative therapies, e.g., optimal immobilization, or the value of bed rest [11–13]. However, immobilization and bed rest lead to loss of muscle mass and thus muscle strength, (e.g., a reduction from 1% to 2% per day in healthy young subjects) [14]. In the presence of RA, the loss of muscle mass is even more pronounced [15]. Also known as rheumatoid cachexia, loss of muscle mass is thought to contribute to increased mortality (two to five times higher all-cause mortality) and reduced life expectancy (by 3–18 years) [16].
A recent Cochrane review of dynamic exercise therapy for treating RA concluded that long-term dynamic exercise is effective in increasing aerobic capacity and/or muscle strength [17]. Studies included in this review indicate that strength training (ST) enhances muscle strength and functional capacity [18, 19] as well as prevents further reduction of bone mineral density [20]. In a recent study by Lemmey et al. [21], 24 weeks of high-intensity ST was effective in restoring lean mass and physical function in patients with RA. However, these results are at odds with the earlier findings of Rall et al. [22], in which progressive ST failed to augment fat-free mass in patients with RA. Therefore, the efficacy of ST on lean body mass in patients with RA requires further investigation. Furthermore, at present, there is little evidence whether long-term dynamic exercise reduces cardiovascular disease (CVD) or its risk factors in patients with RA. Because excess cardiovascular mortality is the main cause of reduced life expectancy in RA [23], interventions to reduce CVD risk factors, e.g., total body fat mass, are of vital importance.
There is now good evidence that dynamic physical activity has nil or only a moderate effect on disease activity and pains [24, 25]. These findings are in accordance with a current systematic review provided by Cairns and McVeigh [26]. Still there are discrepancies in findings across studies regarding the effect of ST on functional ability. One recent study reported improvements [27], while other combined programs did not result in statistically or clinically significant changes in their patient populations [18, 28, 29].
The current study sought to evaluate the effects of 6 months of combined strength and endurance training (CT) on: (1) the disease activity and functional ability in patients with RA and (2) the muscle strength, cardio-respiratory fitness, and anthropometry parameters in RA patients.
The null hypothesis of the present investigation is to find a detrimental effect of CT on disease activity in patients with RA (due to the considerable load that strength training puts on the joints and muscles). However, we expect to find no negative effects on disease activity after 6 months of CT since the strength training load is individually increased and systematically adapted under supervision throughout the entire training period by a professional instructor and an experienced physician. The second null hypothesis is not to find improvements in functional ability after 6 months of CT in patients with RA. That ST might have a positive effect on function and disability in patients with RA is to be expected given the recent finding by Giles et al. [30], in which appendicular fat and lean tissue mass exert significant effects on disability score.
Materials and methods
Study population
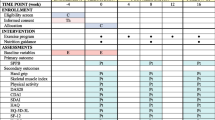
Forty patients (mean age ± standard deviation 59.3 ± 7.9 years; range 41–73 years) with RA were recruited from the Rheumatology Unit at Wilhelminen Hospital Vienna. All patients fulfilled the diagnosis criteria for RA according to the American College of Rheumatology [31]. The patients’ duration of RA symptoms was >2 years at the start of the study; all subjects had been receiving stable drug therapy during the preceding 3 months. All participants were told to continue their current medications during the study. Medications were to be modified only in case of an acute event. Twenty patients (19 females, one male) were randomly assigned to a 6-month supervised combined strength and endurance training program; 20 patients (17 females, three males) served as controls. The patients were assigned, via simple randomization, in a 1:1 ratio to a combined strength and endurance training or control group. Before inclusion in the study, the patients were clinically examined by a rheumatologist to assess their clinical status and to exclude contraindications to perform a physical fitness program. The exclusion criteria included: participation in another study program, cardiac arrhythmia, recent myocardial infarction, stroke, cancer, or an untreated hypertension. The study was approved by a local ethics committee. The purpose, nature, and potential risks of the study were explained to the participants before obtaining their written consent. The progress of patients throughout the study is depicted in Fig. 1.
Measurements
The following examinations were carried out on both groups immediately before and at the end of the training period:
-
Medical history and clinical examination
-
○ Echocardiography—To exclude a RA organ manifestation, each patient had an echocardiography before and at the end of the study period to assess valve morphology and the ejection rate (ER%).
