Abstract
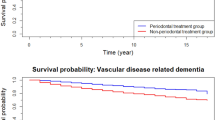
Periodontal disease (PD) is common and increases cardiovascular diseases. However, it is unclear whether PD is associated with increased risk of dementia. We carried out a systematic review and meta-analysis to investigate the influence of PD on dementia. We projected the number of dementia cases to be saved by reducing PD prevalence in the world. We searched cohort and case–control studies reporting the association of PD with all dementia (or any specific type of dementia) through PubMed, MEDLINE, PsycINFO, SocINDEX, CINHAL, and CNKI until 7th November 2018. Five cohorts and seven case–control studies were identified for review. We pooled eligible data to calculate relative risk (RR) of dementia in relation to PD and computed the number of dementia cases saved through reducing PD prevalence. Of 12 studies, six were undertaken in Asia, four in Europe and two in America. Eleven studies showed a positive association between PD and the risk of dementia, of which 10 were significant, and one reported a non-significant inverse association. Overall their quality was good. Pooled RR of dementia in relation to PD from all high quality studies was 1.38 (95%CI 1.01–1.90); in the five cohorts was 1.18 (1.06–1.31) and in the two case–control studies 2.25 (1.48–3.42). A 50% reduction in the current prevalence of 20% of PD in the population could save 850,000 (630,000–1,420,000) patients with dementia in the world. PD could increase the risk of incident dementia. Preventing and treating PD could contribute to controlling the global epidemic of dementia.



Similar content being viewed by others
References
Van Dyke TE, Van Winkelhoff AJ. Infection and inflammatory mechanisms. J Clin Periodontol. 2013;40:S1–7. https://doi.org/10.1111/jcpe.12088.
Kassebaum N, Bernabé E, Dahiya M, Bhandari B, Murray C, Marcenes W. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res. 2014;93(11):1045–53. https://doi.org/10.1177/0022034514552491.
Schätzle M, Faddy MJ, Cullinan MP, Seymour GJ, Lang NP, Bürgin W, et al. The clinical course of chronic periodontitis: V. Predictive factors in periodontal disease. J Clin Periodontol. 2009;36(5):365–71. https://doi.org/10.1111/j.1600-051X.2009.01391.x.
Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809–20. https://doi.org/10.1016/S0140-6736(05)67728-8.
Hansen GM, Egeberg A, Holmstrup P, Hansen PR. Relation of periodontitis to risk of cardiovascular and all-cause mortality (from a Danish nationwide cohort study). Am J Cardiol. 2016;118(4):489–93. https://doi.org/10.1016/j.amjcard.2016.05.036.
Lee YT, Lee HC, Hu CJ, Huang LK, Chao SP, Lin CP, et al. Periodontitis as a modifiable risk factor for dementia: a nationwide population-based cohort study. J Am Geriatr Soc. 2017;65(2):301–5. https://doi.org/10.1111/jgs.14449.
Lee YL, Hu HY, Huang LY, Chou P, Chu D. Periodontal disease associated with higher risk of dementia: population-based cohort study in Taiwan. J Am Geriatr Soc. 2017;65(9):1975–80. https://doi.org/10.1111/jgs.14944.
Chen C-K, Wu Y-T, Chang Y-C. Association between chronic periodontitis and the risk of Alzheimer’s disease: a retrospective, population-based, matched-cohort study. Alzheimers Res Ther. 2017;9(1):56. https://doi.org/10.1186/s13195-017-0282-6.
Tzeng NS, Chung CH, Yeh CB, Huang RY, Yuh DY, Huang SY, et al. Are chronic periodontitis and gingivitis associated with dementia? A nationwide, retrospective, matched-cohort study in Taiwan. Neuroepidemiol. 2016;47(2):82–93. https://doi.org/10.1159/000449166.
Arrivé E, Letenneur L, Matharan F, Laporte C, Helmer C, Barberger-Gateau P, et al. Oral health condition of French elderly and risk of dementia: a longitudinal cohort study. Community Dent Oral Epidemiol. 2012;40(3):230–8. https://doi.org/10.1111/j.1600-0528.2011.00650.x.
