Abstract
Introduction
Metabolic syndrome (MS) is defined by having at least 3 of 4 components: obesity, dyslipidemia, hypertension (HTN), and diabetes. Prior studies analyzed the individual components of MS for all breast cancers which are predominantly hormone positive. Our study is the first to evaluate MS in triple-negative breast cancer (TNBC).
Methods
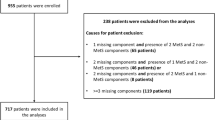
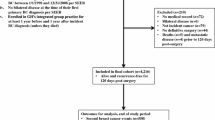
A retrospective review of TNBC from 2007 to 2013 identified 177 patients with complete information for statistical analysis. Cox proportional hazards models were used to test the association between MS, disease-free survival (DFS), and overall survival (OS).
Results
48 (27%) patients had MS. After controlling for age, race, pathologic stage, surgery type, and additional comorbidities outside of MS, MS was significantly associated with poorer DFS (adjusted HR: 2.24, p = 0.030), but not associated with OS (adjusted HR: 1.92, p = 0.103). HTN was significantly associated with poorer DFS (adjusted HR: 3.63, p = 0.006) and OS (adjusted HR: 3.45, p = 0.035) in the univariable and multivariable analyses. Diabetes was not associated with worse OS or DFS. The 5-year age-adjusted OS rates for 60-year-old patients with and without diabetes were 85.8% and 87.3%, respectively. The age-adjusted 5-year OS rate for 60-year old patients was higher in patients with a body mass index (BMI) > 30 (90.2%) versus BMIs of 25–29.9 (88.2%) or < 25 (83.5%).
Conclusion
In the TNBC population, MS was significantly associated with poorer DFS, but not associated with OS. HTN was the only component of MS that was significantly associated with both DFS and OS. Obesity has a potential small protective benefit in the TNBC population.


Similar content being viewed by others
References
Li T, Mello-Thoms C, Brennan PC (2016) Descriptive epidemiology of breast cancer in China: incidence, mortality, survival and prevalence. Breast Cancer Res Treat 159(3):395–406
Davis AA, Kaklamani VG (2012) Metabolic syndrome and triple-negative breast cancer: a new paradigm. Int J Breast Cancer 2012:809291
Ebtekar F, Dalvand S, Gheshlagh RG (2018) The prevalence of metabolic syndrome in postmenopausal women: a systematic review and meta-analysis in Iran. Diabetes Metab Syndr 12(6):955–960
Muhidin SO, Magan AA, Osman KA et al (2012) The relationship between nonalcoholic fatty liver disease and colorectal cancer: the future challenges and outcomes of the metabolic syndrome. J Obes 2012:637538
Rapp K, Schroeder J, Klenk J et al (2006) Fasting blood glucose and cancer risk in a cohort of more than 140,000 adults in Austria. Diabetologia 49(5):945–952
Moebus S, Hanisch J, Bramlage P et al (2008) Regional differences in the prevalence of the metabolic syndrome in primary care practices in Germany. Dtsch Arztebl Int 105(12):207–213
Sighoko D, Hunt BR, Irizarry B et al (2018) Disparity in breast cancer mortality by age and geography in 10 racially diverse US cities. Cancer Epidemiol 53:178–183
Wang M, Cheng N, Zheng S et al (2015) Metabolic syndrome and the risk of breast cancer among postmenopausal women in North-West China. Climacteric 18(6):852–858
Ross-Innes CS, Stark R, Teschendorff AE et al (2012) Differential oestrogen receptor binding is associated with clinical outcome in breast cancer. Nature 481(7381):389–393
Scott LC, Mobley LR, Kuo TM et al (2019) Update on triple-negative breast cancer disparities for the United States: a population-based study from the United States Cancer Statistics database, 2010 through 2014. Cancer 125(19):3412–3417
Ma H, Ursin G, Xu X et al (2018) Body mass index at age 18 years and recent body mass index in relation to risk of breast cancer overall and ER/PR/HER2-defined subtypes in white women and African-American women: a pooled analysis. Breast Cancer Res 20(1):5
Cespedes Feliciano EM, Chen WY, Bradshaw PT et al (2019) Adipose tissue distribution and cardiovascular disease risk among breast cancer survivors. J Clin Oncol 37(28):2528–2536
Liu LN, Miaskowski C, Wang JS et al (2010) Accuracy of body mass index to determine obesity in women with breast cancer: an observational study of Taiwanese sample. Int J Nurs Stud 47(8):994–1000
Tait S, Pacheco JM, Gao F et al (2014) Body mass index, diabetes, and triple-negative breast cancer prognosis. Breast Cancer Res Treat 146(1):189–197
Agnoli C, Berrino F, Abagnato CA et al (2010) Metabolic syndrome and postmenopausal breast cancer in the ORDET cohort: a nested case-control study. Nutr Metab Cardiovasc Dis 20(1):41–48
