Abstract
Purpose
To estimate the nationwide, longitudinal prevalence and incidence rates and assess treatment patterns of non-infectious uveitis (NIU) in Japan.
Study design
A retrospective study.
Methods
Health insurance claims’ data of patients with NIU were extracted from the Japan Medical Data Center (JMDC) database and analyzed descriptively (data extraction period, January 2011 to May 2017). Behçet’s disease (BD), Vogt-Koyanagi-Harada (VKH) disease, and sarcoidosis were selected as the primary diseases of NIU.
Results
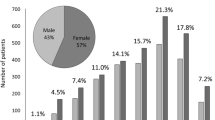
From 2011 to 2016, the mean and median age of patients increased. Most (> 90%) patients were categorized as “undifferentiated NIU” (NIU without specific primary disease information after excluding BD-, VKH disease-, and sarcoidosis-associated NIU). Over 60% of patients with NIU were treated at non-hospital clinics, while the rest were treated at university, public, or other hospitals. The estimated prevalence rate of NIU was 386.5 per 100,000 persons (95% confidence interval [CI], 374.5–398.6) in 2011 and 439.3 per 100,000 persons (95% CI, 432.3–446.3) in 2016; the estimated incidence rate was 189.7 per 100,000 persons (95% CI, 181.2–198.5) in 2012 and 207.8 per 100,000 persons (95% CI, 202.2–213.5) in 2016. Most patients’ prescribed uveitis drugs were ophthalmic drops over the first 6 months after patient presentation and entry into the JMDC database, followed by systemic corticosteroids.
Conclusion
The estimated prevalence of NIU in Japan in recent years was approximately 400 with incidence of 200 per 100,000 persons.



Similar content being viewed by others
References
Rothova A, Suttorp-van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol. 1996;80:332–6.
Dick AD, Tundia N, Sorg R, Zhao C, Chao J, Joshi A, et al. Risk of ocular complications in patients with noninfectious intermediate uveitis, posterior uveitis, or panuveitis. Ophthalmology. 2016;123:655–62.
Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi study. Ophthalmology. 2006;113:1354–62.
Rathinam SR, Cunningham ET Jr. Infectious causes of uveitis in the developing world. Int Ophthalmol Clin. 2000;40:137–52.
Hsu YR, Huang JC, Tao Y, Kaburaki T, Lee CS, Lin TC, et al. Noninfectious uveitis in the Asia-Pacific region. Eye (Lond). 2019;33:66–77.
Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004;111:491–500 (discussion 500).
Suhler EB, Lloyd MJ, Choi D, Rosenbaum JT, Austin DF. Incidence and prevalence of uveitis in Veterans Affairs Medical Centers of the Pacific Northwest. Am J Ophthalmol. 2008;146:890-6.e8.
Acharya NR, Tham VM, Esterberg E, Borkar DS, Parker JV, Vinoya AC, et al. Incidence and prevalence of uveitis: results from the Pacific Ocular Inflammation Study. JAMA Ophthalmol. 2013;131:1405–12.
Thorne JE, Suhler E, Skup M, Tari S, Macaulay D, Chao J, et al. Prevalence of noninfectious uveitis in the United States: a claims-based analysis. JAMA Ophthalmol. 2016;134:1237–45.
Hikita S, Sonoda KH, Hijioka K, Fujimoto T, Ito T, Ishibashi T. Incidence of uveitis in the northern Kyushu region of Japan –comparison between the periods of 1996–2001 and 2003–2008. J Jpn Ophthalmol Soc. 2012;116:847–55 (in Japanese).
Takahashi R, Yoshida A, Inoda S, Okubo A, Kawashima H. Uveitis incidence in Jichi Medical University Hospital, Japan, during 2011–2015. Clin Ophthalmol. 2017;11:1151–6.
Kotake S, Furudate N, Sasamoto Y, Yoshikawa K, Goda C, Matsuda H. Characteristics of endogenous uveitis in Hokkaido. Japan Graefes Arch Clin Exp Ophthalmol. 1996;234:599–603.
Iwata D, Mizuuchi K, Aoki K, Horie Y, Kase S, Namba K, et al. Serial frequencies and clinical features of uveitis in Hokkaido. Japan Ocul Immunol Inflamm. 2017;25(Suppl 1):S15–8.