Leira Y, Domínguez C, Seoane J, Seoane-Romero J, Pías-Peleteiro JM, Takkouche B, et al. Is periodontal disease associated with Alzheimer’s disease? A systematic review with meta-analysis. Neuroepidemiology. 2017;48(1–2):21–31. https://doi.org/10.1159/000458411.
Kapellas K, Ju X, Wang X, Mueller N, Jamieson LM. The association between periodontal disease and dementia: a systematic review and meta-analysis. Dent Oral Biol Craniofac Res. 2019. https://doi.org/10.31487/j.dobcr.2019.01.005.
Syrjälä AM, Ylöstalo P, Ruoppi P, Komulainen K, Hartikainen S, Sulkava R, et al. Dementia and oral health among subjects aged 75 years or older. Gerodontology. 2012;29(1):36–42. https://doi.org/10.1111/j.1741-2358.2010.00396.x.
Iwasaki M, Kimura Y, Ogawa H, Yamaga T, Ansai T, Wada T, et al. Periodontitis, periodontal inflammation, and mild cognitive impairment: a 5-year cohort study. J Periodontal Res. 2018. https://doi.org/10.1111/jre.12623.
Chan KY, Wang W, Wu JJ, Liu L, Theodoratou E, Car J, et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. The Lancet. 2013;381(9882):2016–23. https://doi.org/10.1016/S0140-6736(13)60221-4.
Chen R, Hu Z, Chen R-L, Zhang D, Xu L, Wang J, et al. Socioeconomic deprivation and survival after stroke in China: a systematic literature review and a new population-based cohort study. BMJ Open. 2015;5(1):e005688. https://doi.org/10.1136/bmjopen-2014-005688.
Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. BMJ. 2009. https://doi.org/10.1136/bmj.b2700.
Bramanti E, Bramanti A, Matacena G, Bramanti P, Rizzi A, Cicciu M. Clinical evaluation of the oral health status in vascular-type dementia patients. A case-control study. Minerva Stomatol. 2015;64(4):167–75.
Jureti R, Yiru W, Panlong H, Yue S, Awuti G. Survey on periodontal health status of Xinjiang Uygur and Han patients with Alzheimer’s disease. J Chongqing Med Univ. 2016;41(12):1267–71.
Holmer J, Eriksdotter M, Schultzberg M, Pussinen PJ, Buhlin K. Association between periodontitis and risk of Alzheimer’s disease, mild cognitive impairment and subjective cognitive decline: a case–control study. J Clin Periodontol. 2018. https://doi.org/10.1111/jcpe.13016.
Gil-Montoya JA, Sanchez-Lara I, Carnero-Pardo C, Fornieles F, Montes J, Vilchez R, et al. Is periodontitis a risk factor for cognitive impairment and dementia? A case-control study. J Periodontol. 2015;86(2):244–53. https://doi.org/10.1902/jop.2014.140340.
Stein PS, Steffen MJ, Smith C, Jicha G, Ebersole JL, Abner E, et al. Serum antibodies to periodontal pathogens are a risk factor for Alzheimer’s disease. Alzheimer’s Dementia J Alzheimer’s Dis. 2012;8(3):196–203. https://doi.org/10.1016/j.jalz.2011.04.006.
de Souza RT, Fabri GM, Nitrini R, Anghinah R, Teixeira MJ, de Siqueira JT, et al. Oral infections and orofacial pain in Alzheimer’s disease: a case-control study. J Alzheimers Dis. 2014;38(4):823–9. https://doi.org/10.3233/jad-131283.
Chu CH, Ng A, Chau AMH, Lo ECM. Oral health status of elderly chinese with dementia in Hong Kong. Oral Health Prevent Dent. 2015;13(1):51–7. https://doi.org/10.3290/j.ohpd.a32343.
