Abstract
Purpose
Hippocampal dysfunction plays a key role in the pathology of psychosis. Given hippocampal sensitivity to changes in cerebral perfusion, decreased baroreflex function could contribute to psychosis pathogenesis. This study had two aims: (1) To compare baroreflex sensitivity in participants with psychosis to two control groups: participants with a nonpsychotic affective disorder and participants with no history of psychiatric disease; (2) to examine the relationship between hippocampal neurometabolites and baroreflex sensitivities in these three groups. We hypothesized that baroreflex sensitivity would be reduced and correlated with hippocampal neurometabolite levels in participants with psychosis, but not in the control groups.
Methods
We assessed baroreflex sensitivity during the Valsalva maneuver separated into vagal and adrenergic components. Metabolite concentrations for cellular processes were quantitated in the entire multivoxel hippocampus using H1-MR spectroscopic (MRS) imaging and were compared with baroreflex sensitivities in the three groups.
Results
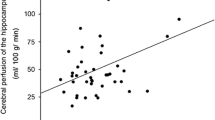
Vagal baroreflex sensitivity (BRS-V) was reduced in a significantly larger proportion of participants with psychosis compared with patients with nonpsychotic affective disorders, whereas participants with psychosis had increased adrenergic baroreflex sensitivity (BRS-A) compared with participants with no history of psychiatric disease. Only in psychotic cases were baroreflex sensitivities associated with hippocampal metabolite concentrations. Specifically, BRS-V was inversely correlated with myo-inositol, a marker of gliosis, and BRS-A was positively correlated with energy dependent dysmyelination (choline, creatine) and excitatory activity (GLX).
Conclusions
Abnormal baroreflex sensitivity is common in participants with psychosis and is associated with MRS markers of hippocampal pathology. Future longitudinal studies are needed to examine causality.


Similar content being viewed by others
Data availability
Data available by request.
References
Ogoh S, Tarumi T (2019) Cerebral blood flow regulation and cognitive function: a role of arterial baroreflex function. J Physiol Sci 69(6):813–823. https://doi.org/10.1007/s12576-019-00704-6
Ogoh S et al (2010) Influence of baroreflex-mediated tachycardia on the regulation of dynamic cerebral perfusion during acute hypotension in humans. J Physiol 588(Pt 2):365–371. https://doi.org/10.1113/jphysiol.2009.180844
Purkayastha S et al (2018) The influence of the carotid baroreflex on dynamic regulation of cerebral blood flow and cerebral tissue oxygenation in humans at rest and during exercise. Eur J Appl Physiol 118(5):959–969. https://doi.org/10.1007/s00421-018-3831-1
De Ferrari GM et al (2007) Baroreflex sensitivity predicts long-term cardiovascular mortality after myocardial infarction even in patients with preserved left ventricular function. J Am Coll Cardiol 50(24):2285–2290. https://doi.org/10.1016/j.jacc.2007.08.043
Adamec I et al (2013) Postural orthostatic tachycardia syndrome associated with multiple sclerosis. Auton Neurosci 173(1–2):65–68. https://doi.org/10.1016/j.autneu.2012.11.009
Habek M et al (2017) Postural orthostatic tachycardia predicts early conversion to multiple sclerosis after clinically isolated syndrome. Eur Neurol 77(5–6):253–257. https://doi.org/10.1159/000469707
den Abeelen ASM et al (2013) Baroreflex function is reduced in Alzheimer’s disease: a candidate biomarker? Neurobiol Aging 34(4):1170–1176. https://doi.org/10.1016/j.neurobiolaging.2012.10.010
Femminella GD et al (2014) Autonomic dysfunction in Alzheimer’s disease: tools for assessment and review of the literature. J Alzheimers Dis 42(2):369–377. https://doi.org/10.3233/JAD-140513
Laosiripisan J et al (2015) Association between cardiovagal baroreflex sensitivity and baseline cerebral perfusion of the hippocampus. Clin Auton Res 25(4):213–218. https://doi.org/10.1007/s10286-015-0296-8