-
○ Blood pressure measurements—Blood pressure measurements were taken with a standard sphygmomanometer after each patient had remained seated for 5 min of quiet rest both before and at the end of the training period (for each training session).
-
○ Laboratory determinations—Serum concentrations of the following parameters were measured by the clinical laboratory of the Herz–Jesu Hospital: sedimentation of the blood (BS), after 1 h and after 2 h, and C- reactive protein (CRP). Samples were analyzed on the day they were collected.
-
○ Medication—Current use of medications was documented relating to the active substance, doses, frequency, and the duration of use.
-
-
Clinical health status
-
Functional ability
-
○ HAQ-DI score (0–3 scale)—Functional ability was assessed with the Health Assessment Questionnaire Disability Index (HAQ-DI) [33]. THE HAQ-DI comprises 20 questions across categories of daily functioning. The total HAQ-DI score ranges from 0 (no functional limitations) to 3 (serious functional limitations). The change score can thus vary from −3 (maximal improvement) to +3 (maximal deterioration).
-
-
Ergometry
Cardio-respiratory fitness was measured by an exercise stress test. All subjects underwent a cycling test on an electrically braked cycle ergometer (Ergometrics 900, Ergoline, Windhagen, Germany) to measure maximum workload (W max) before and after the training period. Heart rate was continuously monitored via an electrocardiogram, with blood pressure measured in the final minute of each work level. The exercise started with a work load of 25 W (W) and was increased stepwise by 25 W every 2 min until exhaustion.
-
Dynamometry
Maximum muscle strength was determined by one repetition maximum (1RM in kilopond) using the Concept 2 Dyno (Concept 2 Ltd, Wilford, Notts, UK). 1RM is defined as the maximal strength that a muscle group is able to generate with a single contraction. Resistance is created in direct response to the patient’s effort. After each completed lift, a monitor shows how much weight was lifted. The Concept 2 Dyno has three basic positions for the determination of muscle strength using the 1RM. A maximum of three tests is allowed to avoid muscle fatigue. The three representative exercises included bench press (m. pectoralis major/minor), bench pull (m. latissimus dorsi), and leg press (m. quadriceps femoris, m. glutei, ischiocrural muscles), all performed in a seated position.
-
Anthropometric measurements
-
○ Body weight—Each participant had her/his body weight measured (Seca, Hamburg, Germany) to the nearest 0.1 kg, and height was recorded to the nearest 0.1 cm while wearing light indoor clothes (without shoes).
-
○ Fat mass—Skinfold measurements were taken with calipers (Model Caliper GMP; Siber Hegner Maschinen AG, Zürich, Switzerland) and recorded to the nearest 0.1 mm. To minimize inter-observer variation, the same experienced instructor assessed each patient’s skinfold. A mean of three measurements was considered to be representative. Measurements were taken at ten different body locations (bucca, chin, chest, mid-axillary-suprailiac, thigh, abdomen, triceps, subscapula, calf, and knee). Percentage of body fat (%BF) was then estimated by using the following sex-appropriate equations [34]: \( {\hbox{BF}}\left( \% \right) = {\hbox{BW}} \times \surd \left\{ {\left[ {\left( {{\hbox{sum of mean values of the ten skinfold measurements}}--{4}0} \right)/{2}0 \times {\hbox{BS}} \times 0.{739}/{\hbox{BW}}} \right] - 0.00{3}} \right\} \times {1}00 \) where body weight (BW) is measured in kilograms and body surface (BS) is equal to 0.007184 × BW0.425 × height0.725.
-
○ Lean body mass—Lean body mass (LBM) was calculated as total weight minus fat mass.
-
Training program
Combined strength and endurance training program
Twenty subjects participated in a 6-month combined strength training and endurance training program undertaken in two sessions, on non-consecutive days of the week. A brief warm-up period required 10 min of stretching exercises before each training session began. Instructions in correct exercise techniques and supervision of the patients throughout the entire training period were performed by a professional instructor and an experienced physician.
