Abstract
Purpose
Fatigue and anxiety are common and significant symptoms reported by cancer patients. Few studies have examined the trajectory of multidimensional fatigue and anxiety, the relationships between them and with quality of life.
Methods
Breast cancer patients (n = 580) from community oncology clinics and age-matched controls (n = 364) completed fatigue and anxiety questionnaires prior to chemotherapy (A1), at chemotherapy completion (A2), and six months post-chemotherapy (A3). Linear mixed models (LMM) compared trajectories of fatigue /anxiety over time in patients and controls and estimated their relationship with quality of life. Models adjusted for age, education, race, BMI, marital status, menopausal status, and sleep symptoms.
Results
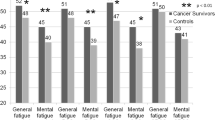
Patients reported greater fatigue and anxiety compared to controls at all time points (p’s < 0.001, 35% clinically meaningful anxiety at baseline). From A1 to A2 patients experienced a significant increase in fatigue (β = 8.3 95%CI 6.6,10.0) which returned to A1 values at A3 but remained greater than controls’ (p < 0.001). General, mental, and physical fatigue subscales increased from A1 to A2 remaining significantly higher than A1 at A3 (p < 0.001). Anxiety improved over time (A1 to A3 β = − 4.3 95%CI -2.6,-3.3) but remained higher than controls at A3 (p < 0.001). Among patients, fatigue and anxiety significantly predicted one another and quality of life. Menopausal status, higher BMI, mastectomy, and sleep problems also significantly predicted change in fatigue.
Conclusion
Breast cancer patients experience significant fatigue and anxiety up to six months post-chemotherapy that is associated with worse quality of life. Future interventions should simultaneously address anxiety and fatigue, focusing on mental and physical fatigue subdomains.



Similar content being viewed by others
Data Availability
Please contact the authors for any questions related to data.
Code Availability
SAS Code is available upon request.
References
Bower JE, Bak K, Berger A et al (2014) Screening, assessment, and management of fatigue in adult survivors of cancer: an American Society of Clinical oncology clinical practice guideline adaptation. J Clin Oncol 32(17):1840–1850
Butt Z, Rosenbloom SK, Abernethy AP et al (2008) Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. J Natl Compr Canc Netw 6(5):448–455
Yi JC, Syrjala KL (2017) Anxiety and Depression in Cancer Survivors. The Medical Clinics of North America 101(6):1099–1113
Ganz PA, Bower JE (2007) Cancer related fatigue: a focus on breast cancer and Hodgkin’s disease survivors. Acta Oncol 46(4):474–479
Minton O, Stone P (2008) How common is fatigue in disease-free breast cancer survivors? A systematic review of the literature. Breast Cancer Res Treat 112(1):5–13
Puigpinos-Riera R, Graells-Sans A, Serral G et al (2018) Anxiety and depression in women with breast cancer: Social and clinical determinants and influence of the social network and social support (DAMA cohort). Cancer Epidemiol 55:123–129
Saboonchi F, Petersson LM, Wennman-Larsen A et al (2014) Changes in caseness of anxiety and depression in breast cancer patients during the first year following surgery: patterns of transiency and severity of the distress response. Eur J Oncol Nurs 18(6):598–604
Tsaras K, Papathanasiou IV, Mitsi D et al (2018) Assessment of Depression and Anxiety in Breast Cancer Patients: Prevalence and Associated Factors. Asian Pac J Cancer Prev 19(6):1661–1669
Ancoli-Israel S, Liu L, Rissling M et al (2014) Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer 22(9):2535–2545
Curt GA (2000) Impact of fatigue on quality of life in oncology patients. Semin Hematol 37(4 Suppl 6):14–17
Wolvers MDJ, Leensen MCJ, Groeneveld IF et al (2018) Predictors for earlier return to work of cancer patients. J Cancer Surviv 12(2):169–177
Lee MK, Kang HS, Lee KS et al (2017) Three-Year Prospective Cohort Study of Factors Associated with Return to Work After Breast Cancer Diagnosis. J Occup Rehabil 27(4):547–558
Bower JE, Ganz PA, Desmond KA et al (2000) Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol 18(4):743–753
Stein KD, Jacobsen PB, Blanchard CM et al (2004) Further validation of the multidimensional fatigue symptom inventory-short form. J Pain Symptom Manage 27(1):14–23
