Abstract
Purpose
To assess long-term quality of life (QoL) in patients with sustained biochemical control of acromegaly, comparing those receiving vs not receiving pharmacotherapy (primary analysis); to assess change in QoL over time (secondary analysis).
Methods
Cross-sectional study, with a secondary longitudinal component, of 58 patients with biochemically controlled acromegaly. All had participated in studies assessing QoL years previously, after having undergone surgery ± radiotherapy. One cohort received medical therapy [MED (n = 33)]; the other did not [NO-MED (n = 25)]. QoL was assessed by the 36-Item-Short-Form Health Survey (SF-36), Acromegaly Quality of Life Questionnaire (AcroQoL), Gastrointestinal Quality of Life Index (GIQLI), Symptom Questionnaire, and QoL-Assessment of Growth Hormone Deficiency in Adults (QoL-AGHDA).
Results
Mean (± SD) duration of biochemical control was 15.0 ± 6.4 years for MED and 20.4 ± 8.2 years for NO-MED (p = 0.007). 58% of subjects scored < 25% of normal on ≥ 1 SF-36 domain and 32% scored < 25% of normal on ≥ 4 of 8 domains. Comparing MED vs NO-MED and controlling for duration of biochemical control, there were no significant differences in QoL by SF-36, AcroQOL, GIQLI, Symptom Questionnaire, or QoL-AGHDA. Growth hormone deficiency (GHD) but not radiotherapy predicted poorer QoL. In MED, QoL improved over time in three AcroQoL domains and two GIQLI domains. In NO-MED, QoL worsened in two SF-36 domains and two Symptom Questionnaire domains; QoL-AGHDA scores also worsened in subjects with GHD.
Conclusion
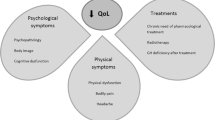
A history of acromegaly and development of GHD, but not pharmacologic or radiotherapy, are detrimental to QoL, which remains poor over the long-term despite biochemical control.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Kyriakakis N, Lynch J, Gilbey SG, Webb SM, Murray RD (2017) Impaired quality of life in patients with treated acromegaly despite long-term biochemically stable disease: results from a 5-years prospective study. Clin Endocrinol 86(6):806–815
Pantanetti P, Sonino N, Arnaldi G, Boscaro M (2002) Self image and quality of life in acromegaly. Pituitary 5(1):17–19
Trepp R, Everts R, Stettler C, Fischli S, Allemann S, Webb SM et al (2005) Assessment of quality of life in patients with uncontrolled vs. controlled acromegaly using the acromegaly quality of life questionnaire (acroqol). Clin Endocrinol 63(1):103–110
Paisley AN, Rowles SV, Roberts ME, Webb SM, Badia X, Prieto L et al (2007) Treatment of acromegaly improves quality of life, measured by acroqol. Clin Endocrinol 67(3):358–362
Matta MP, Couture E, Cazals L, Vezzosi D, Bennet A, Caron P (2008) Impaired quality of life of patients with acromegaly: control of gh/igf-i excess improves psychological subscale appearance. Eur J Endocrinol 158(3):305–310
Broersen LHA, Zamanipoor Najafabadi AH, Pereira AM, Dekkers OM, van Furth WR, Biermasz NR (2021) Improvement in symptoms and health-related quality of life in acromegaly patients: a systematic review and meta-analysis. J Clin Endocrinol Metab 106(2):577–587
Biermasz NR, van Thiel SW, Pereira AM, Hoftijzer HC, van Hemert AM, Smit JW et al (2004) Decreased quality of life in patients with acromegaly despite long-term cure of growth hormone excess. J Clin Endocrinol Metab 89(11):5369–5376
Biermasz NR, Pereira AM, Smit JW, Romijn JA, Roelfsema F (2005) Morbidity after long-term remission for acromegaly: persisting joint-related complaints cause reduced quality of life. J Clin Endocrinol Metab 90(5):2731–2739
Kauppinen-Makelin R, Sane T, Sintonen H, Markkanen H, Valimaki MJ, Loyttyniemi E et al (2006) Quality of life in treated patients with acromegaly. J Clin Endocrinol Metab 91(10):3891–3896
Guo X, Wang K, Yu S, Gao L, Wang Z, Zhu H et al (2021) Quality of life and its determinants in patients with treated acromegaly: a cross-sectional nationwide study in china. J Clin Endocrinol Metab 106(1):211–225
Pelsma ICM, Biermasz NR, van Furth WR, Pereira AM, Kroon HM, Kloppenburg M et al (2021) Progression of acromegalic arthropathy in long-term controlled acromegaly patients: 9 years of longitudinal follow-up. J Clin Endocrinol Metab 106(1):188–200
van der Klaauw AA, Biermasz NR, Hoftijzer HC, Pereira AM, Romijn JA (2008) Previous radiotherapy negatively influences quality of life during 4 years of follow-up in patients cured from acromegaly. Clin Endocrinol 69(1):123–128
Yoshida K, Fukuoka H, Matsumoto R, Bando H, Suda K, Nishizawa H et al (2015) The quality of life in acromegalic patients with biochemical remission by surgery alone is superior to that in those with pharmaceutical therapy without radiotherapy, using the newly developed Japanese version of the acroqol. Pituitary 18(6):876–883
Rowles SV, Prieto L, Badia X, Shalet SM, Webb SM, Trainer PJ (2005) Quality of life (qol) in patients with acromegaly is severely impaired: use of a novel measure of qol: acromegaly quality of life questionnaire. J Clin Endocrinol Metab 90(6):3337–3341
Wexler T, Gunnell L, Omer Z, Kuhlthau K, Beauregard C, Graham G et al (2009) Growth hormone deficiency is associated with decreased quality of life in patients with prior acromegaly. J Clin Endocrinol Metab 94(7):2471–2477