Strength training—During the first 2 weeks of the training program, the weight was kept to a minimal level so that the patients could learn the exercise techniques and allow muscles to adapt to the training, as well as to prevent muscle soreness and joint pains. From the third week, the objective of the training was to achieve hypertrophy, so two sets of exercises per muscle group were undertaken each week. One set consisted of ten to 15 repetitions, without interruption, until severe fatigue occurred and completion of further repetitions was impossible. The ten- to 15-repetitions maximum is equivalent to 70% 1RM for most exercises [35]. The training load was individually and systematically adapted to keep the maximum possible repetitions per set (i.e., ten to 15). When more than 15 repetitions were successfully performed at a given weight, the weight was increased by an amount that permitted approximately ten repetitions to be performed. The numbers of sets for each muscle group were systematically increased every 6 weeks, from two at the beginning of the program to three and finally four sets per week at the end of the program. The ST program consisted of a series of exercises for major muscle groups. Exercises to strengthen the upper body included bench press (pectoralis), chest cross (horizontal flexion of the shoulder joint), shoulder press (trapezius), pull downs (latissimus dorsi), bicep curls, tricep extensions, and exercises for abdominal muscles (sit ups). Lower body exercises included leg press (quadriceps femoris). An individualized program was given to the patients. ST was provided within the available range of movement.
Endurance training (ET)—Systematic ET was performed on a cycle ergometer. During the first 4 weeks, ET participants trained for 15 min per session, two times per week. From the fifth week, exercise sessions were increased by 5 min every 4 weeks. The total exercise time per week during the last 4 weeks (excluding warm up and cool down) was 80 min. Heart rate (HR) was monitored continuously throughout the training period (POLAR Electro, Kempele, Finland). Based on the linear correlation between VO2max and HR, training was controlled by an HR according to 60% of VO2max. This was derived from ergometry by using the following formula [36]: \( {\hbox{HR}} = {\hbox{H}}{{\hbox{R}}_{\rm{rest}}} + \left( {{\hbox{H}}{{\hbox{R}}_{\max }} - {\hbox{H}}{{\hbox{R}}_{\rm{rest}}}} \right) \times 0.6 \pm 5{\hbox{ beats}}/\min \), where HRrest was HR after a break of 10 min, in supine position. Thus, the stress in relation to the maximum power was over the training period constant according to 60% of VO2max.
Control group
The patients in the control group were instructed to perform stretching exercises twice a week, without using additional resistance, to maintain their joint mobility. They were free to continue their recreational physical activity with the exception of ST and systematic ET.
Statistical analysis
Data analysis was performed using the Statistical Package for Social Sciences (SPSS 15.0). All parameters were described by mean values ± standard deviation (SD). Normality was assessed with the Shapiro–Wilk test. In dependency of Gaussian distribution, the paired T-test or the Wilcoxon test was carried out to assess the significant differences in changes of the same variables before and after training; the unpaired T-test was used to assess significant differences in changes between the groups. P values < 0.05 were considered statistically significant.
Results
Baseline characteristic and clinical data
At the beginning of testing, both study groups had similar profiles for age, sex, disease duration, medication, and physical characteristics (Table 1). Five of 20 patients dropped out of the intervention group (25%)—meaning, just 15 of the 20 training group patients finished the study period and were included in the statistical analysis. Two patients did not complete the study for health reasons (acute disease activity), two patients dropped out for private reasons, and one for occupational reasons (Fig. 1). Compliance to training was good for the CT group. Of the 48 scheduled sessions, the subjects completed on average 36 sessions, i.e., 75% of the sessions.
Disease activity, pain, and functional ability
Indices of disease activity are shown in Table 2. Results indicate that disease activity improved after the 6-month training period (from 3.57 ± 1.1 to 3.12 ± 1.27; p = 0.06) but not to a statistically significant degree (Fig. 2). Neither BS nor CRP demonstrated significant changes. Combined training produced a significant reduction in pain, evaluated with a 0–100-mm VAS (from 33.33 ± 21.60 to 25.86 ± 19.78; p = 0.05). Furthermore, the patient’s assessment of general health (GH, in mm VAS) improved significantly (from 36.33 ± 21.25 to 25.20 ± 21.44; p = 0.04) (Fig. 3). The effectiveness of combined ST and ET was supported by a 16% improvement in functional capacity (from 1.23 ± 0.80 to 1.01 ± 0.67; p = 0.06) as assessed with a HAQ-DI (Fig. 2).
