Abstract
Purpose
Few studies have reported temporal and spatial trends of aggressive prostate cancer (PC) among black men who are known to have more aggressive disease. We examined these trends for highly aggressive PC at diagnosis among black and white men in Pennsylvania (PA).
Methods
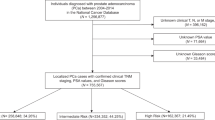
Men, aged ≥ 40 years, with a primary, clinical PC diagnosis were identified from the Pennsylvania Cancer Registry, 2004–2014. Joinpoint analysis was used to evaluate the temporal trend of highly aggressive PC (clinical/pathologic Gleason score ≥ 7 [4 + 3], clinical/pathologic tumor stage ≥ T3, or distant metastasis) and identify change points by race in which annual percent change (APC) was calculated. Logistic regression analyses were used to examine the association between race and highly aggressive PC, after adjusting for covariates with and without spatial dependence.
Results
There were 89,133 PC cases, which included 88.7% white and 11.3% black men. The APC of highly aggressive PC was 8.7% from 2011 to 2014 among white men and 3.6% from 2007 to 2014 among black men (p values ≤ 0.01). The greatest odds of having highly aggressive PC among black compared to white men were found in counties where the black male population was ≤ 5.3%.
Conclusions
Highly aggressive PC increased for both black and white men in PA between 2004 and 2014. Black men had more aggressive disease, with the greatest odds in counties where the black male population was small. The increase in highly aggressive PC may be due to less screening for PC, resulting in more advanced disease at diagnosis.


Similar content being viewed by others
References
ACS (2018) Cancer facts & figures 2018. American Cancer Society, Atlanta
Wood HM, Reuther AM, Gilligan TD, Kupelian PA, Modlin CS, Klein EA (2007) Rates of biochemical remission remain higher in black men compared to white men after radical prostatectomy despite similar trends in prostate specific antigen induced stage migration. J Urol 178(4):1271–1276
SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations) (2009) National Cancer Institute. Accessed 2012
Godley PA, Schenck AP, Amamoo MA, Schoenbach VJ, Peacock S, Manning M, Symons M, Talcott JA (2003) Racial differences in mortality among Medicare recipients after treatment for localized prostate cancer. J Natl Cancer Inst 95(22):1702–1710
Bhardwaj A, Srivastava SK, Khan MA, Prajapati VK, Singh S, Carter JE, Singh AP (2017) Racial disparities in prostate cancer: a molecular perspective. Front Biosci (Landmark edition) 22:772–782
SEER Cancer Statistics Review, 1975–2016 (2018) National Cancer Institute. https://seer.cancer.gov/csr/1975_2016/. Accessed 9 Feb 2019
Kelly SP, Anderson WF, Rosenberg PS, Cook MB (2018) Past, current, and future incidence rates and burden of metastatic prostate cancer in the United States. Eur Urol Focus 4(1):121–127. https://doi.org/10.1016/j.euf.2017.10.014
Gejerman G, Ciccone P, Goldstein M, Lanteri V, Schlecker B, Sanzone J, Esposito M, Rome S, Ciccone M, Margolis E, Simon R, Guo Y, Pentakota SR, Sadhegi-Nejad H (2017) US Preventive Services Task Force prostate-specific antigen screening guidelines result in higher Gleason score diagnoses. Investig Clin Urol 58(6):423–428. https://doi.org/10.4111/icu.2017.58.6.423
Weiner AB, Matulewicz RS, Eggener SE, Schaeffer EM (2016) Increasing incidence of metastatic prostate cancer in the United States (2004–2013). Prostate Cancer Prostatic Dis 19(4):395–397. https://doi.org/10.1038/pcan.2016.30
Bureau USC (2010) Geographic terms and concepts—urban and rural, 2017. https://www.census.gov/geo/reference/gtc/gtc_urbanrural.html
Kim HJ, Fay MP, Feuer EJ, Midthune DN (2000) Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 19(3):335–351
Rodrigues M, de la Riva J, Fotheringham S (2014) Modeling the spatial variation of the explanatory factors of human-caused wildfires in Spain using geographically weighted logistic regression. Appl Geogr 48:52–63. https://doi.org/10.1016/j.apgeog.2014.01.011
Cardozo OD, García-Palomares JC, Gutiérrez J (2012) Application of geographically weighted regression to the direct forecasting of transit ridership at station-level. Appl Geogr 34:548–558. https://doi.org/10.1016/j.apgeog.2012.01.005