Postma MR, Netea-Maier RT, van den Berg G, Homan J, Sluiter WJ, Wagenmakers MA et al (2012) Quality of life is impaired in association with the need for prolonged postoperative therapy by somatostatin analogs in patients with acromegaly. Eur J Endocrinol 166(4):585–592
Tseng FY, Chen ST, Chen JF, Huang TS, Lin JD, Wang PW et al (2019) Correlations of clinical parameters with quality of life in patients with acromegaly: Taiwan acromegaly registry. J Formos Med Assoc Taiwan yi zhi 118(11):1488–1493
Ghajar A, Jones PS, Guarda FJ, Faje A, Tritos NA, Miller KK et al (2020) Biochemical control in acromegaly with multimodality therapies: outcomes from a pituitary center and changes over time. J Clin Endocrinol Metab 105(3):e532
Dichtel LE, Kimball A, Yuen KCJ, Woodmansee W, Haines MS, Guan QX et al (2021) Effects of growth hormone receptor antagonism and somatostatin analog administration on quality of life in acromegaly. Clin Endocrinol 94(1):58–65
McHorney CA, Ware JE Jr, Raczek AE (1993) The mos 36-item short-form health survey (sf-36): Ii. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31(3):247–263
Webb SM, Badia X, Surinach NL (2006) Validity and clinical applicability of the acromegaly quality of life questionnaire, acroqol: a 6-month prospective study. Eur J Endocrinol 155(2):269–277
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E et al (1995) Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg 82(2):216–222
Kellner R (1987) A symptom questionnaire. J Clin Psychiatry 48(7):268–274
McKenna SP, Doward LC, Alonso J, Kohlmann T, Niero M, Prieto L et al (1999) The qol-aghda: an instrument for the assessment of quality of life in adults with growth hormone deficiency. Qual Life Res 8(4):373–383
Arshad MF, Ogunleye O, Ross R, Debono M (2021) Surgically treated acromegaly patients have a similar quality of life whether controlled by surgery or requiring additional medical therapy (qualat study). Pituitary 24(5):768–777
Miller KK, Wexler T, Fazeli P, Gunnell L, Graham GJ, Beauregard C et al (2010) Growth hormone deficiency after treatment of acromegaly: a randomized, placebo-controlled study of growth hormone replacement. J Clin Endocrinol Metab 95(2):567–577
Feldt-Rasmussen U, Abs R, Bengtsson BA, Bennmarker H, Bramnert M, Hernberg-Ståhl E et al (2002) Growth hormone deficiency and replacement in hypopituitary patients previously treated for acromegaly or cushing’s disease. Eur J Endocrinol 146(1):67–74
Winther KH, Cramon P, Watt T, Bjorner JB, Ekholm O, Feldt-Rasmussen U et al (2016) Disease-specific as well as generic quality of life is widely impacted in autoimmune hypothyroidism and improves during the first six months of levothyroxine therapy. PLoS ONE 11(6):e0156925
Tan NC, Chew RQ, Subramanian RC, Sankari U, Koh YLE, Cho LW (2019) Patients on levothyroxine replacement in the community: association between hypothyroidism symptoms, co-morbidities and their quality of life. Fam Pract 36(3):269–275
Samuels MH, Kolobova I, Niederhausen M, Janowsky JS, Schuff KG (2018) Effects of altering levothyroxine (l-t4) doses on quality of life, mood, and cognition in l-t4 treated subjects. J Clin Endocrinol Metab 103(5):1997–2008
Wolters TLC, Roerink S, Sterenborg R, Wagenmakers M, Husson O, Smit JWA et al (2020) The effect of treatment on quality of life in patients with acromegaly: a prospective study. Eur J Endocrinol 182(3):319–331
Funding
This work was conducted with support from The Endocrine Society Acromegaly Clinical Research Fellowship Award; NIH Grants T32 DK007028, K24 HL092902, K23DK115903, and K23 DK113220; and the Harvard Catalyst/The Harvard Clinical and Translational Science Center (Grants 1UL1TR001102, 8 UL1 TR000170 from the National Center for Advancing Translational Science, and 1 UL1 RR025758 from the National Center for Research Resources). Pfizer provided growth hormone for a randomized controlled trial from which baseline data for this study were obtained for a subset of subjects.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AK, LED, and KKM. The first draft of the manuscript was written by AK and all authors made comments on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
LED has received drug donation from Pfizer for an investigator-initiated study. WWW has participated as a clinical trial investigator for Chiasma. LBN has received grant support/investigator funding from Ipsen and Chiasma and serves as a consultant on an advisory board for Pfizer and Chiasma. BS has equity in Pfizer and Amgen. UBK served as a consultant on advisory boards for Novo Nordisk and Acerus. KKM has received grant support for investigator-initiated studies from Amgen and drug donation from Pfizer for an investigated-initiated study and has equity in GE, Bristol-Myers Squibb, Becton Dickinson, and Boston Scientific. The other authors have no conflicts of interest to disclose.
Ethical approval
Approval was obtained from the Massachusetts General Hospital Institutional Review Board. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kimball, A., Dichtel, L.E., Yuen, K.C.J. et al. Quality of life after long-term biochemical control of acromegaly. Pituitary 25, 531–539 (2022). https://doi.org/10.1007/s11102-022-01224-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-022-01224-0