Cardio-respiratory endurance and muscle strength
After the 6-month training period, no significant changes in the maximum strength (1RM) and maximum workload (W max) were observed between the groups. The muscle strength data and cardio-respiratory data are provided in Table 3. However, results demonstrated that W max improved significantly (by 10%) after 6 months of CT (from 96.0 ± 29.39 W to 106.86 ± 31.25 W; p = 0.00). Maximum strength increased by an average of 22% for leg press (from 66.73 ± 24.69 kp to 81.4 ± 22.37 kp; p = 0.01) (Fig. 4), 11% for bench press (from 26.87 ± 12.66 kp to 29.8 ± 14.4 kp; p = 0.06), and 9% for bench pull (from 30.53 ± 16.02 kp to 33.13 ± 15.41 kp; p = 0.03). The respective data in the control group remained unchanged, with no improvements in W max and 1RM of all muscle groups.
Body composition
The benefits of CT for patients with RA were demonstrated in observed alterations in body composition (Table 4). After the training period, a significant reduction in body weight was observed in the CT group by an average of 1.6 kg (from 70.4 ± 11.19 kg to 68.86 ± 10.84 kg; p = 0.01), whereas no such change was seen in the control group. LBM increased and the percentage of body fat (%BF) decreased significantly after 6 months of CT (from 44.87 ± 4.93 kg to 46.34 ± 6.09 kg, p = 0.12, and from 35.3 ± 6.43%BF to 32.42 ± 4.46%BF, p = 0.02, respectively). In contrast, LBM decreased and the percentage of body fat increased significantly after 6 months for patients in the control group (from 49.88 ± 9.39 kg to 48.42 ± 9.43 kg, p = 0.01, and from 33.01 ± 6.84%BF to 34.56 ± 7.07%BF, p = 0.03). Nevertheless, the difference in change after 6-months between CT and control was not statistically significant for body weight (p = 0.31), %BF (p = 0.36), and LBM (p = 0.51).
Changes in medications
All participants were told to continue their current medication during the 6-month study period. Medications were modified only during acute stages of disease activity in two patients. In this case, non-steroidal anti inflammatory drugs or short-term cortisone therapy was used. Thirty-eight of 40 patients received disease-modifying antirheumatic drug as a basal therapy. Twenty of 40 patients undertook cortisone therapy (Aprednislon, 2.5 to 7.5 mg) and 18 of 40 patients received a biologicum (six infliximab, six etanercept, five adalimumab, and one Mabterra).
Discussion
The current study was designed to examine whether exercise training, especially ST, has negative effects on disease activity. Previous studies examining the effects of moderate or high-intensity exercise in patients with RA found either decreased or stable disease activity [18, 19, 24, 29]. In the current study, disease activity and pain were found to have reduced after 6 months of combined strength and endurance training. Nevertheless, two patients have been ruled out due to disease flares. The reasons for this are not clear. In individuals with RA, a nonspecific overflow may occur because more general adaptations to training take place in a deconditioned state. The typical patient with RA is non-trained, both as regards fitness and strength. Further, evidence indicates that the association between long-term high-intensity exercise training and disease activity may be influenced by baseline damage [37].
General health and functional ability improved (by an average of 30% and 18%, respectively). These results are in line with a systematic review of 15 randomized controlled studies summarizing the effect of dynamic physical activity on disease activity measured by inflammatory markers, pain, or changes in range of motion [25]. A conclusion of the review of these studies was that pain or the ability to perform activities of daily life remained unchanged in most studies and that the disease activity was either reduced or unchanged. Based on findings from the few long-term studies that assessed exercise and the radiologic progression of the small joints, it appears that exercise, even long-term ST, is safe for the joints of hands and feet [20, 24, 29, 38, 39]. None of the reviewed studies reported negative outcomes for function and disease activity with dynamic exercise training.
In a previous study, intensive training in the form of weight bearing sports (volleyball, football, or basketball) was found to be effective in slowing down the loss of bone minerals in patients with RA [24], a finding that is in accordance with an earlier study that reported a modest but positive effect arising from dynamic training on bone mineral content [33]. According to one study, ST alone does not appear to affect bone mineral density in early RA [19]; however, a recent study suggests caution in prescribing long-term high-intensity weight bearing exercise to patients who have significant radiologic damage of large joints as some patients might develop additional damage [40].
