Abstract
Purpose
The Risk of Pediatric and Adolescent Cancer Associated with Medical Imaging (RIC) Study is quantifying the association between cumulative radiation exposure from fetal and/or childhood medical imaging and subsequent cancer risk. This manuscript describes the study cohorts and research methods.
Methods
The RIC Study is a longitudinal study of children in two retrospective cohorts from 6 U.S. healthcare systems and from Ontario, Canada over the period 1995–2017. The fetal-exposure cohort includes children whose mothers were enrolled in the healthcare system during their entire pregnancy and followed to age 20. The childhood-exposure cohort includes children born into the system and followed while continuously enrolled. Imaging utilization was determined using administrative data. Computed tomography (CT) parameters were collected to estimate individualized patient organ dosimetry. Organ dose libraries for average exposures were constructed for radiography, fluoroscopy, and angiography, while diagnostic radiopharmaceutical biokinetic models were applied to estimate organ doses received in nuclear medicine procedures. Cancers were ascertained from local and state/provincial cancer registry linkages.
Results
The fetal-exposure cohort includes 3,474,000 children among whom 6,606 cancers (2394 leukemias) were diagnosed over 37,659,582 person-years; 0.5% had in utero exposure to CT, 4.0% radiography, 0.5% fluoroscopy, 0.04% angiography, 0.2% nuclear medicine. The childhood-exposure cohort includes 3,724,632 children in whom 6,358 cancers (2,372 leukemias) were diagnosed over 36,190,027 person-years; 5.9% were exposed to CT, 61.1% radiography, 6.0% fluoroscopy, 0.4% angiography, 1.5% nuclear medicine.
Conclusion
The RIC Study is poised to be the largest study addressing risk of childhood and adolescent cancer associated with ionizing radiation from medical imaging, estimated with individualized patient organ dosimetry.


Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to institutional data sharing policies and are available from the corresponding author upon reasonable request as well as appropriate institutional review board approvals and data sharing agreements.
Code availability
Not applicable.
References
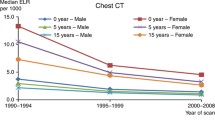
Smith-Bindman R et al (2012) Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 307(22):2400–2409
Smith-Bindman R et al (2019) Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000–2016. JAMA 322(9):843–856
BEIR VII (2006) Health risks from exposure to low levels of ionizing radiation, in Committee to Assess Health Effects from Exposure to Low Levels of Ionizing Radiation. National Research Council, Washington, DC
Pearce MS et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380(9840):499–505
Preston DL et al (2008) Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428–436
Siegel RL et al (2021) Cancer Statistics, 2021. CA Cancer J Clin 71(1):7–33
https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
Hong JY et al (2019) Association of exposure to diagnostic low-dose ionizing radiation with risk of cancer among youths in South Korea. JAMA Netw Open 2(9):e1910584
Mathews JD et al (2013) Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360
Meulepas JM et al (2018) Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst 111:256–263
Kwan ML et al (2019) Trends in medical imaging during pregnancy in the United States and Ontario, Canada, 1996 to 2016. JAMA Netw Open 2(7):e197249
Ross TR et al (2014) The HMO research network virtual data warehouse: a public data model to support collaboration. EGEMS (Wash DC) 2(1):1049
Hornbrook MC et al (2005) Building a virtual cancer research organization. J Natl Cancer Inst Monogr 35:12–25
https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm
https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas-who.htm
Fenton TR, Kim JH (2013) A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr 13:59
Chen K, Zhang X, Petersen A, Muller H-G (2017) Quantifying infinite-dimensional data: functional data analysis in action. Stat Biosci 9:582–604
Geyer AM et al (2014) The UF/NCI family of hybrid computational phantoms representing the current US population of male and female children, adolescents, and adults–application to CT dosimetry. Phys Med Biol 59(18):5225–5242
Maynard MR et al (2011) The UF family of hybrid phantoms of the developing human fetus for computational radiation dosimetry. Phys Med Biol 56(15):4839–4879
Maynard MR et al (2014) The UF Family of hybrid phantoms of the pregnant female for computational radiation dosimetry. Phys Med Biol 59(15):4325–4343
Stepusin EJ et al (2017) Physical validation of a Monte Carlo-based, phantom-derived approach to computed tomography organ dosimetry under tube current modulation. Med Phys 44(10):5423–5432
Stepusin EJ et al (2017) Assessment of different patient-to-phantom matching criteria applied in Monte Carlo-based computed tomography dosimetry. Med Phys 44(10):5498–5508
