Abstract
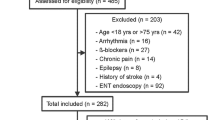
During the perioperative period, nociception control is certainly one of the anesthesiologist's main objectives when assuming care of a patient. There exists some literature demonstrating that the nociceptive stimuli experienced during surgery are responsible for peripheral and central sensitization phenomena, which can in turn lead to persistent postsurgical pain. An individualized approach to the evaluation and treatment of perioperative nociception is beneficial in order to avoid the sensitization phenomena that leads to prolonged postoperative pain and to minimize the consumption of opiates and their adverse effects. In terms of sensitivity, specificity, and positive/negative predictive values when compared to heart rate (HR) and mean arterial pressure (MAP), recent literature has shown that the NOL variation (ΔNOL) is the best index to distinguish noxious from non-noxious stimuli. Chronic treatment with β1-adrenergic antagonists may constitute a limitation to the use of the NOL index. β1-adrenergic antagonists induce a depressive action on the heart rate, which results in a limitation of its variability after a noxious stimulus. Since heart rate and heart rate variability are two parameters integrated into the NOL index, the validity of the NOL index in a population of patients receiving β1-adrenergic antagonists has not yet been determined. Our study sought to explore the NOL index, the BIS, and the heart rate variation in a group of patients under chronic treatment with β1-adrenergic antagonists submitted to standardized noxious stimulus under general anesthesia. We then compared those results to a control group of patients from our previous study (CJA group) that received no β1-adrenergic antagonist chronic treatment. The patients in this study were subjected to a standardized anesthetic protocol from induction up to 3 min after a standardized tetanic stimulus to the ulnar nerve at a frequency of 100 Hz and an amperage of 70 mA, for a duration of 30 s. Data were electronically recorded to obtain NOL, BIS, and heart rate values every 5 s for the duration of the protocol. The NOL maximal mean value reached after noxious stimulation was not different between our two cohorts (CJA: 30(14) versus BETANOL: 36(14) (p = 0.12)). There was no statistically significant difference between our cohorts in regards of the NOL AUC representing the variation of the NOL over a 180 s period (CJA: 595(356) versus BETANOL: 634(301) (p = 0.30)). However, a repeated measurement ANCOVA identified slight statistically significant differences between our cohorts in the peak of variation of the NOL index between 20 and 65 s after noxious stimulation, the NOL index of the cohort of beta-blocked patients being higher than the CJA patients. Moreover, the time to reach the maximum value was not different (CJA: 73(37) versus BETANOL: 63(41) (p = 0.35)). NOL sensitivity and specificity to detect a noxious stimulus under general anesthesia were similar in patients taking beta-blockers or not, and were better than those of heart rate and Bispectral index (AUC NOL 0.97, CI(0.92–1), versus AUC BIS 0.78, CI(0.64–0.89) and AUC HR 0.66, CI(0.5–0.8)). In conclusion, the NOL index is a reliable monitor to assess nociception in a population of patients under chronic beta-blocker therapy. Patients under such therapy achieve similar maximal NOL values over a 180 s period after a standardized noxious stimulus and the NOL variation over time, represented by the AUC is not significantly different from a cohort of non-beta-blocked patients. Whether the patient takes beta-blockers or not, sensitivity of the NOL index is greater than that seen for BIS index or heart rate to detect an experimental noxious stimulus under general anesthesia.




Similar content being viewed by others
References
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–25.
Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895–926.
Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3):S2-15.
Colvin LA, Bull F, Hales TG. Perioperative opioid analgesia-when is enough too much? A review of opioid-induced tolerance and hyperalgesia. Lancet. 2019;393:1558–68.
Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014;112(6):991–1004.
Guignard B, Bossard AE, Coste C, Sessler DI, Lebrault C, Alfonsi P, Fletcher D, Chauvin M. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000;93(2):409–17.
Joly V, Richebe P, Guignard B, Fletcher D, Maurette P, Sessler DI, Chauvin M. Remifentanil-induced postoperative hyperalgesia and its prevention with small-dose ketamine. Anesthesiology. 2005;103(1):147–55.
Shafi S, Collinsworth AW, Copeland LA, Ogola GO, Qiu T, Kouznetsova M, Liao IC, Mears N, Pham AT, Wan GJ, Masica AL. Association of opioid-related adverse drug events with clinical and cost outcomes among surgical patients in a large integrated health care delivery system. JAMA Surg. 2018;153(8):757–63.
Neuman MD, Bateman BT, Wunsch H. Inappropriate opioid prescription after surgery. Lancet. 2019;393:1547–57.
Page MG, Kudrina I, Zomahoun HTV, Croteau J, Ziegler D, Ngangue P, Martin E, Fortier M, Boisvert EE, Beaulieu P, Charbonneau C, Cogan J, Daoust R, Martel MO, Neron A, Richebe P, Clarke H. A systematic review of the relative frequency and risk factors for prolonged opioid prescription following surgery and trauma among adults. Ann Surg. 2020;271(5):845–54.
Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286–93.
Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, Bohnert ASB, Kheterpal S, Nallamothu BK. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504.
Koepke EJ, Manning EL, Miller TE, Ganesh A, Williams DGA, Manning MW. The rising tide of opioid use and abuse: the role of the anesthesiologist. Perioper Med (Lond). 2018;7:16.
Soffin EM, Lee BH, Kumar KK, Wu CL. The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth. 2019;122(6):e198–208.
Ellerkmann RK, Grass A, Hoeft A, Soehle M. The response of the composite variability index to a standardized noxious stimulus during propofol-remifentanil anesthesia. Anesth Analg. 2013;116(3):580–8.