The progressive loss of function starts to develop early in RA; inflammation disturbs body functions, which leads to restrictions in daily activities [37]. Tumor necrosis factor-α plays a central role in the pathogenesis of accelerated muscle loss in patients with RA and induces hepatic production of CRP [41]. Elevated serum CRP level has been extensively reported as an independent predictor of CVD [42, 43]. Currently, there is increasing evidence to suggest that CRP might play a role as a direct contributor to the atherosclerotic process [44]. As such, one of the core aims of therapy for RA is the delay of disability and the prevention of CVD. In our study, CRP decreased with CT (53%), possibly indicating reduced active inflammation in the trained state. These results are in line with a very recent systematic review by de Salles et al. [45], which demonstrated a significant reduction in serum CRP levels after ST intervention. It is speculated that the anti-inflammatory effect of ST on CRP may be mediated by the modulation of cytokine production from other sites, besides adipose tissue, such as skeletal muscle and mononuclear cells [46].
This study demonstrated that the combined strength and endurance training program carried out for a prolonged period (24 weeks) resulted in considerable improvements, both in cardio-respiratory endurance (W max) and in muscle strength (1RM) in patients with RA. The maximum strength of all muscle groups increased significantly after 6 months of CT (9–22% of initial levels), and additional improvements were observed in W max, whereas no changes were observed in the control group. These findings are in accordance with a systematic review provided by Stenström and Minor [25], which demonstrated strong evidence for the benefits of aerobic and strengthening exercise for patients with RA. Because decreased muscle strength is considered to be a major impairment among patients with RA [2], findings offer important clinical implications. Indeed our RA subjects already demonstrated reduced muscle strength at the beginning of the training program. It seems sensible to suggest combined training programs to address both, cardio-respiratory fitness as well as muscle strength. An assumption is that the observed strength development attained in the CT group was not inhibited by simultaneous participation in ET [47]. Even though a recent systematic review found that higher-intensity exercise brings about more benefits [26], we have seen that training at moderate intensity (defined as 60% of heart rate reserved for ET and 60–70%1RM for ST) is sufficient to improve aerobic capacity and muscle strength in patients with RA. The physiologic adaptations attributed to CT may allow the trained patient to better tolerate submaximal workloads such as those encountered during day-to-day functional activities. ST improves muscle strength due to better synchronization (in the beginning of the training program) and by hypertrophy; ET improves capillarization of heart and skeletal muscles by increasing the absolute number of capillaries and the capillary density (number of capillaries for a given cross-sectional area of muscle). However, these adaptations can only be obtained when a sufficient training intensity is given [48].
In this study, CT had a positive impact on body composition, with a significant decrease in percentage of body fat (8.2%) and an improvement in LBM (by an average of 1.5 kg). Compared with healthy controls, many patients with RA have a lower fat-free mass and a relatively high fat mass [49], further highlighting the potential benefits of exercise, especially ST, in the treatment of RA. Visceral adiposity is an important risk factor for low-grade inflammation, which is thought to partly explain the excess risk of CVD associated with obesity in RA patients. Data from the Framingham Heart Study suggest that an increase of 0.8 kg in visceral adipose tissue corresponds to an elevated CRP concentration of 1.8 mg/dl in women and a corresponding increase of 0.7 mg/l in men [50]. A study undertaken by Häkkinen et al. confirmed the positive effects of training on lean mass. These authors found that a 21-week combined strength and endurance training program significantly increased muscle mass (by an average of 6.5%) in women with RA [28]. A current study by Marcora et al. assessed the positive effects of a 12-week ST program on fat-free mass (1.2 kg, 6%) in patients with RA, which was mainly concentrated in the arms and legs [51]. In contrast, one older study by Rall et al. found a significant increase in strength (by an average of 57%) without changes in body composition after 12 weeks of progressive ST in patients with RA [22]. The results of the author suggested that patients with RA, perhaps due to their hypermetabolic state, were resistant to the anabolic effects of exercise. Whilst literature on the effect of exercise on body composition in patients with RA is limited, a recent study [21], as well as the current investigation, supports the results of several studies, indicating that an increase in LBM can be obtained if a sufficient training dose is present. Furthermore, Lemmey et al. demonstrated that muscle hypertrophy coincided with significant elevations of attenuated muscle insulin-like growth factor levels, revealing a possible contributory mechanism for rheumatoid cachexia [21].