Tzeng YC, Willie CK, Ainslie PN (2010) Baroreflex, cerebral perfusion, and stroke: integrative physiology at its best. Stroke 41(5):e429. https://doi.org/10.1161/STROKEAHA.109.570853
Pendlebury ST, Rothwell PM (2016) Brain atrophy, N-terminal brain natriuretic peptide, and carotid disease: interconnecting relationships between cerebral perfusion, cardiovascular disease, inflammation, and cognitive decline. Arterioscler Thromb Vasc Biol 36(11):2141–2142. https://doi.org/10.1161/ATVBAHA.116.308362
Cao H, Cannon TD (2020) New evidence supporting a role of hippocampus in the development of psychosis. Biol Psychiatry 87(3):200–201. https://doi.org/10.1016/j.biopsych.2019.10.017
McHugo M et al (2019) Hyperactivity and reduced activation of anterior hippocampus in early psychosis. Am J Psychiatry 176(12):1030–1038. https://doi.org/10.1176/appi.ajp.2019.19020151
Allen P et al (2016) Resting hyperperfusion of the hippocampus, midbrain, and Basal Ganglia in people at high risk for psychosis. Am J Psychiatry 173(4):392–399. https://doi.org/10.1176/appi.ajp.2015.15040485
Briend F et al (2020) Hippocampal glutamate and hippocampus subfield volumes in antipsychotic-naive first episode psychosis subjects and relationships to duration of untreated psychosis. Transl Psychiatry 10(1):137. https://doi.org/10.1038/s41398-020-0812-z
Doorduin J et al (2009) Neuroinflammation in schizophrenia-related psychosis: a PET study. J Nucl Med 50(11):1801–1807. https://doi.org/10.2967/jnumed.109.066647
Malaspina D et al (2020) Hippocampal metabolite concentrations in schizophrenia vary in association with rare gene variants in the TRIO gene. Schizophr Res 224:167–169. https://doi.org/10.1016/j.schres.2020.11.001
Clamor A et al (2016) Resting vagal activity in schizophrenia: meta-analysis of heart rate variability as a potential endophenotype. Br J Psychiatry 208(1):9–16. https://doi.org/10.1192/bjp.bp.114.160762
Jung W, Jang KI, Lee SH (2019) Heart and brain interaction of psychiatric illness: a review focused on heart rate variability, cognitive function, and quantitative electroencephalography. Clin Psychopharmacol Neurosci 17(4):459–474. https://doi.org/10.9758/cpn.2019.17.4.459
Zhang Y et al (2020) Heart rate variability changes in patients with panic disorder. J Affect Disord 267:297–306. https://doi.org/10.1016/j.jad.2020.01.132
Malaspina D et al (1997) Diminished cardiac vagal tone in schizophrenia: associations to brain laterality and age of onset. Biol Psychiatry 41(5):612–617. https://doi.org/10.1016/s0006-3223(96)00161-8
Wei L, Chen H, Wu G-R (2018) Structural covariance of the prefrontal-amygdala pathways associated with heart rate variability. Front Human Neurosci. https://doi.org/10.3389/fnhum.2018.00002
Kaufmann H, Norcliffe-Kaufmann L, Palma JA (2020) Baroreflex dysfunction. N Engl J Med 382(2):163–178. https://doi.org/10.1056/NEJMra1509723
Fritze S et al (2019) Differential contributions of brainstem structures to neurological soft signs in first- and multiple-episode schizophrenia spectrum disorders. Schizophr Res 210:101–106. https://doi.org/10.1016/j.schres.2019.05.041
Gupta CN et al (2015) Patterns of gray matter abnormalities in schizophrenia based on an international mega-analysis. Schizophr Bull 41(5):1133–1142. https://doi.org/10.1093/schbul/sbu177
Palamarchuk IS, Baker J, Kimpinski K (2016) The utility of Valsalva maneuver in the diagnoses of orthostatic disorders. Am J Physiol Regul Integr Comp Physiol 310(3):R243–R252. https://doi.org/10.1152/ajpregu.00290.2015
Henderson LA et al (2002) Brain responses associated with the Valsalva maneuver revealed by functional magnetic resonance imaging. J Neurophysiol 88(6):3477–3486. https://doi.org/10.1152/jn.00107.2002
Sandroni P et al (2000) Mechanisms of blood pressure alterations in response to the Valsalva maneuver in postural tachycardia syndrome. Clin Auton Res 10(1):1–5. https://doi.org/10.1007/BF02291382
Maghsudi H et al (2020) Regional metabolite concentrations in aging human brain: comparison of short-TE whole brain MR spectroscopic imaging and single voxel spectroscopy at 3T. Clin Neuroradiol 30(2):251–261. https://doi.org/10.1007/s00062-018-00757-x