Danat IM, Clifford A, Partridge M, Zhou W, Bakre AT, Chen A, et al. Impacts of overweight and obesity in older age on the risk of dementia: a systematic literature review and a meta-analysis. J Alzheimer’s Dis. 2019. https://doi.org/10.3233/jad-180763.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Zhang J, Kai FY. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1. https://doi.org/10.1001/jama.280.19.1690.
Bakre AT, Chen R, Khutan R, Wei L, Smith T, Qin G, et al. Association between fish consumption and risk of dementia: a new study from China and a systematic literature review and meta-analysis. Public Health Nutr. 2018;21(10):1921–32. https://doi.org/10.1017/S136898001800037X.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Barnes D, Yaffe K. The projected impact of risk factor reduction on Alzheimer’s disease prevalence. Alzheimer’s Dement J Alzheimer’s Assoc. 2011;7(4):S511. https://doi.org/10.1016/S1474-4422(11)70072-.
WHO (2017) Dementia: key facts. https://www.who.int/en/news-room/fact-sheets/detail/dementia. Accessed 25 Feb 2019.
Petersen PE, Ogawa H. Strengthening the prevention of periodontal disease: the WHO approach. J Periodontol. 2005;76(12):2187–93. https://doi.org/10.1902/jop.2005.76.12.2187.
Watts A, Crimmins EM, Gatz M. Inflammation as a potential mediator for the association between periodontal disease and Alzheimer’s disease. Neuropsychiatr Dis Treat. 2008;4(5):865–76. https://doi.org/10.2147/ndt.s3610.
Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5(1):eaau3333. https://doi.org/10.1126/sciadv.aau3333.
Ship JA. Oral health of patients with Alzheimer’s disease. J Am Dent Assoc. 1992;123(1):53–8. https://doi.org/10.14219/jada.archive.1992.0005.
Martande SS, Pradeep A, Singh SP, Kumari M, Suke DK, Raju AP, et al. Periodontal health condition in patients with Alzheimer’s disease. Am J Alzheimer’s Dis Other Dement. 2014;29(6):498–502. https://doi.org/10.1177/1533317514549650.
Jureti R. Survey on periodontal health status of Xinjiang Uygur and Han patients with Alzheimer’s diseases [Master]. Xinjiang Medical University; 2017.
Hill SB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300.
Chen J, Ren C-J, Wu L, Xia L-Y, Shao J, Leng W-D, et al. Tooth loss is associated with increased risk of dementia and with a dose-response relationship. Front Aging Neurosci. 2018;10:415. https://doi.org/10.3389/fnagi.2018.00415.
Janket S-J, Baird AE, Chuang S-K, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2003;95(5):559–69. https://doi.org/10.1067/moe.2003.107.
Leira Y, Seoane J, Blanco M, Rodriguez-Yanez M, Takkouche B, Blanco J, et al. Association between periodontitis and ischemic stroke: a systematic review and meta-analysis. Eur J Epidemiol. 2017. https://doi.org/10.1007/s10654-016-0170-6.
Anstey KJ, von Sanden C, Salim A, O’kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol. 2007;166(4):367–78. https://doi.org/10.1093/aje/kwm116.
Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol Comment. 2000;28(6):399–406. https://doi.org/10.1034/j.1600-0528.2000.028006399.x.
Kamer AR, Pirraglia E, Tsui W, Rusinek H, Vallabhajosula S, Mosconi L, et al. Periodontal disease associates with higher brain amyloid load in normal elderly. Neurobiol Aging. 2015;36(2):627–33. https://doi.org/10.1016/j.neurobiolaging.2014.10.038.
Pizzo G, Guiglia R, Russo LL, Campisi G. Dentistry and internal medicine: from the focal infection theory to the periodontal medicine concept. Eur J Intern Med. 2010;21(6):496–502. https://doi.org/10.1016/j.ejim.2010.07.011.