CT seems to be effective in improving muscle strength, cardio-respiratory endurance and, concomitantly, functional ability, as demonstrated in this study by improvements in self-reported physical function (HAQ-DI). The current results are in line with a recent study by Flint-Wagner et al. demonstrating the positive effects of a 16-week ST program on pain and function in RA patients [27]. These authors indicated a 53% reduction in pain and a clinically important but not significant improvement in physical function with ST. Furthermore, they found that increases in strength were associated with decreased pain and increased function. As it is unclear whether the improvement in muscular function and disease activity with ST can be maintained in the longer term, further studies with post-intervention follow-ups of at least 6 months are required in order to assess whether training programs can be maintained as part of a regular treatment regime and whether the improved rheumatic clustering can be maintained over longer periods. Findings suggest that patients with RA should be encouraged to undertake both aerobic and strength training exercise. Of note is that exercise programs should be carefully tailored for the individual, especially for patients with underlying large joint damage or pre-existing CVD.
Our study has several limitations, namely: (a) the limited number of subjects recruited for the study groups and (b) no follow-up control data for all outcome measures (disease activity, pain, and functional ability). This study has been planned to prioritize a pre–post comparison within the experimental group for a special treatment regime (combined strength and endurance training) rather than to assess significant changes between the groups. The small sample size (low power) may cause some clinically relevant changes in the outcome measures to disappear, and it limits in part the generalization of the results. Still our results suggest that cardio-respiratory endurance and strength improved without negative effects on pain and disease activity. In order to generalize the results of the present study, a larger group of RA patients should be investigated. However, the size of the study groups is comparable to those in previous studies involving combined training in patients with RA [28].
A particular strength of the study was that the rheumatologist who assessed the clinical status of the patients and the research physician who assessed the outcomes did not know which group the patients were in.
Our study is limited by the exclusion of severely disabled patients and patients with active RA and, therefore, our findings cannot be readily generalized to these subgroups of patients. Patient compliance with CT exercise regimes were rated as 75%, indicating that strength and endurance training is well tolerated. However, the safety of physical training programs should be considered not only in terms of disease activity but also by assessing radiological progression over a longer period of time, particularly in RA patients with considerable damage to large joints.
Conclusion
Long-term training appears to be effective in reducing disease activity and pains. Findings demonstrate that a combined strength and endurance training regime undertaken for 24 weeks resulted in considerable improvements in muscle strength and cardio-respiratory endurance in patients with RA. Improvements in physical fitness were accompanied by positive changes in body composition and in functional ability. For these reasons, a regular strength and endurance training is considered an integral element in the effective treatment of RA.
References
Roubenoff R (2003) Exercise and inflammatory disease. Arthritis Rheum 49:263–266
Ekdahl C, Broman G (1992) Muscle strength, endurance and aerobic capacity in rheumatoid arthritis: a comparative study with healthy subjects. Ann Rheum Dis 51:35–40
Gough A, Lilley J, Ayre S, Holder R, Emery P (1994) Generalized bone loss patients with early rheumatoid arthritis. Lancet 344:23–27
Laan R, Buijs W, Verbeel A, Draad M, Corstens L, van de Putte L, van Riel P (1993) Bone mineral density in patients with recent onset rheumatoid arthritis: influence of disease activity and functional capacity. Ann Rheum Dis 52:21–26
Eggelmeijer F, Camps J, Valkema R, Papapoulos S, Pauwels B, Dijkmans B et al (1993) Bone mineral density in ambulant, non-steroid treated female patients with rheumatoid arthritis. Clin Exp Rheumatol 11:381–385