Marshall EL et al (2019) A scalable database of organ doses for common diagnostic fluoroscopy procedures of children: procedures of historical practice for use in radiation epidemiology studies. Radiat Res 192(6):649–661
McCollough CH et al (2007) Radiation exposure and pregnancy: when should we be concerned? Radiographics 27(4):909–917
https://www.unscear.org/docs/publications/2000/UNSCEAR_2000_Annex-D.pdf
Niwa O et al (2015) ICRP publication 131: stem cell biology with respect to carcinogenesis aspects of radiological protection. Ann ICRP 44(3–4):7–357
Stabin MG (2018) New-generation fetal dose estimates for radiopharmaceuticals. J Nucl Med 59(6):1005–1006
https://seer.cancer.gov/siterecode/icdo3_dwhoheme/index.html
Steliarova-Foucher E et al (2005) International classification of childhood cancer, third edition. Cancer 103(7):1457–1467
Hasle H, Clemmensen IH, Mikkelsen M (2000) Risks of leukaemia and solid tumours in individuals with Down’s syndrome. Lancet 355(9199):165–169
Marlow EC et al (2021) Leukemia risk in a cohort of 3.9 million children with and without Down syndrome. J Pediatr 234:172
Buffler PA et al (2005) Environmental and genetic risk factors for childhood leukemia: appraising the evidence. Cancer Invest 23(1):60–75
Poole C et al (2006) Socioeconomic status and childhood leukaemia: a review. Int J Epidemiol 35(2):370–384
Chow EJ et al (2010) Childhood cancer in relation to parental race and ethnicity: a 5-state pooled analysis. Cancer 116(12):3045–3053
Lim JY et al (2014) Genomics of racial and ethnic disparities in childhood acute lymphoblastic leukemia. Cancer 120(7):955–962
Linabery AM, Ross JA (2008) Trends in childhood cancer incidence in the U.S. (1992–2004). Cancer 112(2):416–432
Messer LC et al (2006) The development of a standardized neighborhood deprivation index. J Urban Health 83(6):1041–1062
Gooley TA et al (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18(6):695–706
Miglioretti DL et al (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 167(8):700–707
Grant EJ et al (2017) Solid Cancer Incidence among the Life Span Study of Atomic Bomb Survivors: 1958–2009. Radiat Res 187(5):513–537
Moysich KB, Menezes RJ, Michalek AM (2002) Chernobyl-related ionising radiation exposure and cancer risk: an epidemiological review. Lancet Oncol 3(5):269–279
Hauptmann M et al (2016) Increased pancreatic cancer risk following radiotherapy for testicular cancer. Br J Cancer 115(7):901–908
Levi F et al (2006) Cancer risk after radiotherapy for breast cancer. Br J Cancer 95(3):390–392
Huang WY et al (2014) Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer 110(9):2354–2360
Bernier MO et al (2018) Cohort Profile: the EPI-CT study: a European pooled epidemiological study to quantify the risk of radiation-induced cancer from paediatric CT. Int J Epidemiol 48:379
Krille L et al (2015) Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: results from a German cohort study. Radiat Environ Biophys 54(1):1–12
Journy N et al (2015) Are the studies on cancer risk from CT scans biased by indication? Elements of answer from a large-scale cohort study in France. Br J Cancer 112(1):185–193
Boice JD Jr (2015) Radiation epidemiology and recent paediatric computed tomography studies. Ann ICRP 44(1 Suppl):236–248
Walsh L et al (2014) Risks from CT scans–what do recent studies tell us? J Radiol Prot 34(1):E1-5
Acknowledgments
We thank Dr. Jonathan Ducore, MD, MPH and Dr. Stacy Month, MD for their pediatric oncology consultation in reviewing our classification of childhood cancers. We also thank our study staff who performed film CT abstraction and database programming support: Zobeyda Otero, Aleyda Solorzano Pinto, Kiara Bell, Andrea Volz, Mary Lyons, Donna Gleason, Arthur Truong, Ali Moin, Mohammed Mamun, Diane Kohnhorst, and Deborah Seger.
Funding
This study was supported by the National Cancer Institute at the National Institutes of Health (R01CA185687 and R50CA211115). The Ontario, Canada portion of the study was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission: (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by institutional review boards at each participating study site. Given this is a minimal risk, medical record review study, participant informed consent was waived.
Consent to participate
This study was approved by institutional review boards at each participating study site. Given this is a minimal risk, medical record review study, participant informed consent was waived.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kwan, M.L., Miglioretti, D.L., Bowles, E.J.A. et al. Quantifying cancer risk from exposures to medical imaging in the Risk of Pediatric and Adolescent Cancer Associated with Medical Imaging (RIC) Study: research methods and cohort profile. Cancer Causes Control 33, 711–726 (2022). https://doi.org/10.1007/s10552-022-01556-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-022-01556-z