Carter CJ, France J, Crean S, Singhrao SK. The Porphyromonas gingivalis/host interactome shows enrichment in GWASdb genes related to Alzheimer’s disease, diabetes and cardiovascular diseases. Front Aging Neurosci. 2017;9:408. https://doi.org/10.3389/fnagi.2017.00408.
Newman AB, Fitzpatrick AL, Lopez O, Jackson S, Lyketsos C, Jagust W, et al. Dementia and Alzheimer’s disease incidence in relationship to cardiovascular disease in the Cardiovascular Health Study cohort. J Am Geriatr Soc. 2005;53(7):1101–7. https://doi.org/10.1111/j.1532-5415.2005.53360.x.
Fang W-l, Jiang M-j, Gu B-b, Wei Y-m, Fan S-n, Liao W, et al. Tooth loss as a risk factor for dementia: systematic review and meta-analysis of 21 observational studies. BMC Psychiatry. 2018;18(1):345. https://doi.org/10.1186/s12888-018-1927-0.
Kato T, Usami T, Noda Y, Hasegawa M, Ueda M, Nabeshima T. The effect of the loss of molar teeth on spatial memory and acetylcholine release from the parietal cortex in aged rats. Behav Brain Res. 1997;83(1–2):239–42. https://doi.org/10.1016/s0166-4328(97)86078-0.
Poole S, Singhrao SK, Kesavalu L, Curtis MA, Crean S. Determining the presence of periodontopathic virulence factors in short-term postmortem Alzheimer’s disease brain tissue. J Alzheimer’s Dis. 2013;36(4):665–77. https://doi.org/10.3233/JAD-121918.
Kawahata M, Ono Y, Ohno A, Kawamoto S, Kimoto K, Onozuka M. Loss of molars early in life develops behavioral lateralization and impairs hippocampus-dependent recognition memory. BMC Neurosci. 2014;15(1):4. https://doi.org/10.1186/1471-2202-15-4.
Ishida N, Ishihara Y, Ishida K, Tada H, Funaki-Kato Y, Hagiwara M, et al. Periodontitis induced by bacterial infection exacerbates features of Alzheimer’s disease in transgenic mice. NPJ Aging Mech Dis. 2017;3(1):15. https://doi.org/10.1038/s41514-017-0015-x.
Ilievski V, Zuchowska PK, Green SJ, Toth PT, Ragozzino ME, Le K, et al. Chronic oral application of a periodontal pathogen results in brain inflammation, neurodegeneration and amyloid beta production in wild type mice. PLoS ONE. 2018;13(10):e0204941. https://doi.org/10.1371/journal.pone.0204941.
Poole S, Singhrao SK, Chukkapalli S, Rivera M, Velsko I, Kesavalu L, et al. Active invasion of Porphyromonas gingivalis and infection-induced complement activation in ApoE-/-mice brains. J Alzheimers Dis. 2015;43(1):67–80. https://doi.org/10.3233/JAD-140315.
Kaye EK, Valencia A, Baba N, Spiro A III, Dietrich T, Garcia RI. Tooth loss and periodontal disease predict poor cognitive function in older men. J Am Geriatr Soc. 2010;58(4):713–8. https://doi.org/10.1111/j.1532-5415.2010.02788.x.
Acknowledgements
Professor Ruoling Chen and Dr Jie Tang thank an EU Grant from Horizon 2020 MSCA – DEMAIRPO #799247. Dr Kaarin Anstey is funded by NHMRC Fellowship #1102694. Dr Wu is the recipient of BBSRC [BB/P004695/1] and NIA [1R01AG049321-01A1] Grant for aging research. Dr Yuyou Yao, Associate Professor of Anhui Medical University, China is a visiting scholar at the Faculty of Education, Health and Wellbeing, University of Wolverhampton to support this study and has made valuable comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nadim, R., Tang, J., Dilmohamed, A. et al. Influence of periodontal disease on risk of dementia: a systematic literature review and a meta-analysis. Eur J Epidemiol 35, 821–833 (2020). https://doi.org/10.1007/s10654-020-00648-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-020-00648-x