Huiku M, Uutela K, van Gils M, Korhonen I, Kymalainen M, Merilainen P, Paloheimo M, Rantanen M, Takala P, Viertio-Oja H, Yli-Hankala A. Assessment of surgical stress during general anaesthesia. Br J Anaesth. 2007;98(4):447–55.
Storm H. Changes in skin conductance as a tool to monitor nociceptive stimulation and pain. Curr Opin Anaesthesiol. 2008;21(6):796–804.
Gruenewald M, Ilies C, Herz J, Schoenherr T, Fudickar A, Hocker J, Bein B. Influence of nociceptive stimulation on analgesia nociception index (ANI) during propofol-remifentanil anaesthesia. Br J Anaesth. 2013;110(6):1024–30.
Aissou M, Snauwaert A, Dupuis C, Atchabahian A, Aubrun F, Beaussier M. Objective assessment of the immediate postoperative analgesia using pupillary reflex measurement: a prospective and observational study. Anesthesiology. 2012;116(5):1006–12.
Sabourdin N, Barrois J, Louvet N, Rigouzzo A, Guye ML, Dadure C, Constant I. Pupillometry-guided intraoperative remifentanil administration versus standard practice influences opioid use: a randomized study. Anesthesiology. 2017;127(2):284–92.
Gruenewald M, Ilies C. Monitoring the nociception-anti-nociception balance. Best Pract Res Clin Anaesthesiol. 2013;27(2):235–47.
Ben-Israel N, Kliger M, Zuckerman G, Katz Y, Edry R. Monitoring the nociception level: a multi-parameter approach. J Clin Monit Comput. 2013;27(6):659–68.
Martini CH, Boon M, Broens SJ, Hekkelman EF, Oudhoff LA, Buddeke AW, Dahan A. Ability of the nociception level, a multiparameter composite of autonomic signals, to detect noxious stimuli during propofol-remifentanil anesthesia. Anesthesiology. 2015;123(3):524–34.
Stockle PA, Julien M, Issa R, Decary E, Brulotte V, Drolet P, Henri M, Poirier M, Latulippe JF, Dorais M, Verdonck O, Fortier LP, Richebe P. Validation of the PMD100 and its NOL Index to detect nociception at different infusion regimen of remifentanil in patients under general anesthesia. Minerva Anestesiol. 2018;84:1160. https://doi.org/10.23736/S0375-9393.18.12720-9.
Renaud-Roy E, Stockle PA, Maximos S, Brulotte V, Sideris L, Dube P, Drolet P, Tanoubi I, Issa R, Verdonck O, Fortier LP, Richebe P. Correlation between incremental remifentanil doses and the Nociception Level (NOL) index response after intraoperative noxious stimuli. Can J Anaesth. 2019;66(9):1049–61.
Edry R, Recea V, Dikust Y, Sessler DI. Preliminary intraoperative validation of the nociception level index: a noninvasive nociception monitor. Anesthesiology. 2016;125(1):193–203.
Edry R, Recea V, Dikust Y. NOL index performance in patients treated by beta-blockers. European Society of Anesthesiology meeting (ESA, Euroanesthesia) Geneva, Switzerland; 2017. p. 185888; 08AP05–12
Raft J, Coulombe MA, Renaud-Roy E, Tanoubi I, Verdonck O, Fortier LP, Espitalier F, Richebe P. Impact of intravenous phenylephrine bolus administration on the nociceptive level index (NOL). J Clin Monit Comput. 2019;34:1079.
Acknowledgements
Thanks to Nadia Godin, RN and Research Coordinator and Moulay Idrissi, BEng, MSc for their help in research organization. Thanks to Kyle Vaughn Roerick, editor, for his English language edition of this manuscript.
Funding
This study was fully supported by the department of anesthesiology and pain medicine of Maisonneuve-Rosemont Hospital, CIUSSS de l’Est de Montreal, University of Montreal.
Author information
Authors and Affiliations
Contributions
Study design: CB, VB, FP, AC, MEB, RI, RU, IT, PD, LPF, OV, AF, FE, PR. Recording data: CB, VB, FP, FE, PR. Interpreting data: CB, VB, FP, AC, MEB, RI, RU, IT, PD, LPF, OV, AF, FE, PR. Data analysis: CB, VB, AF, PR. Writing manuscript: CB, VB, PR. Reading and reviewing manuscript: CB, VB, FP, AC, MEB, RI, RU, IT, PD, LPF, OV, AF, FE, PR.
Corresponding author
Ethics declarations
Conflict of interest
CB, VB, FP, AC, MEB, RI, RU, IT, PD, LPF, OV, AF, FE declare no conflict of interest. P.R. received honorarium as a consultant from the following companies: Medasense, Abbvie, Medtronic-Covidien, Biosyent, Merck. He has been a member of the Scientific Advisory Board of Medasense Ltd. since 2014.
Ethics approval
The trial was conducted at the Maisonneuve-Rosemont University Hospital, University of Montreal, Montreal, QC, Canada. The recruitment was carried out from August 27, 2019 to March 4, 2020. Our research protocol was approved by our institution’s Research Ethics Committee (Comité d’Éthique de la Recherche, installation Hôpital Maisonneuve-Rosemont, CIUSS de l’Est de l’île de Montréal, Montréal, Qc, Canada; CER 2020-1946, August 12th 2019, see annexes). It was registered on clinicaltrial.gov (NCT04060095).
Informed consent
All patients gave written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bergeron, C., Brulotte, V., Pelen, F. et al. Impact of chronic treatment by β1-adrenergic antagonists on Nociceptive-Level (NOL) index variation after a standardized noxious stimulus under general anesthesia: a cohort study. J Clin Monit Comput 36, 109–120 (2022). https://doi.org/10.1007/s10877-020-00626-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00626-4