Chen Y, Wen YY, Li ZR et al (2016) The molecular mechanisms between metabolic syndrome and breast cancer. Biochem Biophys Res Commun 471(4):391–395
Ahmadi A, Leipsic J, Feuchtner G et al (2015) Is metabolic syndrome predictive of prevalence, extent, and risk of coronary artery disease beyond its components? Results from the multinational coronary CT angiography evaluation for clinical outcome: an international multicenter registry (CONFIRM). PLoS ONE 10(3):e0118998
Dankner R, Boker LK, Boffetta P et al (2018) A historical cohort study on glycemic-control and cancer-risk among patients with diabetes. Cancer Epidemiol 57:104–109
Esposito K, Chiodini P, Capuano A et al (2013) Metabolic syndrome and postmenopausal breast cancer: systematic review and meta-analysis. Menopause 20(12):1301–1309
Hauner D, Hauner H (2014) Metabolic syndrome and breast cancer: is there a link? Breast Care (Basel) 9(4):277–281
Jiralerspong S, Kim ES, Dong W et al (2013) Obesity, diabetes, and survival outcomes in a large cohort of early-stage breast cancer patients. Ann Oncol 24(10):2506–2514
Ma FJ, Liu ZB, Qu L et al (2014) Impact of type 2 diabetes mellitus on the prognosis of early stage triple-negative breast cancer in People’s Republic of China. Onco Targets Ther 7:2147–2154
Yang Y, Lynch BM, Hodge AM et al (2017) Blood pressure and risk of breast cancer, overall and by subtypes: a prospective cohort study. J Hypertens 35(7):1371–1380
Li DJ, Evans RG, Yang ZW et al (2011) Dysfunction of the cholinergic anti-inflammatory pathway mediates organ damage in hypertension. Hypertension 57(2):298–307
Geng Y, Chandrasekaran S, Hsu JW et al (2013) Phenotypic switch in blood: effects of pro-inflammatory cytokines on breast cancer cell aggregation and adhesion. PLoS ONE 8(1):e54959
Bayraktar S, Hernadez-Aya LF, Lei X et al (2012) Effect of metformin on survival outcomes in diabetic patients with triple receptor-negative breast cancer. Cancer 118(5):1202–1211
Peairs KS, Barone BB, Snyder CF et al (2011) Diabetes mellitus and breast cancer outcomes: a systematic review and meta-analysis. J Clin Oncol 29(1):40–46
Herath HMM, Weerasinghe NP, Weerarathna TP et al (2018) A comparison of the prevalence of the metabolic syndrome among Sri Lankan patients with type 2 diabetes mellitus using WHO, NCEP-ATP III, and IDF definitions. Int J Chronic Dis 2018:7813537
Mowad R, Chu QD, Li BD et al (2013) Does obesity have an effect on outcomes in triple-negative breast cancer? J Surg Res 184(1):253–259
Morris GJ, Naidu S, Topham AK et al (2007) Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients: a single-institution compilation compared with the National Cancer Institute’s Surveillance, Epidemiology, and End Results database. Cancer 110(4):876–884
Dietze EC, Sistrunk C, Miranda-Carboni G et al (2015) Triple-negative breast cancer in African-American women: disparities versus biology. Nat Rev Cancer 15(4):248–254
Shen Y, Dong W, Esteva FJ et al (2007) Are there racial differences in breast cancer treatments and clinical outcomes for women treated at M.D. Anderson Cancer Center? Breast Cancer Res Treat 102(3):347–56
Shachar SS, Jolly TA, Jones E et al (2018) Management of triple-negative breast cancer in older patients: how is it different? Oncology (Williston Park) 32(2):58–63
Sineshaw HM, Freedman RA, DeSantis CE et al (2018) Treatment patterns among women diagnosed with stage I–III triple-negative breast cancer. Am J Clin Oncol 41(10):997–1007
Funding
This work was supported by the Sharpe Strumia Foundation [Grant Number SSRF2019-20].
Author information
Authors and Affiliations
Contributions
KK developed the study protocol, assembled the database, and assisted in writing the manuscript. MEB was the lead statistician who provided data analysis and interpretation of data. LS helped with study development and manuscript writing. SL oversaw the development of study protocol and analyses. WBC assisted with study development, analysis, and manuscript development. TGF worked in study design, analysis, and manuscript development. NZC assisted with study design, analyses, and manuscript development.
Corresponding author
Ethics declarations
Conflict of interest
All the authors of this manuscript have no conflicts of interest to disclose. Only funding was that of Sharpe Strumia as listed above to Kaitlyn Kennard MD.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kennard, K., Buckley, M.E., Sizer, L.M. et al. Metabolic Syndrome: does this influence breast cancer outcomes in the triple-negative population?. Breast Cancer Res Treat 186, 53–63 (2021). https://doi.org/10.1007/s10549-020-06034-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06034-1