Nosaka S (1996) Modifications of arterial baroreflexes: obligatory roles in cardiovascular regulation in stress and poststress recovery. Jpn J Physiol 46(4):271–288. https://doi.org/10.2170/jjphysiol.46.271
Joe P et al (2021) An integrative study of the microbiome gut-brain-axis and hippocampal inflammation in psychosis: persistent effects from mode of birth. Schizophr Res. https://doi.org/10.1016/j.schres.2021.09.019
Nurnberger JI Jr et al (1994) Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch Gen Psychiatry 51(11):849–59. https://doi.org/10.1001/archpsyc.1994.03950110009002. (discussion 863-4)
Pato MT et al (2013) The genomic psychiatry cohort: partners in discovery. Am J Med Genet B Neuropsychiatr Genet 162B(4):306–312. https://doi.org/10.1002/ajmg.b.32160
American Psychiatric Association (2014) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington DC
Low PA (2003) Testing the autonomic nervous system. Semin Neurol 23(4):407–421. https://doi.org/10.1055/s-2004-817725
Palamarchuk I et al (2014) Baroreflex sensitivity: reliability of baroreflex components of the Valsalva maneuver. Auton Neurosci 185:138–140. https://doi.org/10.1016/j.autneu.2014.05.002
Thayer JF, Lane RD (2009) Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev 33(2):81–88. https://doi.org/10.1016/j.neubiorev.2008.08.004
Low PA (1993) Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc 68(8):748–752
Schrezenmaier C et al (2007) Adrenergic and vagal baroreflex sensitivity in autonomic failure. Arch Neurol 64(3):381–386. https://doi.org/10.1001/archneur.64.3.381
Sandroni P, Benarroch EE, Low PA (1991) Pharmacological dissection of components of the Valsalva maneuver in adrenergic failure. J Appl Physiol (1985) 71(4):1563–7. https://doi.org/10.1152/jappl.1991.71.4.1563
Fendrich SJ et al (2022) Patient-reported exposures and outcomes link the gut-brain axis and inflammatory pathways to specific symptoms of severe mental illness. Psychiatry Res 312:114526. https://doi.org/10.1016/j.psychres.2022.114526
Broadley AJ et al (2005) Baroreflex sensitivity is reduced in depression. Psychosom Med 67(4):648–651. https://doi.org/10.1097/01.psy.0000170829.91643.24
Park J et al (2017) Baroreflex dysfunction and augmented sympathetic nerve responses during mental stress in veterans with post-traumatic stress disorder. J Physiol 595(14):4893–4908. https://doi.org/10.1113/JP274269
Fritze S et al (2020) Brainstem alterations contribute to catatonia in schizophrenia spectrum disorders. Schizophr Res 224:82–87. https://doi.org/10.1016/j.schres.2020.09.025
Hirjak D et al (2013) Neurological soft signs and brainstem morphology in first-episode schizophrenia. Neuropsychobiology 68(2):91–99. https://doi.org/10.1159/000350999
Allswede DM, Cannon TD (2018) Prenatal inflammation and risk for schizophrenia: a role for immune proteins in neurodevelopment. Dev Psychopathol 30(3):1157–1178. https://doi.org/10.1017/S0954579418000317
Dunleavy C et al (2022) Inflammation in first-episode psychosis: the contribution of inflammatory biomarkers to the emergence of negative symptoms, a systematic review and meta-analysis. Acta Psychiatr Scand. https://doi.org/10.1111/acps.13416
Williams DP et al (2019) Heart rate variability and inflammation: a meta-analysis of human studies. Brain Behav Immun 80:219–226. https://doi.org/10.1016/j.bbi.2019.03.009
Robinson-Papp J et al (2020) Sympathetic function and markers of inflammation in well-controlled HIV. Brain Behav Immun Health 7:100112. https://doi.org/10.1016/j.bbih.2020.100112
Gomes FV (2022) Altered ventral striatum-hippocampus connectivity during reward processing as an endophenotype for psychosis. Biol Psychiatry 91(2):e7–e9. https://doi.org/10.1016/j.biopsych.2021.10.019
Gregory DF et al (2021) Increased functional coupling between VTA and hippocampus during rest in first-episode psychosis. eNeuro. https://doi.org/10.1523/ENEURO.0375-20.2021