Chen D-R, Truong K (2012) Using multilevel modeling and geographically weighted regression to identify spatial variations in the relationship between place-level disadvantages and obesity in Taiwan. Appl Geogr 32(2):737–745. https://doi.org/10.1016/j.apgeog.2011.07.018
Chi G, Wang D (2016) Small-area population forecasting: a geographically weighted regression approach. In: Swanson D (ed) The frontiers of applied demography. Springer, New York, pp 449–471
Team RC (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Institute ESR (2009) ArcGIS Desktop Help 9.3 Geostatistical Analyst. Redlands, CA
Bureau USC (2018) Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2017 U.S. Census Bureau, Population Division. https://www.census.gov/data/datasets/2017/demo/popest/counties-detail.html. Accessed 1/18/19 2019
DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, Jemal A (2016) Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA 66(4):290–308. https://doi.org/10.3322/caac.21340
Health PDo (2017) Cancer facts and figures Pennsylvania, 2017 (trans: Informatics DoH). Pennsylvania Department of Health, Harrisburg, PA
Wang M, Matthews SA, Iskandarani K, Li Y, Li Z, Chinchilli VM, Zhang L (2017) Spatial-temporal analysis of prostate cancer incidence from the Pennsylvania Cancer Registry, 2000–2011. Geospat Health 12(2):611. https://doi.org/10.4081/gh.2017.611
Reese AC, Wessel SR, Fisher SG, Mydlo JH (2016) Evidence of prostate cancer “reverse stage migration” toward more advanced disease at diagnosis: data from the Pennsylvania Cancer Registry. Urol Oncol 34(8):e321–e328. https://doi.org/10.1016/j.urolonc.2016.03.014
Calonge N, Petitti DB, Dewitt TG, Dietrich AJ, Gregory KD, Harris R, Isham GJ, Lefevre ML, Leipzig R, Loveland-Cherry C, Marion LN (2008) Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 149(3):185–191
Moyer VA (2012) Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 157 (2):120–134. https://doi.org/10.7326/0003-4819-157-2-201207170-00459
Downer MK, Stampfer MJ, Cooperberg MR (2017) Declining incidence rates of prostate cancer in the United States: is this good news or not? JAMA Oncol 3(12):1623–1624. https://doi.org/10.1001/jamaoncol.2017.0470
Jemal A, Ward E, Wu X, Martin HJ, McLaughlin CC, Thun MJ (2005) Geographic patterns of prostate cancer mortality and variations in access to medical care in the United States. Cancer Epidemiol Biomark Prev 14(3):590–595. https://doi.org/10.1158/1055-9965.epi-04-0522
Ong MS, Mandl KD (2017) Trends in prostate-specific antigen screening and prostate cancer interventions 3 years after the U.S. Preventive Services Task Force Recommendation. Ann Intern Med 166(6):451–452. https://doi.org/10.7326/l16-0422
Network ACC (2009) The Cancer Burden in Appalachia.
Commission AR (2019) The Appalachian Region. Appalachia Regional Commission. https://www.arc.gov/appalachian_region/TheAppalachianRegion.asp
Antwi S, Tucker TC, Coker AL, Fleming ST (2013) Racial disparities in survival after diagnosis of prostate cancer in Kentucky, 2001–2010. Am J Men's Health 7(4):306–316. https://doi.org/10.1177/1557988312473774
Acknowledgments
A special thanks to James Rubertone for data extraction and other inquiries related to the Pennsylvania Cancer Registry.
Funding
This study was supported by The Eberly Medical Research Endowment Innovation Fund at the Pennsylvania State University College of Medicine, The Pennsylvania State Clinical and Translational Science Institute (CTSI) Novel Methodologies in Health Research (5 UL1 RR0330184-04), and Highmark Incorporation Grant at Penn State Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This study used existing data which allowed to waive informed consent and was approved by the Pennsylvania Department of Health and the Institutional Review Board of The Pennsylvania State College of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, M., Chi, G., Bodovski, Y. et al. Temporal and spatial trends and determinants of aggressive prostate cancer among Black and White men with prostate cancer. Cancer Causes Control 31, 63–71 (2020). https://doi.org/10.1007/s10552-019-01249-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01249-0