Morris G, Anderson G, Maes M (2017) Hypothalamic-Pituitary-Adrenal Hypofunction in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS) as a Consequence of Activated Immune-Inflammatory and Oxidative and Nitrosative Pathways. Mol Neurobiol 54(9):6806–6819
Bower JE (2019) The role of neuro-immune interactions in cancer-related fatigue: Biobehavioral risk factors and mechanisms. Cancer 125(3):353–364
Bower JE, Ganz PA, Aziz N et al (2002) Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med 64(4):604–611
Janelsins MC, Heckler CE, Peppone LJ et al (2018) Longitudinal Trajectory and Characterization of Cancer-Related Cognitive Impairment in a Nationwide Cohort Study. J Clin Oncol. https://doi.org/10.1200/jco.2018.78.6624:Jco2018786624
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA (1983) Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press, Palo Alto, CA
Addolorato G, Ancona C, Capristo E et al (1999) State and trait anxiety in women affected by allergic and vasomotor rhinitis. J Psychosom Res 46(3):283–289
Cella DF, Tulsky DS, Gray G et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
Gerber LH, Stout N, McGarvey C et al (2011) Factors predicting clinically significant fatigue in women following treatment for primary breast cancer. Support Care Cancer 19(10):1581–1591
Inglis JE, Janelsins MC, Culakova E et al (2019) Longitudinal assessment of the impact of higher body mass index on cancer-related fatigue in patients with breast cancer receiving chemotherapy. Support Care Cancer. https://doi.org/10.1007/s00520-019-04953-4
Tsaras K, Papathanasiou IV, Mitsi D et al (2018) Assessment of Depression and Anxiety in Breast Cancer Patients: Prevalence and Associated Factors. Asian Pacific journal of cancer prevention : APJCP 19(6):1661–1669
Janelsins MC, Heckler CE, Peppone LJ et al (2017) Cognitive Complaints in Survivors of Breast Cancer After Chemotherapy Compared With Age-Matched Controls: An Analysis From a Nationwide, Multicenter. Prospective Longitudinal Study J Clin Oncol 35(5):506–514
Chan A, Yo TE, Wang XJ et al (2018) Minimal Clinically Important Difference of the Multidimensional Fatigue Symptom Inventory-Short Form (MFSI-SF) for Fatigue Worsening in Asian Breast Cancer Patients. J Pain Symptom Manage 55(3):992-997.e2
Liu L, Rissling M, Neikrug A et al (2013) Fatigue and Circadian Activity Rhythms in Breast Cancer Patients Before and After Chemotherapy: A Controlled Study. Fatigue 1(1–2):12–26
Villar RR, Fernandez SP, Garea CC et al (2017) Quality of life and anxiety in women with breast cancer before and after treatment. Rev Lat Am Enfermagem 25:e2958
Ng CG, Mohamed S, See MH et al (2015) Anxiety, depression, perceived social support and quality of life in Malaysian breast cancer patients: a 1-year prospective study. Health Qual Life Outcomes 13:205
Kyranou M, Puntillo K, Dunn LB et al (2014) Predictors of initial levels and trajectories of anxiety in women before and for 6 months after breast cancer surgery. Cancer Nurs 37(6):406–417
Davis LE, Bubis LD, Mahar AL et al (2018) Patient-reported symptoms after breast cancer diagnosis and treatment: A retrospective cohort study. Eur J Cancer 101:1–11
Hopwood P, Sumo G, Mills J et al (2010) The course of anxiety and depression over 5 years of follow-up and risk factors in women with early breast cancer: results from the UK Standardisation of Radiotherapy Trials (START). Breast 19(2):84–91
Saboonchi F, Petersson LM, Wennman-Larsen A et al (2015) Trajectories of Anxiety Among Women with Breast Cancer: A Proxy for Adjustment from Acute to Transitional Survivorship. J Psychosoc Oncol 33(6):603–619
Kreukels BP, van Dam FS, Ridderinkhof KR et al (2008) Persistent neurocognitive problems after adjuvant chemotherapy for breast cancer. Clin Breast Cancer 8(1):80–87
Fries E, Hesse J, Hellhammer J et al (2005) A new view on hypocortisolism. Psychoneuroendocrinology 30(10):1010–1016
Chaudhuri A, Behan PO (2004) Fatigue in neurological disorders. Lancet 363(9413):978–988
Dumas A, Luis IMVD, Bovagnet T, et al. Return to work after breast cancer: Comprehensive longitudinal analyses of its determinants. Journal of Clinical Oncology 2019;37(15_suppl):11564–11564.