Hansen M, Florescu A, Stoltenberg M, Podenphant J, Pedersen-Zbinden B, Horslev-Petersen K et al (1996) Bone loss in rheumatoid arthritis. Influence of disease activity, duration of disease, functional capacity, and corticosteroid treatment. Scand J Rheumatol 25:367–376
De Carvalho M, Tebexreni A, Salles C, Barros Neto T, Natour J (2004) Oxygen uptake during walking in patients with rheumatoid arthritis—a controlled study. J Rheumatol 31(4):655–662
Hicks EJ (1990) Exercise in patients with inflammatory arthritis and connective tissue disease. Rheum Dis Clin North Am 16:845–870
Plasqui G (2008) The role of physical activity in rheumatoid arthritis. Physiol Behav 94:270–275
Ottawa-Panel (2004) Ottawa Panel evidence-based clinical practice guidelines for therapeutic exercises in the management of rheumatoid arthritis in adults. Phys Ther 84(10):934–972
Partridge R, Duthie J (1963) Controlled trial of the effect of complete immobilization of the joints in rheumatoid arthritis. Ann Rheum Dis 22:91–99
Alexander GJ, Hortas C, Bacon P (1983) Bed rest, activity and the inflammation of rheumatoid arthritis. Br J Rheumatol 22:134–140
Mills JA, Pinals RS, Ropes MW, Short CL, Sutcliffe J (1971) Value of bed rest in patients with rheumatoid arthritis. N Engl J Med 284:453–458
Suzuki Y, Murakami T, Haruna Y, Kawakubo K, Goto S, Makita Y, Ikawa S, Gunji A (1994) Effects of 10 and 20 days bed rest on leg muscle mass and strength in young subjects. Acta Physiol Scand Suppl 616:5–18
Rutherford O, Jones D, Round J (1990) Long-lasting unilateral muscle wasting and weakness following injury and immobilization. Scand J Rehabil Med 22:33–37
Walsmith J, Roubenoff R (2002) Cachexia in rheumatoid arthritis. Int J Cardiol 85(1):89–99
Hurkmanns E, van der Giesen FJ, Vliet Vlieland TP, Schoones J, Van den Ende EC (2009) Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Chochrane Database Syst Rev 7:CD006853
van den Ende C, Breedveld F, le Cessie S, Dijkmans B, de Mug A, Hazes J (2000) Effect of intensive exercise on patients with active rheumatoid arthritis. A randomised clinical trial. Ann Rheum Dis 59:615–621
Häkkinen A, Sokka T, Kotaniemi A, Hannonen P (2001) A randomized two year study of the effects of dynamic strength training on muscle strength, disease activity, functional capacity, and bone mineral density in early rheumatoid arthritis. Arthritis Rheum 44:515–522
Häkkinen A, Sokka T, Kautiainen H, Kotaniemi A, Hannonen P (2004) Sustained maintenance of exercise included muscle strength gains and normal bone mineral density in patients with early rheumatoid arthritis: a 5 year follow up. Ann Rheum Dis 63:910–916
Lemmey AB, Marcora SM, Chester K, Wilson S, Casanova F, Maddison P (2009) Effects of high-intensity resistance training in patients with rheumatoid arthritis: a randomized controlled trial. Arthritis Rheum 61:1726–1734
Rall LC, Meydani SN, Kehayias JJ, Dawson-Huges B, Roubenoff R (1996) The effect of progressive resistance training in rheumatoid arthritis. Increased strength without changes in energy balance or body composition. Arthritis Rheum 39:415–426
Naz SM, Symmons DP (2007) Mortality in established rheumatoid arthritis. Best Pract Res Clin Rheumatol 21:871–883
de Jong Z, Munneke M, Zwinderman A, Kroon H, Ronday K, Lems W et al (2004) Long term high intensity exercise and damage of small joints in rheumatoid arthritis. Ann Rheum Dis 63:1399–1405
Stenstrom CH, Minor MA (2003) Evidence for the benefit of aerobic and strengthening exercise in rheumatoid arthritis. Arthritis Rheum 49(3):428–434
Cairns AP, McVeigh JG (2009) A systematic review of the effects of dynamic exercise in rheumatoid arthritis. Rheumatol Int. doi:10.1007/s00296-009-1090-5
Flint-Wagner HG, Lisse J, Lohman TG, Going SB, Guido T, Cussler E, Gates D, Yocum DE (2009) Assessment of a sixteen-week training program on strength, pain, and function in rheumatoid arthritis patients. J Clin Rheumatol 15:165–171
Häkkinen A, Pakarinen A, Hannonen P, Kautiainen H, Nyman K, Kraemer WJ et al (2005) Effects of prolonged combined strength and endurance training on physical fitness, body composition and serum hormones in women with rheumatoid arthritis and in healthy controls. Clin Exp Rheumatol 23:505–512
de Jong Z, Munneke M, Zwinderman AH et al (2003) Is a long-term high-intensity exercise program effective and safe in patients with rheumatoid arthritis? Results of a randomized controlled trial. Arthritis Rheum 48:2415–2424