Keino H, Nakashima C, Watanabe T, Taki W, Hayakawa R, Sugitani A, et al. Frequency and clinical features of intraocular inflammation in Tokyo. Clin Exp Ophthalmol. 2009;37:595–601.
Nakahara H, Kaburaki T, Takamoto M, Okinaga K, Matsuda J, Konno Y, et al. Statistical analyses of endogenous uveitis patients (2007–2009) in central Tokyo area and comparison with previous studies (1963–2006). Ocul Immunol Inflamm. 2015;23:291–6.
Nakahara H, Kaburaki T, Tanaka R, Takamoto M, Ohtomo K, Karakawa A, et al. Frequency of uveitis in the central Tokyo area (2010–2012). Ocul Immunol Inflamm. 2017;25(Suppl 1):S8-14.
Shirahama S, Kaburaki T, Nakahara H, Tanaka R, Takamoto M, Fujino Y, et al. Epidemiology of uveitis (2013–2015) and changes in the patterns of uveitis (2004–2015) in the central Tokyo area: a retrospective study. BMC Ophthalmol. 2018;18:189.
Ohguro N, Sonoda KH, Takeuchi M, Matsumura M, Mochizuki M. The 2009 prospective multi-center epidemiologic survey of uveitis in Japan. Jpn J Ophthalmol. 2012;56:432–5.
Takeuchi M, Kanda T, Kaburaki T, Tanaka R, Namba K, Kamoi K, et al. Real-world evidence of treatment for relapse of noninfectious uveitis in tertiary centers in Japan: a multicenter study. Medicine (Baltimore). 2019;98:14668.
Goto H, Mochizuki M, Yamaki K, Kotake S, Usui M, Ohno S. Epidemiological survey of intraocular inflammation in Japan. Jpn J Ophthalmol. 2007;51:41–4.
Japan Intractable Diseases Information Center. List of intractable diseases. http://www.nanbyou.or.jp/entry/5461. Accessed 5 Apr 2021. (in Japanese).
Japan Intractable Diseases Information Center. Number of patients having the Medical Care Recipient Certificate for Specific Diseases. http://www.nanbyou.or.jp/entry/1356. Accessed 5 Apr 2021. (in Japanese).
Act on Medical Care for Patients with Intractable/Rare Diseases. Law number: Act No. 50 of 2014. Last version: Amendment of Act No. 68 of 2014.
Japanese Ocular Inflammation Society. Guideline for treatment of uveitis (June 10, 2019). https://www.nichigan.or.jp/member/journal/guideline/detail.html?itemid=316&dispmid=909. Accessed 5 Apr 2021. (in Japanese).
Mitsubishi Tanabe Pharma Corporation. REMICADE® for I.V. Infusion Japanese package insert version 1 (revised May 2019). https://www.info.pmda.go.jp/go/pack/2399402F1026_1_43/. Accessed 5 Apr 2021. (in Japanese).
AbbVie GK. Humira® Japanese package insert version 2 (revised November 2020). https://www.info.pmda.go.jp/go/pack/3999426G3027_1_05/. Accessed 5 Apr 2021. (in Japanese).
Japanese Ophthalmological Society. Guideline for diagnosis and treatment of ocular Behçet disease, Section 6 Treatment of ocular Behçet disease. 2012. https://www.nichigan.or.jp/member/journal/guideline/detail.html?itemid=290&dispmid=909. Accessed 5 Apr 2021. (in Japanese).
Herbort CP Jr, Abu El Asrar AM, Yamamoto JH, Pavésio CE, Gupta V, Khairallah M, et al. Reappraisal of the management of Vogt-Koyanagi-Harada disease: sunset glow fundus is no more a fatality. Int Ophthalmol. 2017;37:1383–95.
Japan Society of Sarcoidosis and Other Granulomatous Disorders. Guidance on sarcoidosis treatment. 2020. https://www.jssog.com/journal. Accessed 5 Apr 2021. (in Japanese).
Statistics Bureau of Japan, Ministry of Internal Affairs and Communications. Result of the Population Estimates. https://www.stat.go.jp/english/data/jinsui/2.html. Accessed 5 Apr 2021.
Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20:413–9.