Lindbohm ML, Kuosma E, Taskila T et al (2014) Early retirement and non-employment after breast cancer. Psychooncology 23(6):634–641
Bower JE, Asher A, Garet D et al (2019) Testing a biobehavioral model of fatigue before adjuvant therapy in women with breast cancer. Cancer 125(4):633–641
Mustian KM, Alfano CM, Heckler C et al (2017) Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue: A Meta-analysis. JAMA Oncol 3(7):961–968
Kleckner IR, Dunne RF, Asare M et al (2018) Exercise for Toxicity Management in Cancer-A Narrative Review. Oncol Hematol Rev 14(1):28–37
Liu L, Mills PJ, Rissling M et al (2012) Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun 26(5):706–713
Roscoe JA, Kaufman ME, Matteson-Rusby SE et al (2007) Cancer-related fatigue and sleep disorders. Oncologist 12(Suppl 1):35–42
Ancoli-Israel S, Moore PJ, Jones V (2001) The relationship between fatigue and sleep in cancer patients: a review. Eur J Cancer Care (Engl) 10(4):245–255
Berger AM, Kuhn BR, Farr LA et al (2009) Behavioral therapy intervention trial to improve sleep quality and cancer-related fatigue. Psychooncology 18(6):634–646
Wu LM, Amidi A, Valdimarsdottir H et al (2018) The Effect of Systematic Light Exposure on Sleep in a Mixed Group of Fatigued Cancer Survivors. J Clin Sleep Med 14(1):31–39
Kroenke CH, Rosner B, Chen WY et al (2004) Functional impact of breast cancer by age at diagnosis. J Clin Oncol 22(10):1849–1856
Andrykowski MA, Donovan KA, Laronga C et al (2010) Prevalence, predictors, and characteristics of off-treatment fatigue in breast cancer survivors. Cancer 116(24):5740–5748
Bower JE, Ganz PA, Desmond KA et al (2006) Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer 106(4):751–758
Alfano CM, Imayama I, Neuhouser ML et al (2012) Fatigue, inflammation, and omega-3 and omega-6 fatty acid intake among breast cancer survivors. J Clin Oncol 30(12):1280–1287
Acknowledgments
This work was supported by grants from the National Institutes of Health (DP2CA195765 to M.C.J.) and the National Cancer Institute at the National Institutes of Health (F99CA222742 to A.M.W., R01CA231014 to M.C.J.). We thank the participants in this study and all staff at the University of Rochester Cancer Center National Cancer Institute (NCI) Community Clinical Oncology Research Program (NCORP) Research Base and our NCORP affiliate sites who recruited and observed participants. We thank the National Cancer Institute Clinical Community Oncology Program (CCOP) and NCORP programs for their funding and support of this project. The following CCOP/NCORPs participated in this study: Central Illinois, Columbus, Cancer Research Consortium of West Michigan, Dayton, Delaware, Grand Rapids, Greenville, Hematology-Oncology Associates of Central New York, Kalamazoo, Kansas City, Marshfield, Metro Minnesota, Nevada, North Shore, Pacific Cancer Research Consortium, Southeast Cancer Control Consortium, Southeast Clinical Oncology Research Consortium, Upstate Carolina, Virginia Mason, Wichita, Wisconsin NCORP, and Western Oncology Research Consortium.
Funding
This work was supported by grants from the National Institutes of Health (DP2CA195765 to M.C.J.) and the National Cancer Institute at the National Institutes of Health (F99CA222742 to A.M.W., R01CA231014 to M.C.J.).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest. The role of the funder: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decisions to submit the manuscript for publication.
Ethical approval
This study was approved by the Institutional Review Board of the University of Rochester Cancer Center NCORP Research Base and each NCORP location; the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to Participate
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Williams, A.M., Khan, C.P., Heckler, C.E. et al. Fatigue, anxiety, and quality of life in breast cancer patients compared to non-cancer controls: a nationwide longitudinal analysis. Breast Cancer Res Treat 187, 275–285 (2021). https://doi.org/10.1007/s10549-020-06067-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06067-6