Giles JT, Bartlett SJ, Andersen RE, Fontaine KR, Bathon JM (2008) Association of body composition with disability in rheumatoid arthritis: impact of appendicular fat and lean tissue mass. Arthritis Rheum 59:1407–1415
Arnett F, Edworthy S, Bloch D, McShane D, Fries J, Cooper N et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Prevoo MLL, van Hof MA, Kuper HH, van Leeuwen MA, van de Putte LBA, van Riel PLCM (1995) Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Westby MD, Wade JP, Rangno KK, Berkowitz J (2000) A randomized controlled trial to evaluate the effectiveness of an exercise program in women with rheumatoid arthritis taking low dose prednisone. J Rheumatol 27:1674–1680
Allen TH, Peng MT, Chen KP et al (1956) Prediction of total adiposity from skinfolds and the curvilinear relationship between external and internal adiposity. Metabolism 5:346–352
Williams MA, Haskell WL, Ades PA et al (2007) Resistance training in individuals with and without cardiovascular disease: 2007 update. A scientific statement from the American heart association council on clinical cardiology and council on nutrition, physical activity, and metabolism. Circulation 116:572–584
Karvonen MJ, Kentela E, Mustalo O (1957) The effects of training on heart rate, a longitudinal study. Ann Med Exp Biol Fenn 35:307–315
Wolfe F, Cathey M (1991) The assessment and prediction of functional disability in rheumatoid arthritis. J Rheumatol 18:1298–1306
Nordemar R, Ekblom B, Zachrisson L, Lundqvist K (1981) Physical training in rheumatoid arthritis: a controlled long-term study. Scand J Rheumatol 10:17–23
Häkkinen A, Sokka T, Hannonen P (2004) A home-based two-year strength training period in early rheumatoid arthritis led to good long-term compliance: a five-year follow-up. Arthritis Rheum 51:56–62
Munneke M, de Jong Z, Zwinderman AH, Ronday HK, van Schaardenburg D, Dijkmans BA et al (2005) Effect of a high-intensity weight-bearing exercise program on radiologic damage progression of the large joints in subgroups of patients with rheumatoid arthritis. Arthritis Rheum 53:410–417
Walsmith J, Abad L, Kehayias J, Roubenoff R (2004) Tumor necrosis factor-alpha production is associated with less body cell mass in women with rheumatoid arthritis. J Rheumatol 31:23–29
Gonzalez MA, Selwyn AP (2003) Endothelial function, inflammation, and prognosis in cardiovascular disease. Am J Med 115(S.8A):99S–106S
Gonzalez-Gay MA, Gonzalez-Juanatey C, Pineiro A, Garcia-Porrua C, Testa A, Llorca J (2005) High-grade C-reactive protein elevation correlates with accelerated atherogenesis in patients with rheumatoid arthritis. J Rheumatol 32:1219–1223
Wilson AM, Ryan MC, Boyle AJ (2006) The novel role of C-reactive protein in cardiovascular disease: risk marker or pathogen. Int J Cardiol 106:291–297
De Salles BF, Simao R, Fleck SJ, Dias I, Kraemer-Aguiar LG, Bouskela E (2010) Effects of resistance training on cytokines. Int J Sports Med 31:441–450
Kasapis C, Thompson PD (2005) The effects of physical activity on serum C-reactive protein and inflammatory markers: a systematic review. J Am Coll Cardiol 45:1563–1569
McCarthy JP, Agre JC, Graf BK, Pozniak MA, Vailas AC (1995) Compatibility of adaptive responses with combining strength and endurance training. Med Sci Sports Exerc 27:429–436
Swain DP, Franklin BA (2002) Is there a threshold intensity for aerobic training in cardiac patients? Med Sci Sports Exerc 34:1071–1075
Rall LC, Roubenoff R (2004) Rheumatoid cachexia: metabolic abnormalities, mechanisms and interventions. Rheumatol 43:1219–1223
Pou KM, Massaro JM, Hoffmann U et al (2007) Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation 116:1234–1241
Marcora SM, Lemmey AB, Maddison PJ (2005) Can progressive resistance training reverse cachexia in patients with rheumatoid arthritis? Results of a pilot study. J Rheumatol 32:1031–1039
Acknowledgment
This study was supported by the Jubiläumsfonds of the Austrian National Bank (Project No. 11901). We thank Raffaella Gothe for her advice regarding the statistical analysis.
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strasser, B., Leeb, G., Strehblow, C. et al. The effects of strength and endurance training in patients with rheumatoid arthritis. Clin Rheumatol 30, 623–632 (2011). https://doi.org/10.1007/s10067-010-1584-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-010-1584-2