O’Keefe GA, Rao NA. Vogt-Koyanagi-Harada disease. Surv Ophthalmol. 2017;62:1–25.
Yamanaka H, Sugiyama N, Inoue E, Taniguchi A, Momohara S. Estimates of the prevalence of and current treatment practices for rheumatoid arthritis in Japan using reimbursement data from health insurance societies and the IORRA cohort (I). Mod Rheumatol. 2014;24:33–40.
Ohisa M, Kimura Y, Matsuo J, Akita T, Sato T, Matsuoka T, et al. Estimated numbers of patients with liver disease related to hepatitis B or C virus infection based on the database reconstructed from medical claims from 2008 to 2010 in Japan. Hepatol Res. 2015;45:1228–40.
Miwa H, Takeshima T, Iwasaki K, Hiroi S. Medical cost, incidence rate, and treatment status of gastroesophageal reflux disease in Japan: analysis of claims data. J Med Econ. 2016;19:1049–55.
Hwang DK, Chou YJ, Pu CY, Chou P. Epidemiology of uveitis among the Chinese population in Taiwan: a population-based study. Ophthalmology. 2012;119:2371–6.
Rim TH, Kim SS, Ham DI, Yu SY, Chung EJ, Lee SC, Korean Uveitis Society. Incidence and prevalence of uveitis in South Korea: a nationwide cohort study. Br J Ophthalmol. 2018;102:79–83.
Japan Ophthalmological Society. Guideline for diagnosis and treatment of ocular Behçet disease, Section 2 Epidemiology of Behçet disease. 2012. https://www.nichigan.or.jp/member/journal/guideline/detail.html?itemid=290&dispmid=909. Accessed 5 Apr 2021. (in Japanese).
Ohno S, Inaba Y, Inoko H, Onoe K, Mochizuki M, Usui M, et al. Grant-in-Aid for Scientific Research. Research on the mechanism of onset of Harada disease. Project No. 02304049. 1992. https://kaken.nii.ac.jp/ja/grant/KAKENHI-PROJECT-02304049/. Accessed 5 Apr 2021. (in Japanese).
Japan Intractable Diseases Information Center. Sarcoidosis. http://www.nanbyou.or.jp/entry/110. Accessed 5 Apr 2021. (in Japanese).
Matsuo T, Fujiwara N, Nakata Y. First presenting signs or symptoms of sarcoidosis in a Japanese population. Jpn J Ophthalmol. 2005;49:149–52.
Acknowledgements
This work was funded by AbbVie GK. AbbVie GK participated in the study design; data analysis and interpretation; and writing, reviewing, and approval of the publication. We thank Prof. Ishikawa of the International University of Health and Welfare for his contribution as an advisor and database study expert, and Motohiro Okayasu, Yoko Yoshinaga, and Masahiko Nakayama, past or current AbbVie employees, for their contribution to the design of this study. Data extraction and statistical analyses were performed by JMDC Co. Ltd. and funded by AbbVie GK. Medical writing support was provided by Mami Hirano, MS, of Cactus Communications and funded by AbbVie GK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Umazume, None; N. Ohguro, None; A. A. Okada, Grants (Bayer, Novartis, Santen, Mitsubishi Tanabe, Alcon), Consulting fees (Bayer, AbbVie, Astellas, Biocon Biologics, Daiichi Sankyo, Allergan, Chugai), Lecture fees (Bayer, Kowa, Novartis, Santen, Mitsubishi Tanabe, Senju, Alcon, Otsuka); K. Namba, Grant (AbbVie, Mitsubishi Tanabe, Eisai, EP-CRSU), Lecture fee (Alcon, Pfizer, Novartis, Kowa, Senju, Mitsubishi Tanabe, Eisai, AbbVie, Santen, Celgene); K. Sonoda, None; H. Goto, None; H. Tsuruga and K. Morita are employees of AbbVie GK and may receive stock.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Hidekazu Tsuruga
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Umazume, A., Ohguro, N., Okada, A.A. et al. Prevalence and incidence rates and treatment patterns of non-infectious uveitis in Japan: real-world data using a claims database. Jpn J Ophthalmol 65, 657–665 (2021). https://doi.org/10.1007/s10384-021-00850-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-021-00850-8