Kraguljac NV et al (2021) Neuroimaging biomarkers in schizophrenia. Am J Psychiatry 178(6):509–521. https://doi.org/10.1176/appi.ajp.2020.20030340
Malaspina D et al (2021) Preliminary findings associate hippocampal (1)H-MR spectroscopic metabolite concentrations with psychotic and manic symptoms in patients with schizophrenia. AJNR Am J Neuroradiol 42(1):88–93. https://doi.org/10.3174/ajnr.A6879
Meyer EJ et al (2016) Metabolic abnormalities in the hippocampus of patients with schizophrenia: a 3D multivoxel MR spectroscopic imaging study at 3T. AJNR Am J Neuroradiol 37(12):2273–2279. https://doi.org/10.3174/ajnr.A4886
Kim S et al (2016) Differential activation of immune/inflammatory response-related co-expression modules in the hippocampus across the major psychiatric disorders. Mol Psychiatry 21(3):376–385. https://doi.org/10.1038/mp.2015.79
Catts VS et al (2014) Increased expression of astrocyte markers in schizophrenia: association with neuroinflammation. Aust N Z J Psychiatry 48(8):722–734. https://doi.org/10.1177/0004867414531078
Nuriya M, Hirase H (2016) Involvement of astrocytes in neurovascular communication. Prog Brain Res 225:41–62. https://doi.org/10.1016/bs.pbr.2016.02.001
Bar KJ et al (2005) Loss of efferent vagal activity in acute schizophrenia. J Psychiatr Res 39(5):519–527. https://doi.org/10.1016/j.jpsychires.2004.12.007
Bunce SC et al (2005) High prevalence of personality disorders among healthy volunteers for research: implications for control group bias. J Psychiatr Res 39(4):421–430. https://doi.org/10.1016/j.jpsychires.2004.09.005
Zandersen M, Parnas J (2019) Borderline personality disorder or a disorder within the schizophrenia spectrum? A psychopathological study. World Psychiatry 18(1):109–110. https://doi.org/10.1002/wps.20598
West ML, Guest RM, Carmel A (2021) Comorbid early psychosis and borderline personality disorder: conceptualizing clinical overlap, etiology, and treatment. Personal Ment Health 15(3):208–222. https://doi.org/10.1002/pmh.1509
Oades RD, Zimmermann B, Eggers C (1996) Conditioned blocking in patients with paranoid, non-paranoid psychosis or obsessive compulsive disorder: associations with symptoms, personality and monoamine metabolism. J Psychiatr Res 30(5):369–390. https://doi.org/10.1016/0022-3956(96)00006-4
Pec O, Bob P, Raboch J (2014) Dissociation in schizophrenia and borderline personality disorder. Neuropsychiatr Dis Treat 10:487–491. https://doi.org/10.2147/NDT.S57627
Geiss L et al (2021) Cardiovascular autonomic modulation during metronomic breathing and stress exposure in patients with borderline personality disorder. Neuropsychobiology 80(5):359–373. https://doi.org/10.1159/000511543
Back SN et al (2022) Reduced vagal activity in borderline personality disorder is unaffected by intranasal oxytocin administration, but predicted by the interaction between childhood trauma and attachment insecurity. J Neural Transm (Vienna) 129(4):409–419. https://doi.org/10.1007/s00702-022-02482-9
Schmahl CG et al (2004) Psychophysiological reactivity to traumatic and abandonment scripts in borderline personality and posttraumatic stress disorders: a preliminary report. Psychiatry Res 126(1):33–42. https://doi.org/10.1016/j.psychres.2004.01.005
Herpertz SC et al (1999) Affective responsiveness in borderline personality disorder: a psychophysiological approach. Am J Psychiatry 156(10):1550–1556. https://doi.org/10.1176/ajp.156.10.1550
Juengling FD et al (2003) Positron emission tomography in female patients with borderline personality disorder. J Psychiatr Res 37(2):109–115. https://doi.org/10.1016/s0022-3956(02)00084-5
Acknowledgements
This work was supported by R01MH110418 (PI: Malaspina) and R01DK122853 (PI: Robinson-Papp)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mueller, B., Robinson-Papp, J., Suprun, M. et al. Baroreflex sensitivity is associated with markers of hippocampal gliosis and dysmyelination in patients with psychosis. Clin Auton Res 33, 101–110 (2023). https://doi.org/10.1007/s10286-023-00929-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-023-00929-x